Abstract
Purpose
The aim of this study was to analyze clinical outcomes after surgical and/or conservative management of patients with colonic diverticulitis.
Material and methods
Between January 2001 and November 2018, data for 1175 patients (right (Rt.) side: n = 1037, left (Lt.) side: n = 138) who underwent conservative management (n = 987) and surgical management (n = 188) for colonic diverticulitis were retrieved from a retrospective database. The Rt. sided was defined up to the proximal two-thirds of the transverse colon and Lt. sided was defined from the distal one-third of the transverse colon.
Results
The overall incidence of colonic diverticulitis is gradually increasing. The mean age of all patients was 43.2 ± 17 and was significantly higher in patients with Lt.-sided (57.0 ± 15.7) than with Rt.-sided (41.4 ± 13.4) diverticulitis (p = 0.001). The most common lesion site was cecum (71.7%, n = 843). First-time attacks were the most common (91.0%, n = 1069). The surgical rate was 12.2% on the right. sided and 44.9% on the left sided (p < 0.005). The mean age, age distribution, BMI, open surgery rate, stoma formation rate, and Hinchey types III and IV rate were significantly higher in Lt. sided than in Rt. sided (p < 0.005). Older age, higher BMI (≥ 25), and Hinchey types III and IV were significantly associated with surgical risk factors of diverticulitis (p < 0.005).
Conclusion
Base on present study, Lt.-sided colonic diverticulitis tends to be more severe than Rt. sided, and surgery is more often required. In addition, colonic diverticulitis that requires surgery seems to be older and more obese on Lt. sided.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colonic diverticulosis refers to a small outpouching of the intestinal wall. It is classified histologically as a true diverticulum when all layers of the bowel wall protrude or as a false diverticulum when only the mucosal and submucosal layers protrude through the muscular layer [1]. Colonic diverticulosis is common in the Western population and is mainly present in the sigmoid colon, whereas it is less common in Asian populations, including South Koreans, and is mainly present in the right-sided colon [2,3,4]. Although colonic diverticulosis is usually asymptomatic, 10–20% of colonic diverticulosis can develop into colonic diverticulitis [5].
Recently, the prevalence of colonic diverticulosis has been increasing in South Korea, as has the incidence of colonic diverticulitis since the 1990s [2, 6]. Uncomplicated colonic diverticulitis can be treated with nonsurgical management (conservative management and antibiotic therapy), whereas complicated colonic diverticulitis that includes perforation, abscess, purulent or feculent peritonitis, fistula, stricture, and obstruction may sometimes require surgical treatment [7, 8]. The aim of the present study was to analyze the clinical characteristics and outcomes after surgical and/or conservative management in South Korean patients with acute colonic diverticulitis.
Material and methods
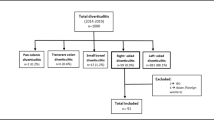
Between January 2001 and November 2018, 1175 patients who underwent management after admission to two South Korean hospitals (Severance Hospital and Sooncheonhyang Bucheon Hospital) were identified from a retrospective database. The patients with small bowel diverticulitis, with colonic diverticulitis with bleeding, and with malignancy were excluded from the present study. Of the remaining patients, 987 had undergone conservative management, including percutaneous drain catheter insertion for abscess drainage after admission, and 188 patients had undergone surgical management. All data for clinical and pathological features were reviewed retrospectively. All patients underwent abdominal pelvic CT scans and, occasionally, colonoscopy, biopsy, and abdomen ultrasound. Complicated colonic diverticulitis was defined as attacks that included obstruction, fistula, abscess, and free perforation causing either purulent or feculent peritonitis. Colonic diverticulitis found in the cecum, the ascending colon, and the hepatic flexure was classified as right sided, whereas diverticulitis found in the splenic flexure, the descending colon, and the sigmoid colon was classified as left sided. Conservative management included intravenous broad-spectrum antibiotic therapy for 1–2 weeks, with no food by mouth and fluid support and/or interventional catheter insertion for abscess drainage. Patients received follow-up and were recorded on a database until death or until May 2019.
Statistical analysis
All statistical analyses were performed using SAS Version 9.1.3 (SAS Institute Inc., Cary, NC) and SPSS software, Version 24.0 (SPSS, Chicago, IL). Categorical variables were analyzed using the χ2 or Fisher’s exact test, and continuous variables were analyzed using Student’s t test/Mann-Whitney U rank tests. The association between the risk factors and colonic diverticulitis surgery was analyzed using unconditional logistic regression models. p values less than 0.05 were considered statistically significant.
