Abstract
Purpose
To examine long-term recurrence and anal continence of patients with anal fistula treated by fistulectomy and endorectal advancement flap repair.
Method
Retrospective analysis of a prospective cohort of 115 patients (77.4% males, mean age 48.9 years) requiring 130 procedures, with a minimum follow-up of 10 years. Recurrence included reappearance of fistula after wound healing or presence of an abscess or chronic suppuration in the operated area at follow-up. Fecal incontinence was evaluated by the Cleveland Clinic Florida (CCF-FI) fecal incontinence scoring system.
Results
The mean and SD duration of the follow-up period was 155.5 (21.7) months. Recurrence developed in 31 (23.8%) cases, 28 (90.3%) of which within the first year, with a mean time to recurrence of 4.9 (2.9) months. The success rate was 76.2%. Anal continence was normal in 80% of patients before surgery, 63.8% at 1-year follow-up, and 71.5% at the end of follow-up (p < 0.001). Overall, continence worsened in 16.9% of cases. The mean (95% CI) CCF-FI score was 0.78 (0.35–1.21) preoperatively, 1.04 (0.64–1.43) at 1 year after surgery, 0.90 (0.52–1.29) at 5 years, and 1.16 (0.66–1.67) at the end of the study (p < 0.05). Neither recurrence nor continence was significantly associated with previous anal or fistula surgical procedures or complexity of the fistula.
Conclusion
In this study, fistulectomy and endorectal advancement flap repair was associated with a long-term high rate of success. Most recurrences occurred within the first year and continence showed a mild deterioration over time.
Clinical trial registration: Not applicable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fistula-in-ano is an abnormal epithelial-lined tract connecting the anal canal to the perianal skin, which usually arises from an infected anal crypt representing the chronic state of anal suppuration. Anal fistula is one of the most common proctological disease. In a recent real-world study, the standardized prevalence of anal fistula in Europe and the UK, with and without Crohn’s disease, was 1.80 and 1.83 per 100,000 patients, respectively [1]. Surgery is the treatment of choice, but despite a variety of surgical techniques, the management of anal fistula can be complicated and remains a source of concern for patients and surgeons [2, 3]. The goal of treatment is to achieve healing without sphincter damage and consequent continence disturbance. The management of complex fistulas using different surgical procedures [4,5,6] poses an increased risk for recurrence and incontinence [3, 6, 7] and is technically challenging [6, 8, 9].
The advancement flap procedure is an option in the treatment of patients with fistulas of different etiologies, such as cryptoglandular, trauma, obstetrical, or inflammatory bowel disease. Fistulectomy and endorectal advancement flap repair is a sphincter-sparing and well-established technique, which has been shown to be safe and effective for treating anal fistulas that could not be treated by simple procedures [6, 7, 9,10,11]. However, results of endorectal advancement flap repair published in the literature are mostly based on small and heterogeneous series of patients with variable lengths of follow-up usually shorter than 24 months. Data on long-term outcomes is scare and inconsistent. As far as we are aware, very long-term data of a large series of patients with anal fistula undergoing fistulectomy and endorectal advancement flap repair have not been previously reported. The present study was designed to assess the recurrence rate and functional outcome of fistulectomy and endorectal advancement flap repair in the treatment of anal fistula after a follow-up of at least 10 years.
Method
This was a retrospective analysis of a prospective cohort study conducted in a colorectal surgery unit of a tertiary care hospital in Pamplona, Navarra (Spain). Between January 2001 and December 2006, all consecutive patients diagnosed with anal fistula of cryptoglandular origin undergoing fistulectomy and endorectal advancement flap repair were included in the study provided that they were aware of the purpose of the study and signed the informed consent. The primary objective of the study was to assess recurrence of the fistula and changes in continence in the long term. Patients diagnosed with inflammatory bowel disease before surgery or at follow-up were excluded from the study due to special characteristics of perianal disease in these patients, as were those patients with previous radiation therapy in the pelvic region, history of rectal surgery for colorectal cancer, rectovaginal fistulas, or those referred from elsewhere. Patients with difficulties of knowing previous diagnostic studies and surgical techniques reliably, and not being able to ensure adequate long-term follow-up, were also excluded. The study was approved by the institutional review board and all patients gave written informed consent.
