Abstract
Introduction
Endoscopic migration of plastic biliary stents is performed by endoscopic retrograde cholangiopancreatography (ERCP) for biliary and pancreatic diseases. This plays an increasingly important role. Intestinal perforation caused by stent migration is one of the complications. Although sigmoid colon perforation caused by stent migration is rare, it can be life-threatening. This case shows us that we should increase awareness of sudden abdominal pain after ERCP.
Method
We provide a review of the clinical manifestations, imaging data of this case, and the literature related to the perforation caused by stent migration.
Results
A male patient had a history of choledocholithiasis, cholecystolithiasis, and biliary pancreatitis treated with ERCP and a pancreatic stent. After the operation, the patient developed cholangitis and was treated with ERCP and a plastic biliary stent. This patient was admitted to the emergency department with sudden lower abdominal pain. A CT scan showed sigmoid colon perforation by a foreign body and infra-diaphragmatic free air. An emergency surgery confirmed that the stent had caused the perforation. The patient was then treated with sigmoid colectomy and sigmoidostomy.
Discussion
Biliary stent migration after ERCP is rare, but intestinal perforation caused by migration should be considered in cases of abdominal pain of unknown cause.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case presentation
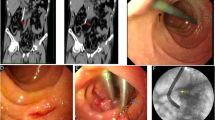
A 54-year-old male patient presented at the hospital with right upper abdominal pain and shivering. A physical examination showed jaundice and right upper abdominal tenderness with muscular tension. An auxiliary B-ultrasound showed gallstones and choledochectasis. A CT showed acute pancreatitis choledochectasis and cholecystolithiasis. Amylase was 3254.00 μ/L, T-Bil was 90.8 μmol/L, and D-Bil was 66.3 μmol/L. The patient was treated with emergency endoscopic retrograde cholangiopancreatography (ERCP) along with sphincterotomy of duodenal papilla, choledocholithotomy, pancreatic stent, and nasobiliary drainage. During the operation, congestion of duodenal papilla, bile sludge, and choledocholithiasis were observed. After operation, jaundice decreased slowly, and the patient began to experience shivering and high fever. Residual stones were evaluated by radiography. Then ERCP was performed, and a plastic biliary stent was placed. During the operation, the common bile duct was visibly dilated, with a maximum diameter of about 1.3 cm. Jaundice decreased, and the patient recovered after the operation, and the jaundice had completely disappeared by the time the patient was discharged. Three months later, the patient complained of progressive aggravation of lower abdominal pain. In the outpatient department, a subsequent CT scan of the abdomen revealed sigmoid colon perforation by a foreign body (Figs. 1, 2, 3, 4, and 5) and infra-diaphragmatic free air. An emergency surgery confirmed that the stent had caused the perforation, and the patient was treated with sigmoid colectomy + sigmoidostomy. Pathology revealed inflammatory ulcer with perforation. After an uncomplicated recovery period, the patient was discharged on the tenth postoperative day.
Discussion
ERCP has gradually become one of the most important methods for the clinical treatment of cholelithiasis, cholangitis, obstructive jaundice, and similar conditions. Endoscopic retrograde biliary drainage (ERBD) has become more important in the treatment of benign stricture of the bile duct. The average patency period is about 3–6 months, and the migration rate is 5–10% [1]. After migration, perforation is rare. However, plastic stents fall off more easily than metal stents; most of plastic stents can be removed through anus. Rarely, the migration of biliary stents leads to perforation of the sigmoid colon, but once it occurs, it can be life-threatening. The risk factors include diverticulum, adhesion, hernia, straight stent, and stent length greater than 7 cm.
According to the literature review, 26 related cases have been reported [2,3,4,5,6,7,8], including 4 cases of incarceration, 22 cases of perforation, and 20 cases with sigmoid colon diverticulum. All of the reported works described a plastic stent that had migrated. The earliest time of migration was 2 weeks after placement, and the latest was 6 months. Most of the clinical manifestations were paroxysmal lower abdominal pain. The main diagnostic methods were history and abdominal CT. Treatment measures included the following: 1 case treated was with endoscopy, 1 case declined treatment, and the rest were all treated with emergency surgery. The operations included perforation resection, distal closure, and sigmoidostomy. The patient who decided not to undergo treatment died, but the rest were cured and discharged from the hospital, and a second-stage return operation was performed later.
References
ERCP Group, Chinese Society of Digestive Endoscopology;Biliopancreatic group, Chinese Association of Gastroenterologist Hepatologist; National Clinical Research Center for Digestive Diseases (2018) Diagnosis and treatment guidelines for ERCP in China (2018). Chinese Journal of Practical Internal Medicine 35(11):777–813. https://doi.org/10.19538/j.nk2018110167
Konstantinidis C, Varsos P, Kympouris S et al (2014) Migrated biliary plastic stent causing double sigmoid colon perforation. J Surg Case Rep 2014(12). https://doi.org/10.1093/jscr/rju134
Siaperas P, Argyrios et al (2017) A rare cause for Hartmann’s procedure due to biliary stent migration: a case report. Int J Surg Case Rep 31:83–85. https://doi.org/10.1016/j.ijscr.2017.01.016
Riccardi M, Deters K, Jabbar F (2019) Sigmoid diverticulitis and perforation secondary to biliary stent migration. Case Rep Surg 2019:1–3. https://doi.org/10.1155/2019/2549170
Virgilio E, Pascarella G, Scandavini CM et al (2015) Colonic perforations caused by migrated plastic biliary stents. Korean J Radiol 16(2):444–445. https://doi.org/10.3348/kjr.2015.16.2.444
Chittleborough TJ, Mgaieth S, Kirkby B et al (2014) Remove the migrated stent: sigmoid colon perforation from migrated biliary stent. ANZ J Surg 86(11):47–948. https://doi.org/10.1111/ans.12796
Konstantinidis C, Varsos P, Kympouris S et al (2014) Migrated biliary plastic stent causing double sigmoid colon perforation. J Surg Case Rep 2014(12):1–2. https://doi.org/10.1093/jscr/rju134
Bagul A, Pollard C, Dennison AR (2010) A review of problems following insertion of biliary stents illustrated by an unusual complication. Ann R Coll Surg Engl 92(4):e27–e31. https://doi.org/10.1308/147870810x12659688852239
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tao, Y., Long, J. Sigmoid colon perforation caused by migrated plastic biliary stents: a case report. Int J Colorectal Dis 36, 199–201 (2021). https://doi.org/10.1007/s00384-020-03728-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03728-2