Abstract
Background
Pilonidal disease (PD) is a common disease of the natal cleft, which can lead to complications including infection and abscess formation. Various operative management options are available, but the ideal technique is still debatable. Recurrent PD after surgical treatment is frequent event for the 25–30% of cases. The present study evaluated endoscopic pilonidal sinus treatment (EPSiT) in recurrent and multi-recurrent PD.
Methods
Of the consecutive prospective patients with recurrent PD, 122 were enrolled in a prospective international multicenter study conducted at a secondary and tertiary colorectal surgery centers. Primary endpoint was to evaluate short- and long-term outcomes: healing rate/time, morbidity rate, re-recurrence rate, and patient’s quality of life (QoL).
Results
Complete wound healing rate was occurred in 95% of the patient, with a mean complete wound healing time of 29 ± 12 days. The incomplete healing rate (5%) was significantly related to the number of external openings (p = 0.008), and recurrence was reported in six cases (5.1%). Normal daily activity was established on the first postoperative day, and the mean duration before patients returned to work was 3 days. QoL significantly increased between the preoperative stage and 30 days after the EPSiT procedure (45.3 vs. 7.9; p < 0.0001).
Conclusions
The EPSiT procedure seems to be a safe and effective technique in treating even complex recurrent PD. It enables excellent short- and long-term outcomes than various other techniques that are more invasive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pilonidal disease (PD) is a common inflammatory disease of the buttocks and gluteal fold. It manifests mainly in young men and is associated with being overweight, having a sedentary lifestyle and local irritation. PD usually causes pain and can lead to complications such as the formation of abscesses and acute or chronic recurrent infections [1]. Optimal treatment for primary PD is still under discussion, considering a high recurrence rate of between 15 and 30%. Results after surgical treatment for secondary or tertiary recurrence of PD are more unsatisfactory with a relapse rate of up to 30% [2].
Broad classical excision with the wound left open to heal by secondary intention, or directly closed with lateral or medial wound closure, remains the most common surgical procedure also performed for PD recurrence, but these procedures are associated with very high recurrence rates [3,4,5]. Flap techniques are described to reduce the rate of recurrence, but are more frequently associated with local complications, pain, discomfort, longer rest days, and reduced quality of life [6].
In agreement with the above tests, the use of wide open/close excision techniques in the last decade, which are associated with significant postoperative discomfort and correlated with a non-negligible recurrence rate, have received a re-evaluation criticism [7, 8]. Minimally invasive and outpatient surgical techniques, able to guarantee a reduced cost for the hospital stay and a consequent minimal morbidity, were more frequently considered in the treatment of PD.
In 2013, Meinero and Collegues [9] described a new type of minimally invasive treatment for PD, the endoscopic treatment of pilonidal sinus (EPSiT). The authors used the same equipment and technology for the treatment of video-assisted anal fistula (VAAFT) [10] for the treatment of primary and current pilonidal sinus. The concept of EPSiT is to endoscopically remove the entire infected and infected area within the pilonidal sinus cavity with a fistuloscope introduced through a small circular incision of about half a centimeter in diameter that should substantially reduce the operational morbidity associated with more extensive flap.
Several authors have reported a good postoperative outcome considering the short- and long-term follow-up, but there is still no evidence on the efficacy and safety of the EPSiT procedure in the pilonidal recurrent pathology.
The aim of this study is to present a series of 122 consecutive patients treated with the EPSiT procedure for relapsing PD and to analyze the results in the short and long term.
Materials and methods
From March 2012 to December 2014, a total of 122 consecutive patients with recurrent PD underwent the EPSiT procedure in four different centers: Sestri Levante Hospital (GE), Sanatrix Clinic (Rome), Madonna delle Grazie Clinic (Velletri, Rome), and EOC Hospital of Mendrisio (Switzerland). The multicenter prospective study was preliminarily approved by the hospital ethics committee, and an informed consent of the patient was obtained prior to the operation. Clinical features, preoperative and postoperative data, and follow-up data were recorded prospectively.
In order to evaluate the EPSiT procedure in relapses, we included all patients with early or late failures after previous excision surgery or patients with persistence of PD after surgical excision. Patients with acute pilonidal abscesses, malignant neoplasms under treatment, inflammatory bowel disease, neurological disease, and coagulation disorder were excluded from the study.