Results
Characteristics of patients with colonic diverticulitis
The mean age of all patients in the present study was 43.2 ± 17.9 years. The study population included 679 (57.8) males and 496 (42.2%) females with a mean weight of 65.6 ± 12.8 kg, mean height of 165.8 ± 8.7 cm, and mean body mass index (BMI) of 23.8 ± 3.6 kg/m2. The patient characteristics were analyzed by comparing the conservative management (n = 987) and surgical management (n = 188) groups (Table 1). The mean age was significantly higher in the surgical management group than in the conservative management group (47.8 ± 17.9 vs. 42.3 ± 13.6 years, p < 0.005). The sex ratio, height, weight, and BMI did not differ significantly between the two groups. Patient characteristics were also analyzed by comparing right-sided (n = 1037) versus left-sided (n = 138) diverticulitis (Table 2). The mean age was significantly higher in patients with left-sided (57.0 ± 15.7 years) than with right-sided (41.4 ± 13.4 years, p = 0.001) diverticulitis. The BMI was significantly higher in patients with left-sided (24.5 ± 4.2 kg/m2) than with right-sided (23.7 ± 3.6, p = 0.021) diverticulitis (Table 2).
Incidence of colonic diverticulitis
The overall incidence of colonic diverticulitis increased gradually during the present study. The yearly incidence of hospitalized colonic diverticulitis patients and the numbers of patients in the conservative management group gradually increased, whereas the numbers of patients in the surgical management group were relatively steady (Fig. 1a). The numbers of patients with right-sided colonic diverticulitis gradually increased and the numbers of patients with left-sided colonic diverticulitis were relatively steady (Fig. 1b).
Age distribution
Patients in the conservative management group showed a bell-shaped age distribution, while patients in the surgical management group showed an even ranking (p < 0.005). The most common age distribution was the 3rd decade (31~40 years: 27.3%, n = 269) and 4th decade (41~50 years: 26.4%, n = 261) for the conservative management group, whereas the age distribution showed an even spread in the surgical management group, as follows: 2nd (21~30 years: 13.8%, n = 26), 3rd (31~40 years: 17.0%, n = 32), 4th (41~50 years: 20.2%, n = 38), 5th (51~60 years: 15.9%, n = 31), 6th (61~70 years: 15.4%, n = 29), 7th (71~80 years: 8.0%, n = 15), and > 8th (n = 6, 3.2) decades (Fig. 2a).
Comparison of the right-sided and left-sided colonic diverticulitis revealed the most common age distributions as the following: 3rd (31~40 years: 27.6%, n = 286) and 4th (41~50 years: 26.2%, n = 272) decades for right-sided colonic diverticulitis, and 5th (51~60 years: 21.7%, n = 30) and 4th (41~50 years: 21.7%, n = 30) decades for left-sided colonic diverticulitis (p < 0.005) (Fig. 2b).
The most common age distribution in patients in the conservative management group with right-sided colonic diverticulitis was the 3rd (31~40 years: 28.3%, n = 257) and 4th (41~50 years: 27.0%, n = 246) decades. For left-sided colonic diverticulitis, the most common age distribution was the 5th (51~60 years: 30.3%, n = 23) and 4th (41~50 years: 23.7%, n = 18) decades (p < 0.005) (Fig. 2c). The most common age distribution in patients in the surgical management group with right-sided colonic diverticulitis was the 3rd (31~40 years: 23.0%, n = 29) and 4th (41~50 years: 23.0%, n = 29) decades. For left-sided colonic diverticulitis, the most common age distribution was the 6th (61~70 years: 30.6%, n = 19) and 7th (71~80 years: 16.1%, n = 10) decades (p < 0.005) (Fig. 2d).