Before operation, every patient underwent a digital examination, proctosigmoidoscopy, and rectal endosonography. The anatomical location of fistulas was described according to the classification of Parks et al. [12]. Patients underwent fistulectomy and endorectal advancement flap repair as previously described [13] with operations performed on a short-stay basis, under spinal anesthesia and in the lithotomy or jack-knife position. The main fistulous tract and any secondary tracts were dissected, a small elliptical incision around the internal opening was made, and the fistula tract was excised. The internal opening was sutured with interrupted 4/0 polyglactin sutures (Ethicon Endosurgery, Madrid, Spain). A curvilinear (semicircular) endorectal advancement flap of partial thickness was raised immediately above the internal opening and mobilized 4 ± 6 cm proximally. The base of the flap was approximately twice the width of its apex. The flap was advanced and sutured (also with 4/0 polyglactin) to the level of the intersphincteric line. The external wound was left open for drainage and packed loosely.
Patients were advised to contact the surgical staff if any symptoms appeared during the intervals between scheduled visits. Patients were followed at the outpatient clinics at 3-month intervals during the first year after surgery, and all of them were visited again at the outpatient clinics at 5 years. In December 2016 after a minimum follow-up of 10 years, the medical records were reviewed and patients were contacted by phone to assess their clinical status; in case of changes in continence as compared with previous data or presence of symptoms suggestive of recurrence, patients were appointed for a medical visit.
Recurrence was defined as the presence of an abscess or chronic suppuration arising in the same area after wound healing or by obvious evidence of fistulation at any time during follow-up. The degree of incontinence was evaluated according to the Cleveland Clinic Florida fecal incontinence (CCF-FI) scoring system [14]. The continence score takes into account the type of incontinence (solid, liquid, gas, wears pad, lifestyle alteration) and frequency (scored from 0 = never; 1 = rarely [< 1/month], 2 = sometimes [< 1 week, > 1 month]; 3 = usually [< 1 day, ≥ 1 week]; 4 = always [≥ 1 day]) and ranges from 0 (perfect) to 20 (complete incontinence). In this study, continence was defined as score 0 and incontinence as ≥ 1 point on this scale.
Statistical analysis
Categorical variables are expressed as frequencies and percentages and continuous variables as mean and standard deviation (SD). The chi-square test and the Wilcoxon signed-rank test were used for the comparison of categorical and quantitative data, respectively. The cumulative incidence of recurrence was assessed with the Kaplan-Meier method. Statistical significance was set at p < 0.05. The Statistical Package for the Social Sciences (SPSS) version 25 (IBM Statistics, Chicago, IL, USA) was used for the analysis of data.
Results
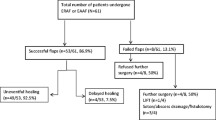
Of a total of 363 patients with anal fistula who were operated on as part of their treatment during the study period, 230 underwent different procedures, such as fistulotomy, fistulectomy, advancement flap, seton placement, or fibrin glue fixation, and were excluded. The study population included the remaining 133 (36.6%) patients, who underwent fistulectomy and endorectal advancement flap repair. Eighteen patients (8.3%) were lost at follow-up, and 15 required a second advancement flap repair. Therefore, the study population included 115 patients (77.4% males, mean age 48.9 years) who underwent a total of 130 surgical procedures and completed a minimum follow-up of 10 years, with a mean (SD) of 155.5 (21.7) months. Salient clinical characteristics are shown in Table 1. History of anal surgery was recorded in 73.8% of the cases due to an anal fistula in 40.6% and an abscess in 36.1%. Trans-sphincteric fistulas were the most common (88.5%) (low 30.4%, medium 53.0%). Suprasphincteric fistulas occurred in 10% of patients and extrasphincteric in 1.5%.
During the follow-up period, 31 recurrences were documented, with a recurrence rate of 23.8%. In 28 cases (90.3%), recurrences occurred within the first year after surgery, and a second endorectal flap advancement repair was performed in 15 (53.6%) patients. The remaining three cases of recurrence occurred after the first follow-up year, at 19, 30, and 72 months, respectively. The overall success rate was 76.2%. The cumulative recurrence incidence at follow-up is shown in Fig. 1. There was a trend towards recurrence in patients with history of anal surgery (p = 0.054), but statistically significant differences in the recurrence rate according to previous surgical procedures for the presence of an anal fistula (p = 0.493) or complexity of the fistula (p = 0.671) were not observed (Fig. 2).