All patients were admitted on the day of the operation and no antibiotic prophylaxis was administered. All procedures were performed as day-case procedure under local anesthesia. Local anesthesia was achieved using the injection in the 40 ml zone of a solution consisting of 2% Lidocaine and 7.5% Naropine. All patients were placed in a prone position with legs slightly apart. No changes were made to the surgical technique and anesthetic protocol during the study period.
After the surgery, the patients were followed weekly by 2 weeks after surgery in the outpatient clinic by the operating surgeon; follow-up continued until the wound was healed, or until further surgery was required. Long-term follow-up and recurrence of the disease were both evaluated by the outpatient consultation.
We considered complete wound healing as a primary endpoint; incomplete healing was defined when the wound or swelling persisted after 60 days postoperatively.
Patients were reported to relapse if they reported symptoms of local pain, intermittent secretion, or swelling after at least 4 months from the time of complete recovery.
The secondary endpoint refers to a quality of life assessment (QoL). Two different questionnaires were administered: the SF-36 (validated Italian version) and an in-house QoL questionnaire specifically prepared for proctological disease, in order to perform the following: (1) evaluate the symptoms (pain, body temperature, wound secretion, frequency removal of the dressing on a scale from 0 to 20, where 0 represented absence of fever, pain, wound secretion, and no need to remove the dressing); (2) a general QoL evaluation (scale from 1 to 6, where 1 represents “a very good QoL”); (3) an evaluation of the impact of PD on patient QoL (scale from 0 to 52, where 0 represented without significant impact of PS on QoL); and (4) an evaluation of the last 30 days of QoL in terms of concern, discomfort, and depression regarding PD (score 1 to 6, where 1 represented without feelings of concern, discouragement, or depression related to PD). The preoperative scores of each element were calculated and compared with postoperative scores obtained on postoperative day 30.
Surgical technique
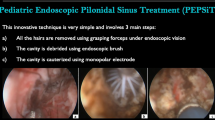
The EPSiT procedure consists of two phases: a diagnostic phase and an operative phase. The purpose of the diagnostic phase is to identify the anatomy of the PS and any possible secondary trait and/or abscess cavities. The midline or the outer lateral opening is removed by making a 0.5-cm circular incision around the opening. The number and site of incisions varies depending on the presence of secondary traits or abscesses of the fistula; therefore, in more complex cases two or three incisions may be necessary. As shown in Fig. 1, the Meinero fistuloscope [9, 10] (the fistuloscope has an 8° angle eyepiece with an optical channel and an operating channel of 3.2 × 4.8 mm in diameter, and its operative length is 18 cm) is then inserted through the external opening, while the infusion of 1% glycine/mannitol solution helps to open the underlying section. Hair, fistulas and abscess cavities clearly appear on the screen. The purpose of the operating phase is to ablate and clean the infected area. Endoscopic forceps are inserted through the operative channel to completely remove all hair follicles and directly visible hair. This maneuver is considered a fundamental step in healing assistance. Once this procedure is completed, the monopolar electrode is connected to a blade electrosurgical unit for the ablation with cautery of the sinus granulation tissue. This begins in the main stretch and, if necessary, crosses secondary sections and abscess cavities. The necrotic material is removed with an endobrush passed through the fistuloscope, or with a Volkmann spoon if more superficially placed.
The continuous jet of glycine-mannitol solution during the procedure ensures both a clear visual field and the elimination of the cauterized waste material, which is brushed through the incision. Additional pilonidal midline pits are then treated with curettage and cauterization. At the end of the procedure, a light dressing is applied without packing.
Statistical analysis
Statistical analyses were performed using MedCalc for Windows version 10.2.0.0 (MedCalc Software, MariaKerke, Belgium). The differences in distribution were calculated using the ANOVA test for continuous variables and the chi-squared test or Fisher’s exact test, depending on the number of cases in each subgroup for categorical variables.