Distribution of lesions
Overall, 88.3% (n = 1037) of the patients had right-sided diverticulitis and 11.7% (n = 138) had left-sided diverticulitis (Table 1). The occurrence of right-sided diverticulitis was statistically more common than left-sided diverticulitis (p < 0.005). In all colonic diverticulitis, the distribution of lesions in right-sided colonic diverticulitis was 71.7% (n = 843) in the cecum, 7.7% (n = 90) in the ascending colon, and 8.6% (n = 104) in the hepatic flexure. The cecum was the most common site of lesions in right-sided colonic diverticulitis. In all colonic diverticulitis, distribution of lesions in left-sided colonic diverticulitis was 8.3% (n = 97) in the sigmoid colon, 3.4% (n = 40) in the descending colon, and 0.1% (n = 1) in the splenic flexure. The conservative management group had 92.3% (n = 911) right-sided and 7.7% (n = 76) left-sided colonic diverticulitis, with the following lesion distributions: 71.7% (n = 843) in the cecum, 7.7% (n = 90) in the ascending colon, and 8.6% (n = 104) in the hepatic flexure for right-sided diverticulitis and 4.7% (n = 46) in the sigmoid colon, 2.9% (n = 29) in the descending colon, and 0.1% (n = 1) in the splenic flexure for left-sided diverticulitis. The surgical management group had 67.0% (n = 126) right-sided and 33.0% (n = 62) left-sided cases of colonic diverticulitis, with the following lesion distributions: 59.0% (n = 111) in the cecum, 5.9% (n = 11) in the ascending colon, and 2.1% (n = 4) in the hepatic flexure for right-sided diverticulitis and 27.1% (n = 51) in the sigmoid colon, 5.9% (n = 11) in the descending colon, and 0% (n = 0) in the splenic flexure for left-sided diverticulitis.
Number of attacks
The most common number of attacks in the patient population was one (91.0%, n = 1069), followed by two (6.6%, n = 77), three (2.0%, n = 24), four (0.3%, n = 4), and five (0.1%, n = 1) (Table 1). The conservative management group had the following attack incidence: one (91.9%, n = 907), two (6.0%, n = 59), three (1.7%, n = 17), four (0.3%, n = 3), and five (0.1%, n = 1). The surgical management group had the following attack incidence: one (85.6%, n = 161), two (9.0%, n = 17), three (3.7%, n = 7), four (0.5%, n = 1), and five (0%, n = 0) (p = 0.136). The attack incidence for right-sided colonic diverticulitis was as follows: one (91.9%, n = 957), two (6.0%, n = 62), three (1.7%, n = 18), four (0.3%, n = 3), and five (0.1%, n = 1). The attack incidence for left-sided colonic diverticulitis was as follows: one (84.3%, n = 113), two (10.4%, n = 14), three (4.6%, n = 6), four (0.7%, n = 1), and five (0%, n = 0) (p = 0.047) (Table 2).
Surgical treatment of patients with colonic diverticulitis
The surgery was performed in 126 of 1037 patients with right-sided diverticulitis, accounting for 12.2%, while the surgery was performed in 62 of 138 patients with left-sided diverticulitis, accounting for 44.9% (p < 0.005). Patients with right-sided colonic diverticulitis who underwent surgical management (n = 126) showed rates of cecal wedge resection of 38.9% (n = 49), bowel resection of 31.7% (n = 40), primary repair of 0.8% (n = 1), and appendectomy of 28.6% (n = 36). Patients with left-sided colonic diverticulitis who underwent surgical management (n = 62) showed rates of bowel resection of 93.6% (n = 58), primary repair of 3.2% (n = 2), and subtotal colectomy of 3.2% (n = 2) (Table 3). Stoma formation occurred most frequently in left-sided colonic diverticulitis, with a rate of 46.7% (n = 28) in left-sided colonic diverticulitis with surgical management versus 0.8% (n = 1) in right-sided colonic diverticulitis with surgical management (p < 0.005). The anastomosis rate after bowel resection was significantly lower in left-sided colonic diverticulitis, with a rate of 100% (n = 40) in right-sided and 46.7% (n = 28) in left-sided colonic diverticulitis (p < 0.005). The open surgery rate was significantly higher for left-sided (81.4%, n = 48) than for right-sided (59.7%, n = 77) colonic diverticulitis (p = 0.003). The laparoscopic surgery rate was significantly higher for right-sided (40.3%, n = 52) than for left-sided (18.6%, n = 11) colonic diverticulitis (p = 000.3).