Of the 130 procedures, preoperative continence was normal in 104 cases (80%) and impaired in the remaining 26 cases. After the first year of surgery, continence worsened in 20.2% (21/104) cases, and at the end of follow-up, continence disturbance was recorded in 10.5% (11/104) cases. Overall, there was a worsening of continence in 16.9% (22/130) cases. The mean (95% CI) CCF-FI score was 0.78 (0.35–1.21) preoperatively, 1.04 (0.64–1.43) at 1 year after surgery, 0.90 (0.52–1.29) at 5 years, and 1.16 (0.66–1.67) at the end of the study (p < 0.05). Continence disturbance was unrelated to previous anal or fistula surgical procedures or complexity of fistula.
Discussion
The technique of fistulectomy with the advancement of rectal flap to repair the primary defect meets the goal of surgical treatment of anal fistula, which is to cure the disease without affecting fecal continence. This procedure is especially indicated in the management of complex fistulas [10, 11, 13] even in patients who had undergone previous seton insertion [15]. However, most series of endorectal advancement flap repair published in the literature are small and heterogeneous, or have included patients with fistulas of cryptoglandular origin as well as fistulas of other causes.
The success rates and the incidence of continence disturbance reported in the literature are about 80.8% and 13.3%, respectively [4]. In a recent systematic review and meta-analysis of 30 studies comprising 797 patients treated with the endorectal advancement flap, the overall success was 74.6% with 25.6% recurrence rate but lower incontinence rate of 7.8% [16]. On the other hand, the average follow-up of patients in these series is 28.9 months [4], with only three studies with mean duration of follow-up longer than 60 months (range 67–72 months) [8, 16,17,18]. In 41 patients with high fistulas reported by van der Hagen et al. [8], a high recurrence rate of 63% was found after a follow-up of 6 years, whereas in the study of Jarrar et al. [10] of 75 patients with complex fistula disease, primary healing occurred in 72% of patients after a mean follow-up of 7 years. Moreover, study populations are small, with data of more than 100 patients (range 103–189 patients) analyzed in only four studies [13, 19,20,21]. In order to identify predictive variables of failure of the endorectal advancement flap repair in high trans-sphincteric fistulas, van Onkelen et al. [22], in 2014, reported a series of 252 patients with a 3-year success rate of 59% (mean follow-up 21 months). In the present study of 130 fistulectomies and advanced flap repair performed in 115 patients diagnosed with cryptoglandular fistulas, with a prolonged follow-up (mean 155.5 months), the success rate was 76.2% with an overall worsening of continence of 16.9%, which are consistent with mean rates published in the literature [4].
In 2000, van der Hagen et al. [8] reported after a mean follow-up of 72 months that success rates of fistulectomy with endorectal advancement flap repair may decrease over time, from 78% at 12 months up to 37% at 48 months of follow-up. In contrast, the previous experience of our group showed that no recurrences occurred after 1 year [23]. This study included a series of 91 patients treated between January 2001 and June 2004, with a mean follow-up of 42 months. In the present study after extending the follow-up, only three recurrences (3/31, 9.7%) were diagnosed from the first year of follow-up, and all of them occurred in patients included in the cohort after 2004, so that the success rate of the surgical technique in our series only decreased from 78.4% at 12 months to 76.2% at 72 months of follow-up.
In our study, like others [6, 22, 24], a statistically significant relationship between recurrence and history of surgery for previous perianal fistula was not found. However, in other series of patients, failure rate was influenced by previous fistula repairs, but in the study of Ozuner et al. [17] of 106 advancement flap repairs, Crohn’s disease was the cause of fistulas in 30% of the cases, and in the series of 68 patients reported by Ellis and Clark [25], history of previous repairs was present in 40% of them. In 44 patients undergoing transanal advancement flap repair, Schouten et al. [26] found that the success rate of 75% dropped to 50% in patients with two or more previous repairs.