Results
The clinical results and characteristics of the patients are shown in Table 1. The patient sample was mainly male (70%) with a mean age of 25.9 ± 4.2 years. The EPSiT procedure was performed as a secondary treatment for PD in 89 cases (72.9%), as a tertiary treatment in 26 cases (21.3%), and as a fourth surgical operation in 7 patients (5.7%). The mean operative time was 50 min (range, 40–70 min). A re-EPSiT procedure was performed in 13 patients (10.6%) with incomplete healing or relapse following first-line treatment with EPSiT. The mean number of pilonidal openings per patient was 1.66 (range 1–4); of these, 82 cases (67.2%) were located in the midline, 21 cases (17.3%) located in the midline with one or more additional side openings, and 19 patients (15.5%) presented a lateral opening. In the immediate postoperative period, all patients returned to normal painless daily activity on the first postoperative day, the average duration before returning to work was 3 days (range 1–4), and 10.9% of patients required analgesics (paracetamol 1 g, if necessary). In this series, no early complications of the wound were observed (e.g., hematoma, seroma, or necrosis) requiring hospitalization or emergency assessment.
A complete wound healing rate of 95% was reported after a mean 16-month follow-up period, although 110 patients recovered within 2 months postoperatively. The average wound healing time was 29 ± 12 days (range 10–60) (Table 2). Six patients had incomplete healing (5%) and failed healing was significantly related to the number of external openings (p = 0.008): when PD was associated with a healing, opening occurred in 1.7% of patients; when PD was associated with two openings, the failure of healing occurred in 3.8% of patients; and finally, when PD was associated with three or more openings, the failure of healing occurred in 21.4% of patients. In six cases recurrence occurred after complete wound healing (> 6 weeks) despite two patients (1.6%) were lost from follow-up. All remaining 12 patients (9.8%), of these 7 (58.3%) with incomplete healing and 5 patients (41.7%) with relapse, underwent re-EPSiT procedure and complete recovery occurred within 30 days postoperatively in 10 patients (83%); however, two patients were lost from follow-up.
The QoL of 45 patients was studied. The scores of SF-36 were significantly improved for all the items studied: physical function (PF), role-physical (RP), body pain (BP), general health (GH), vitality (VT), social function (SF), role-emotional (RE), and mental health (MH) (p < 0.0001, t test). When the internal QoL score questionnaire was analyzed, the mean preoperative QoL score was 43.1 ± 2.8, while on the 30th postoperative day, the mean score was 8.9 ± 1.2, with a statistical difference significant between the two scores (p < 0.0001, t test) (Fig. 2).
Discussion
The recurrence rates after treatment with PD associated with various surgical procedures can range from 0 to 40% [11]. Over the past three decades with the intent of lateralizing and flattening the natal fissure, while providing a healthy tissue coverage of the defect without the risk of tension in the suture line, procedures based on the off-center flap (Limberg, Karidakis, “clift left”) “modified Bascom technique and ZV flaps” have been shown to significantly reduce recurrence and incomplete wound healing rate [11, 12].
These procedures, however, if in one hand they reduce the recurrence rates, in another hand they expose the patients to a high rate of non-negligible morbidity and are associated with long hospital stays, high hospital costs (outpatient visits, dressing changes, etc.), and long off-work time.
Several randomized trials have demonstrated wound-related complications such as seroma, hematoma, deep infectious collection, wound dehiscence, and infection in up to 25% of cases [13].
A recent RCT that compares the efficacy of Limberg and Karydakis flap in recurrent pilonidal sinus disease in a population study of 71 patients described a 53.5% of the total morbidity rate with 38 patients with fluid collection, wound infection, flap edema, hematoma, and partial dehiscence of the wound [14].
Ideally, the goals of treatment for this disease should be reliable wound healing with a low risk of relapse, a short period of hospitalization, low morbidity, and minimal discomfort for the patient. By focusing on this last topic, we need to take into account the young age of the patients, their intense social, and work life and recognize that current resection techniques are often associated with serious impairments of patient QoL and long “off-the-job” periods. Nordon and Senapati [15] described a median of 2 weeks off work (interval, 1–6 weeks) after the “simple” Bascom procedure, and after the patient left the procedures modified by Bascom. A recent meta-analysis of RCT comparing surgical outcomes after primary closure or rhomboidal excision and Limberg limb for primary sacrococcygeal pilonidal disease management showed a mean of 9.24% of the surgical infection rate, an average of 5 days postoperative hospital stay, and an average of 20 days for complete return to work [14].