Hinchey classification of patients with colonic diverticulitis
The conservative management group showed Hinchey classification type I as the most common classification for both right-sided (97%, n = 884) and left-sided (90.5%, n = 68) colonic diverticulitis. The incidence of type II was 2.6% (n = 24) and type III was 0.4% (n = 4) for right-sided colonic diverticulitis, whereas the incidence of type II was 9.4% (n = 7) and type III was 0% for left-sided colonic diverticulitis. The surgical management group showed types III and IV as significantly more common in left-sided than in right-sided colonic diverticulitis (p < 0.005). The incidence of type IV was 61.3% (n = 38) in left-sided and 7.1% (n = 9) in right-sided colonic diverticulitis. The incidence of type III was 30.6% (n = 19), II was 3.2% (n = 2), Ib was 1.6% (n = 1), and Ia was 3.2% (n = 2) in left-sided colonic diverticulitis, whereas the incidence of type III was 13.5% (n = 17), II was 17.5% (n = 22), Ib was 20.6% (n = 26), and Ia was 41.2% (n = 52) for right-sided colonic diverticulitis (Table 4).
Risk factor for surgery of colonic diverticulitis
Older age (OR, 0.972; 95% CI, 0.953 to 0.991), high BMI (≥ 25) (OR, 1.745; 95% CI, 1.026 to 2.996), and Hinchey classification types III and IV (OR, 0.002; 95% CI, 0.000 to 0.010) were associated with an increased risk of surgery for colonic diverticulitis (p < 0.005). Underlying medical disease, sex, number of attacks, and locations of lesions were not associated with a need for surgery for colonic diverticulitis (Table 5).
Discussion
In previous South Korean studies, the mean age of surgical patients with symptomatic colonic diverticulitis was 57.2 years (range 19–87 years), and the largest number of patients was in the 60–69 years age group [9]. In addition, the mean age was significantly higher in surgical patients with left-sided than with right-sided colonic diverticulitis [9]. In the present study, the mean age of the surgical patients with colonic diverticulitis was 47.8 years (range 13–95), and the mean age was significantly higher for surgical patients with left-sided than with right-sided colonic diverticulitis (left-sided 57.0 years vs. right-sided 41.4 years, p = 0.001). The reason for the relatively older age of left-sided diverticulitis patients requiring surgical management is unknown.
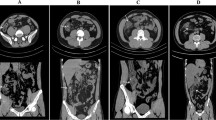
Colonic diverticulitis is now mainly diagnosed by computed tomography (CT). The CT scan with intravenous and oral contrast has a reported sensitivity of 98% and a specificity of 99% and has become a standard in the evaluation of suspected acute colonic diverticulitis [8,9,10]. CT scan findings of colonic diverticulitis include thickening of fascial planes, pericolic fat stranding, colonic wall thickening, the presence of an extraluminal mass, and an inflamed diverticulum. Therefore, CT scanning is very useful for evaluating the Hinchey classification used to identify the severity of colonic diverticulitis [10]. All colonic diverticulitis patients in the present study were diagnosed with CT scans, and patients who did not undergo CT were excluded from the study.
Distinguishing right-sided colonic diverticulitis from appendicitis with CT can sometimes be difficult, and a large proportion of right-sided diverticulitis has been misdiagnosed as acute appendicitis because of inflammation around the cecum [11]. In particular, the presence of an abscess pocket due to microperforation creates difficulties in distinguishing whether the abscess is due to colonic diverticulitis or to appendicitis. In the present study, the surgical management group contained patients who underwent appendectomy only (n = 36). Some of these patients underwent surgery for abscess drainage, while others underwent a combination of surgeries for diverticulitis and appendicitis.
Previous studies indicated younger age as a risk factor for more serious diverticulitis and higher recurrence of attacks, but a more recent study showed no association between younger age and worse outcomes or higher recurrences [12, 13]. In the present study, most patients with severe colonic diverticulitis who required surgical management were relatively older (especially patients with left-sided disease). A systematic review has shown recurrence rates of 10 to 35% after a first episode of uncomplicated diverticulitis [14]. Free perforation is more likely in patients who have no history of diverticulitis than in those with a previous episode (25% vs. 12%) [15]. Most patients who have a perforation of the bowel associated with colonic diverticulitis experience the perforation during their first attack [16]. However, in the present study, the recurrent attack rate for diverticulitis was relatively low (9.0%, overall), and of those patients, a second attack occurred in only 6.6%. Most patients (over 90.0%) in the present study had only experienced a first attack, and most did not relapse after treatment of the first attack. In addition, no significant difference was noted in the attack rate for the second or more incidents between the conservative management group and surgical management group. However, the attack rate was significantly higher for patients with right-sided than with left-sided diverticulitis.