In relation to continence, and in contrast to the study of Mizrahi et al. [6] in which continence deterioration was a more common finding in patients who had undergone previous surgical repairs, a mild significant continence deterioration was found in our study, although it was independent of history of anal surgery, previous surgical repairs, or complexity of fistula. A few studies have compared pre- and postoperative continence. We found that among patients with normal continence before surgery, disturbed continence occurred in 10.5% (11/104) of cases after operation, which is a percentage lower than 26% (7/27) reported in the series of van der Hagen et al. [8] and 19.6% (10/51) in the study of Uribe et al. [24], but similar to 9.5% (2/21) found by Perez et al. [7].
The present study includes only patients with anal fistula of cryptoglandular etiology undergoing fistulectomy and endorectal advancement flap repair but limitations include the retrospective design and the single-center characteristics. However, the mean follow-up of patients to assess recurrence and continence disturbances after fistulectomy and advancement flap is the longest reported so far.
Conclusion
In this study, the success rate of fistulectomy and endorectal advancement flap repair for treating cryptoglandular anal fistula is high and recurrences occur mostly within the first year after surgery. Therefore, prolonged follow-up periods do not appear to be necessary. There was a mild deterioration of continence along the years independently of previous anal surgical procedures or complexity of the anal fistula.
References
Hokkanen SR, Boxall N, Khalid JM, Bennett D, Patel H (2019) Prevalence of anal fistula in the United Kingdom. World J Clin Cases 7:1795–1804. https://doi.org/10.12998/wjcc.v7.i14.1795
Malik AI, Nelson RL (2008) Surgical management of anal fistulae: a systematic review. Colorectal Dis 10:420–430. https://doi.org/10.1111/j.1463-1318.2008.01483.x
Jacob TJ, Perakath B, Keighley MR (2010) Surgical intervention for anorectal fistula. Cochrane Database Syst Rev 5:CD006319. https://doi.org/10.1002/14651858.CD006319.pub2
Soltani A, Kaiser AM (2010) Endorectal advancement flap for cryptoglandular or Crohn's fistula-in-ano. Dis Colon Rectum 53:486–495. https://doi.org/10.1007/DCR.0b013e3181ce8b01
Kronborg O (1985) To lay open or excise a fistula-in-ano: a randomized trial. Br J Surg 172:970. https://doi.org/10.1002/bjs.1800721211
Mizrahi N, Wexner SD, Zmora O, Da Silva G, Efron J, Weiss EG, Vernava AM 3rd, Nogueras JJ (2002) Endorectal advancement flap: are there predictors of failure? Dis Colon Rectum 45:1616–1621. https://doi.org/10.1097/01.DCR.0000037654.01119.CD
Perez F, Arroyo A, Serrano P, Sánchez A, Candela F, Perez MT, Calpena R (2006) Randomized clinical and manometric study of advancement flap versus fistulotomy with sphincter reconstruction in the management of complex fistula-in-ano. Am J Surg 192:34–40. https://doi.org/10.1016/j.amjsurg.2006.01.028
van der Hagen SJ, Baeten CG, Soeters PB, van Gemert WG (2006) Long-term outcome following mucosal advancement flap for high perianal fistulas and fistulotomy for low perianal fistulas: recurrent perianal fistulas: failure of treatment or recurrent patient disease? Int J Colorectal Dis 21:784–790. https://doi.org/10.1007/s00384-005-0072-7
Mitalas LE, Gosselink MP, Oom DM, Zimmerman DD, Schouten WR (2009) Required length of follow-up after transanal advancement flap repair of high transsphincteric fistulas. Colorectal Dis 11:726–728. https://doi.org/10.1111/j.1463-1318.2008.01666.x
Jarrar A, Church J (2011) Advancement flap repair: a good option for complex anorectal fistulas. Dis Colon Rectum 54:1537–1541. https://doi.org/10.1097/DCR.0b013e31822d7ddd
Lee CL, Lu J, Lim TZ, Koh FH, Lieske B, Cheong WK, Tan KK (2015) Long-term outcome following advancement flaps for high anal fistulas in an Asian population: a single institution's experience. Int J Colorectal Dis 30:409–412. https://doi.org/10.1007/s00384-014-2100-y