Although many approaches to operational management of the pilonidal sinus are available for many years, there is still no consensus on which technique is most effective, and this sentence is equally true in the recurrences. This is the first study in the literature focusing on the EPSiT procedure in recurrent PD. Despite a small sample size, this procedure seems to offer adequate and effective results in wound healing, as well as a 5.1% relapse rate at a median follow-up of 16 months and an incomplete wound healing of the 5%. Furthermore, when PD was persistent or recurrent (12 cases), re-EPSiT was able to effectively treat the disease with a further 8.3% success rate. The EPSiT approach allows the surgeon to directly visualize the sinus tract and any secondary tracts or cavities that may be present. This is far superior to detecting secondary traits by blind palpation, as the thickness of the tissue and the depth of the stretch make it unreliable. In addition, direct vision allows hair removal and homogeneous diathermy without losing any area and avoids causing unnecessary damage. Overall, patients undergoing EPSiT seem to have a high rate of satisfaction. This could be due to the low postoperative pain level and the rapid return to work and daily activities. The initial studies also showed good rates of healing and low recurrence rates. A recent meta-analysis by Tien et al. [16] out of eight articles with the EPSiT technique reported a complete cure in all study patients [9, 17, 18]. Two other studies reported recovery rates of over 88% in their patients [19, 20].
A larger number of external openings was associated with a higher rate of incomplete wound healing (p = 0.01). Two of the studies did not record healing as a result [18, 21]. No repetition occurred during the follow-up period in three studies [9.17, 21]. A recurrence rate of 5% or less was achieved in four studies [20,21,22]. One study did not measure recurrence as a result [19]. The patient satisfaction rate was reported as 97 and 93% by Giarratano et al. and Milone et al., respectively [21, 22]. Another study reported a 78% satisfaction rate, but in only nine patients. When minimally invasive and conventional treatment was compared, the patients in the minimally invasive group expressed greater satisfaction at 1 month and 6 months after surgery (p < 0.001) [13].
A randomized study [18] compared the endoscopic treatment of pilonidal sinus with conventional surgery (Bascom-cleft lift procedure) in a cohort of 145 consecutive patients. Although patients undergoing endoscopic treatment had significantly shorter working time (1.6 vs. 3.9 days) and greater patient satisfaction, rates of recurrence and complications were comparable between the two groups without they observed significant differences. An important ending of this particular study was that a difference of more than 2.5 cm between the lateral sinus orifice and the midline was a significant predictor for postoperative wound complications with hazard ratio of 9.6 and p value of 0.004. The limits of endoscopic pilonidal sinus treatment are similar to those of VAAFT that Emile and colleagues have elaborated in a previous review [23].
These disadvantages include the need for adequate training to achieve the required experience, in addition to the cost of the stethoscope and kit. On the other hand, the cost of the equipment required for the procedure is sustained only once and the fistuloscope can be used for the treatment of both PD and anal fistula. Short hospital stays, less postoperative pain, reduced need for dressing changes, and shorter work time can help reduce secondary costs and make the procedure cost-effective for PD. Despite these promising results, the present study presents several limitations. Firstly, the small sample size can be a positive factor and can reduce the power of the analysis and underestimate the complications associated with the use of EPSiT; moreover, in consideration of the data provided here, all patients must be monitored long-term QoL. Finally, it is not a randomized study, for a better evaluation of the functional outcome a prospective randomized study with a long-term follow-up may be required.
Conclusions
Considering the alternative standard flap techniques in recurrences, EPSiT guarantees a fast postoperative course with a return to normal daily activities in 1 day, and a return to work in 3 days after the procedure without significant morbidity rate. It is therefore considered that re-EPSiT is safe to perform, and can offer a high success rate; furthermore, the patient requires a judicious postoperative evaluation in an outpatient setting, in order to detect early recurrence or incomplete healing. However, it is acknowledged that further studies involving a long-term follow-up are required to confirm these promising results.