Recent studies have shown that the number of attacks is not clearly associated with complicated diverticulitis that requires surgical management [7, 17, 18]. One study reported that many patients do not have another attack after the initial attack of uncomplicated diverticulitis and that only 3–5% have a recurrence of complicated colonic diverticulitis after uncomplicated diverticulitis [18]. In the present study, most of the surgical management for colonic diverticulitis was for first attacks (85.6%). The number of attacks and the locations of the lesions were not associated with a requirement for surgery in the present study.
In Western countries, acute colonic diverticulitis is predominantly left-sided, with right-sided diverticulitis being relatively rare and appearing only in 1.5% of patients [19]. A retrospective cohort study of patients in the USA with acute colonic diverticulitis reported incidences of 72% in the sigmoid colon, 33% in the descending colon, 3% in the transverse colon, and 5% in the ascending colon [20]. In contrast to Western countries, right-sided colonic diverticulitis has a higher incidence in Asian populations, including South Koreans [21, 22]. This difference is thought to be due to environmental factors, diversity of life, and genetics, but the exact reason is not known [23].
In the present study, the incidence of diverticulitis was much higher for the right-sided than for the left-sided (88.3% vs. 11.7%) colon (p < 0.005). In patients with right-sided colonic diverticulitis in the present study, 71.7% had the disease in the cecum, 7.7% in the mid ascending colon, and 8.6% in the hepatic flexure.
The most commonly used staging system for colonic diverticulitis is the Hinchey classification, which was developed in 1978 and subsequently modified [24, 25]. In the present study, patients in the surgical management group with right-sided colonic diverticulitis had more Hinchey types I and II disease (79.3%), whereas patients with left-sided colonic diverticulitis had more Hinchey types III and IV (91.9%) (p < 0.005). In other words, left-sided colonic diverticulitis was a more severe disease than right-sided colonic diverticulitis in patients who needed surgical management. The majority of the patients in the conservative management group with right-sided (99.6%) and left-sided colonic diverticulitis (100.0%) were Hinchey types I and II. One study has reported that left-sided colonic diverticulitis frequently required a multistage operation and was more often associated with postoperative morbidity and mortality when compared with right-sided colonic diverticulitis because of the higher Hinchey stage of left-sided versus right-sided colonic diverticulitis [9]. Another study reported that a diverting stoma was more common in the left-sided than right-sided colonic diverticulitis (62.5% vs. 6.3%, p < 0.001). In addition, open surgery was more common in left-sided than in right-sided colonic diverticulitis (90.6% vs. 71.9%), although the difference was not statistically significant [26]. In the present study, the surgical management group showed higher Hinchey stage type, open surgery rate, and stoma formation rate for left-sided than for right-sided colonic diverticulitis.
The present study has several limitations, including its retrospective design, significant selection biases, and small sample size. Nevertheless, the findings of the present study are meaningful for the analysis and demonstration of the characteristics and surgical outcomes of patients with colonic diverticulitis in Asia, and in South Korea in particular, compared with Western patients. The present study may also be helpful for future treatment of colonic diverticulitis disease.
In conclusion, the overall incidence of colonic diverticulitis is increasing gradually in South Korea. South Koreans have a very common right-sided colonic diverticulitis, but the surgical rate is low and often treated with conservative management, but the left-sided colonic diverticulitis is not common, but the surgical rate is very high and also the severity of the lesion is high. The mean age, distribution of age, BMI, open surgery rate, stoma formation rate, and Hinchey types III and IV incidence were significantly higher in patients requiring surgical treatment for left-sided than for right-sided colonic diverticulitis. Base on present study, Lt.-sided colonic diverticulitis tends to be more severe than Rt.-sided colonic diverticulitis, and surgery is more often required. In addition, colonic diverticulitis that requires surgery seems to be older and more obese on Lt.-sided colonic diverticulitis.