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano. Br J Surg 63:1–12. https://doi.org/10.1002/bjs.1800630102
Ortíz H, Marzo J (2000) Endorectal flap advancement repair and fistulectomy for high trans-sphincteric and suprasphincteric fistulas. Br J Surg 87:1680–1683. https://doi.org/10.1046/j.1365-2168.2000.01582.x
Jorge JM (1993) Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97. https://doi.org/10.1007/BF02050307
Tan KK, Alsuwaigh R, Tan AM, Tan IJ, Liu X, Koh DC, Tsang CB (2012) To LIFT or to flap? Which surgery to perform following seton insertion for high anal fistula? Dis Colon Rectum 55:1273–1277. https://doi.org/10.1097/DCR.0b013e31826dbff0
Stellingwerf ME, van Praag EM, Tozer PJ, Bemelman WA, Buskens CJ (2019) Systematic review and meta-analysis of endorectal advancement flap and ligation of the intersphincteric fistula tract for cryptoglandular and Crohn's high perianal fistulas. BJS Open 21:231–241. https://doi.org/10.1002/bjs5.50129
Ozuner G, Hull TL, Cartmill J, Fazio VW (1996) Long-term analysis of the use of transanal rectal advancement flaps for complicated anorectal/vaginal fistulas. Dis Colon Rectum 39:10–14. https://doi.org/10.1007/BF02048261
van Koperen PJ, Wind J, Bemelman WA, Bakx R, Reitsma JB, Slors JF (2008) Long-term functional outcome and risk factors for recurrence after surgical treatment for low and high perianal fistulas of cryptoglandular origin. Dis Colon Rectum 51:1475–1481. https://doi.org/10.1007/s10350-008-9354-9
Aguilar PS, Plasencia G, Hardy TG Jr, Hartmann RF, Stewart WR (1985) Mucosal advancement in the treatment of anal fistula. Dis Colon Rectum 28:496–498. https://doi.org/10.1007/BF02554093
Golub RW, Wise WE Jr, Kerner BA, Khanduja KS, Aguilar PS (1997) Endorectal mucosal advancement flap: the preferred method for complex cryptoglandular fistula-in-ano. J Gastrointest Surg 1:487–491. https://doi.org/10.1016/s1091-255x(97)80138-2
Zimmerman DD, Delemarre JB, Gosselink MP, Hop WC, Briel JW, Schouten WR (2003) Smoking affects the outcome of transanal mucosal advancement flap repair of trans-sphincteric fistulas. Br J Surg 90:351–354. https://doi.org/10.1002/bjs.4044
van Onkelen RS, Gosselink MP, van Rosmalen J, Thijsse S, Schouten WR (2014) Different characteristics of high and low transsphincteric fistulae. Colorectal Dis 16:471–475. https://doi.org/10.1111/codi.12578
Ortiz H, Marzo M, de Miguel M, Ciga MA, Oteiza F, Armendariz P (2008) Length of follow-up after fistulotomy and fistulectomy associated with endorectal advancement flap repair for fistula in ano. Br J Surg 95:484–487. https://doi.org/10.1002/bjs.6023
Uribe N, Millán M, Minguez M, Ballester C, Asencio F, Sanchiz V, Esclapez P, del Castillo JR (2007) Clinical and manometric results of endorectal advancement flaps for complex anal fistula. Int J Colorectal Dis 22:259–264. https://doi.org/10.1007/s00384-006-0172-z
Ellis CN, Clark S (2007) Effect of tobacco smoking on advancement flap repair of complex anal fistulas. Dis Colon Rectum 50:459–463. https://doi.org/10.1007/s10350-006-0829-2
Schouten WR, Zimmerman DD, Briel JW (1999) Transanal advancement flap repair of transsphincteric fistulas. Dis Colon Rectum 42:1419–1422. https://doi.org/10.1007/BF02235039
Acknowledgements
The authors thank Dr Marta Pulido for editing the manuscript and editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval statement
The study was approved by the Institutional Review Board of Complejo Hospitalario de Navarra, Spain.
Patient consent statement
Written informed consent was obtained from all participants.
Permission to reproduce material from other sources
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chaveli Diaz, C., Esquiroz Lizaur, I., Marzo Virto, J. et al. Fistulectomy and endorectal advancement flap repair for cryptoglandular anal fistula: recurrence and functional outcome over 10 years of follow-up. Int J Colorectal Dis 36, 841–846 (2021). https://doi.org/10.1007/s00384-021-03867-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03867-0