References
McCallum I, King PM, Bruce J (2007) Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev (4):CD006213 Review. Update in: Cochrane Database Syst Rev. 2010;(1):CD006213
Iesalnieks I, Deimel S, Schlitt HJ (2013) Karydakis flap for recurrent pilonidal disease. World J Surg 37(5):1115–1120
Bascom J (1980) Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery 87:567–572
Bascom J (1983) Pilonidal disease: long-term results of follicle removal. Dis Colon Rectum 26:800–807
Tejirian T, Lee JJ, Abbas MA (2007) Is wide local excision for pilonidal disease still justified? Am Surg 73(10):1075–1078
Karydakis GE (1973) New approach to the problem of pilonidal sinus. Lancet 2(7843):1414–1415
Gips M, Melki Y, Salem L, Weil R, Sulkes J (2008) Minimal surgery for pilonidal disease using trephines: description of a new technique and long-term outcomes in 1,358 patients. Dis Colon Rectum 51(11):1656–1662
Kepenekci I, Demirkan A, Celasin H, Gecim IE (2010) Unroofing and curettage for the treatment of acute and chronic pilonidal disease. World J Surg 34(1):153–157
Meinero P, Mori L, Gasloli G (2014) Endoscopic pilonidal sinus treatment (E.P.Si.T.). Tech Coloproctol 18(4):389–392
Meinero P, Mori L (2011) Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol 15:417–422
Steele SR, Perry BW, Mills S, Buie WD (2013) Practice parameters for the management of pilonidal disease. Dis Colon Rectum 56:1021–1027
Karakayali F, Karagulle E, Karabulut Z, Oksuz E, Moray G, Haberal M (2009) Unroofing and marsupialization vs. rhomboid excision and Limberg flap in pilonidal disease: a prospective, randomized, clinical trial. Dis Colon Rectum 52:496–502
Horwood J, Hanratty D, Chandran P, Billings P (2012) Primary closure or rhomboid excision and Limberg flap for the management of primary sacrococcygeal pilonidal disease? A meta-analysis of randomized controlled trials. Color Dis 14(2):143–151
Bali İ, Aziret M, Sözen S, Emir S, Erdem H, Çetinkünar S, İrkörücü O (2015) Effectiveness of Limberg and Karydakis flap in recurrent pilonidal sinus disease. Clinics (Sao Paulo) 70(5):350–355
Nordon IM, Senapati A, Cripps NP (2009) A prospective randomized controlled trial of simple Bascom's technique versus Bascom's cleft closure for the treatment of chronic pilonidal disease. Am J Surg 197(2):189–192
Tien T, Athem R, Arulampalam T (2018) Outcomes of endoscopic pilonidal sinus treatment (EPSiT): a systematic review. Tech Coloproctol 22(5):325–331
Gecim IE, Goktug UU, Celasin H (2017) Endoscopic pilonidal sinus treatment combined with crystalized phenol application may prevent recurrence. Dis Colon Rectum 60(4):405–407
Milone M, Fernandez LMS, Musella M, Milone F (2016) Safety and efficacy of minimally invasive video-assisted ablation of pilonidal sinus. JAMA Surg 151(6):547–553
Chia CLK, Tay VWY, Mantoo SK (2015) Endoscopic pilonidal sinus treatment in the Asian population. Surg Laparosc Endosc Percutan Tech 25(3):e95–e97
Meinero P, Stazi A, Carbone A, Fasolini F, Regusci L, La Torre M (2016) Endoscopic pilonidal sinus treatment: a prospective multicentre trial. Color Dis 18(5):O164–O170
Milone M, Musella M, Di Spiezio Sardo A, Bifulco G, Salvatore G, Sosa Fernandez LM et al (2014) Video-assisted ablation of pilonidal sinus: a new minimally invasive treatment—a pilot study. Surgery 155(3):562–566
Giarratano G, Toscana C, Shalaby M, Buonomo O, Petrella G, Sileri P (2017) Endoscopic pilonidal sinus treatment: long-term results of a prospective series. JSLS J Soc Laparoendosc Surg 21(3):e2017.00043
Emile SH, Elfeki H, Shalaby M, Sakr A (2018 Apr) A systematic review and meta-analysis of the efficacy and safety of video-assisted anal fistula treatment (VAAFT). Surg Endosc 32(4):2084–2093
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data: PM, GL, AS, AC, FF, LR, MLaT. Drafting the article or revising it critically for important intellectual content: PM, GL, AS, AC, FF, LR, MLaT. Final approval of the version to be published: PM, GL, AS, AC, FF, LR, MLaT.
Corresponding author
Ethics declarations
Conflicts of interest
Professor Piercarlo Meinero declares to receive financial grants from Karl Storz. The remaining authors declare no potential financial conflict of interest related to this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meinero, P., La Torre, M., Lisi, G. et al. Endoscopic pilonidal sinus treatment (EPSiT) in recurrent pilonidal disease: a prospective international multicenter study. Int J Colorectal Dis 34, 741–746 (2019). https://doi.org/10.1007/s00384-019-03256-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03256-8