References
Berk HE (1985) Bockus gastroenterology, 4th edn. WB Saunder, Philadelphia
Song JH, Kim YS, Lee JH, Ok KS, Ryu SH, Lee JH, Moon JS (2010) Clinical characteristics of colonic diverticulosis in Korea: a prospective study. Korean J Intern Med 25:140–146
Martel J, Raskin JB (2008) History, incidence, and epidemiology of diverticulosis. J Clin Gasteroenterol 42:1125–1127
Jacobs DO (2017) Clinical practice. Diverticulitis. N Engl J Med 357:2057–2066
Wolff BG, Boostrom SY (2012) Prophylactic resection, uncomplicated diverticulitis, and recurrent diverticulitis. Dig Dis 30:108–113
Kim JS, Cha SG, Kim YT, Yoon YB, Song IS, Choi KW et al (1993) The prevalence and clinical features of diverticular disease of the colon. Korean J Gastroenterol 25:305–314
Chapman J, Davies M, Wolff B, Dozois E, Tessier D, Harrington J et al (2005) Complicated diverticulitis: is it time to rethink the rules? Ann Surg 242:576–581
Parks TG (1969) Natural history of diverticular disease of the colon. A review of 521 cases. Br Med J 4:639–642
Oh HK, Han EC, Ha HK, Choe EK, Moon SH, Ryoo SB et al (2014) Surgical management of colonic diverticular disease: discrepancy between right and left sided disease. World J Gastroenterol 20:1015–1020
Lameris W, van Randen A, Bipat S et al (2008) Graded compression ultrasonography and comuted tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol 18:2498–2511
Gilmore T, Jordan C, Edelstein E (2013) Right-sided diverticulitis mimics appendicitis. J Emerg Med 44:29–32
Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, Essani R, Beart RW (2005) The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol 100:910–917
Kotzampassakis N, Pittet O, Schmidt S, Denys A, Demartines N, Calmes JM (2010) Presentation and treatment outcome of diverticulitis in younger adults: a different disease than in order patients? Dis Colon Rectum 53:333–338
Regenbogen SE, Hardiman KM, Hendren S, Morris AM (2014) Surgery for diverticulitis in the 21st century: a systematic review. JAMA Surg 149:209–303
Rits JP, Lehmann KS, Frericks B, Stroux A, Buhr HJ, Holmer C (2011) Outcome of patients with acute sigmoid diverticulitis: multivariate analysis risk factors for free perforation. Surgery 149:606–613
Anaya DA, Flum DR (2005) Risk of emergency colectomy and colostomy in patients with diverticular disease. Arch Surg 140:681–685
Valizadeh N, Suradkar K, Kiran RP (2018) Specific factors predict the risk for urgent and emergent colectomy in patients undergoing surgery for diverticulitis. Am Surg 84:1781–1786
Bharucha AE, Parthasarathy G, Ditah I, Fletcher JG, Ewelukwa O, Pendlimari R, Yawn BP, Melton JL, Schleck C, Zinsmeister AR (2015) Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol 110:1589–1596
Nguyen GC, Sam J, Anand N (2011) Epidermiological trends and geographic variation in hospital admissions for diverticulitis in the United States. World J Gastroenterol 17:1600–1605
Wheat CL, Strate LL (2016) Trends in hospitalization for diverticulitis and diverticular bleeding in the United States from 2000 to 2010. Clin Gastroenterol Hepatol 14:96–103
Kim JH, Cheon JH, Park S, Kim BC, Lee SK, Kim TI, Kim WH (2008) Relationship between disease location and age, obesity, and complications in Korean patients with acute diverticulitis: a comparison of clinical patterns with those of Western populations. Hepatogastroenterology 55:983–986
Manabe N, Haruma K, Nakajima A, Yamada M, Maruyama Y, Gushimiyagi M, Yamamoto T (2015) Characteristics of colonic diverticulitis and factors associated with complications: a Japanese multicenter, retrospective, cross sectional study. Dis Colon Rectum 58:1174–1181
Commane DM, Arasaradnam RP, Mills S, Matchers JC, Bradburn M (2009) Diet, ageing and genetic factors in the pathogenesis of diverticular disease. World J Gastroenterol 15:2479–2488
Hinchey EJ, Schaal PG, Richards GK (1978) Treatment of perforated diverticular disease of the colon. Adv Surg 12:85–109
Barat M, Dohan A, Pautrat K, Boudiaf M, Dautry R, Guerrache Y, Pocard M, Hoeffel C, Eveno C, Soyer P (2016) Acute colonic diverticulitis: an update on clinical classification and management with MDCT correlation. Abdom Radiol (NY) 41:1842–1850
Al-Temimi MH, Trujillo CN, Mahlberg S, Ruan J, Nguyen P, Yuhan R et al (2018) Surgical intervention for right-side diverticulitis: A case-matched comparison with Left-side diverticulitis. Am Surg 84:1608–1612
Funding
This work was financially supported by the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lim, D.R., Kuk, J.C., Shin, E.J. et al. Clinical outcome for management of colonic diverticulitis: characteristics and surgical factor based on two institution data at South Korea. Int J Colorectal Dis 35, 1711–1718 (2020). https://doi.org/10.1007/s00384-020-03639-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03639-2