Abstract
Background
Colorectal cancer (CRC) is the third most frequent cancer diagnosed in men and the second in women. Laparoscopic surgery has been a technical revolution in colorectal surgery, facilitating a better recovery of patients with lower morbidity and better esthetic results, compared to traditional surgery via laparotomy, without compromising safety and long-term oncological results.
Purpose
The trial is a randomized controlled trial indented to evaluate the two interventions with thorough measurements of the postoperative variables and complications to improve the evaluation of the surgical technique. The primary endpoint is to compare the hospital stay, which will be measured in days between both groups. The purpose of the study at secondary endpoints is to compare intraoperative and postoperative events between both groups in terms of operating time, anastomotic performance time, intraoperative complications, number of harvested lymph nodes, need for blood transfusion, length of the surgical wound, start and tolerance of oral intake, beginning of digestive functionality, postoperative pain, need for analgesic administration, surgical wound infection, paralytic ileus, anastomosis leakage or dehiscence, need for surgical reintervention, and hospital readmission within the first 30 days after surgery.
Methods
This trial is a prospective, randomized, single-blind, and single-center clinical trial comparing intracorporeal anastomosis versus extracorporeal anastomosis for right laparoscopic hemicolectomy.
Conclusions
Nowadays, there are several retrospective trials comparing the benefits for extracorporeal anastomosis versus intracorporeal anastomosis in right colon cancer patients. Considering the impact for laparoscopic surgery, we think it is necessary to do a randomized trial comparing extracorporeal versus intracorporeal anastomosis modalities.
Trial registration
www.clinicaltrials.gov No. NCT02667860 and Hospital de la Santa Creu i Sant Pau Research Institute No. IIBSP-AIE-2015-01
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
Colorectal cancer (CRC) is the third most common cancer in men and the second most common in women, with an estimated 1.4 million cases and 693,900 deaths per year [1]. In America, 132,770 patients were diagnosed with CRC in 2015 [2]. In Spain, right colon tumors represent about 30% of cases of CRC.
Despite advances in the field of oncology, surgical treatment remains the best option for these patients, with right hemicolectomy being the most frequently performed surgical procedure.
In recent years, one of the main fields of development has been minimally invasive surgery, the aim of which is to cause the least possible impact on the patient and to enhance postoperative recovery. Laparoscopic surgery has created a technical revolution in colorectal surgery, facilitating better recovery of patients with lower morbidity and better esthetic results than those with traditional surgery via laparotomy. And most importantly, these results do not compromise safety or long-term oncological results [3,4,5].
Currently, there are three main approaches to a right hemicolectomy. The first of these is laparoscopy-facilitated right hemicolectomy. In this approach, colon dissection is performed laparoscopically, and then, through a mini laparotomy, the vessels are ligated, and ileocolic anastomosis is carried out. A second approach is laparoscopic-assisted right hemicolectomy, in which the dissection and ligation of the vessels are performed laparoscopically, but the anastomosis is performed extracorporeally through an abdominal incision. And third, a total laparoscopic hemicolectomy can be performed. In this approach, vessel dissection, sectioning of the piece, and anastomosis are all performed laparoscopically, and the piece is extracted through a Pfannenstiel incision. Performing an intracorporeal anastomosis is a technical challenge that requires advanced laparoscopic skills and extensive experience by the surgeon.
Ileocolic anastomosis can be performed in multiple ways—end-to-end, side-to-side, end-to-side, and side-to end anastomosis [6]—using handsewn, stapled, or mixed methods [7,8,9,10]. Currently, we can say that the most frequent approaches are side-to-side anastomosis (80%) and end-to-side anastomosis (15.1%). Stapled anastomosis is performed in 70.6% and handsewn anastomosis in 29.4% [11]. In addition, side-to-side anastomosis can be isoperistaltic or antiperistaltic, and it is controversial as to which offers better results [12].
In recent years, several meta-analysis have compared the laparoscopic technique with extracorporeal anastomosis (EA) versus the technique with intracorporeal anastomosis (IA), defining the latter technique as superior in view of its faster postoperative recovery and shorter hospital stay with less morbidity. Furthermore, as long as the technique is carried out by expert surgeons, recovery of intestinal functionality and tolerance to a solid diet is faster, and there is less use of analgesia [13,14,15,16,17,18,19,20,21,22,23]. In addition, there is a clear esthetic benefit when the anastomosis is performed intracorporeally through a Pfannenstiel incision [24,25,26].
Another benefit of IA over EA is less postoperative pain. The most widely accepted explanation for this is that IA does not involve traction of the mesenteric-portal axis while EA does. It seems that less traction, besides mediating postoperative pain, is also responsible for the appearance of paralytic ileus. The incidence of paralytic ileus appears to be higher the greater the manipulation. In patients undergo an IA, the assistance incision is Pfannenstiel’s suprapubic incision, which is only used for the extraction of the surgical piece. Pfannenstiel’s incisions have a lower incidence of superficial surgical wound infection, a lower rate of eventration, and lower analgesic requirements, along with esthetic results that are superior to the incision in the right hypochondrium or in the supraumbilical midline. Conversely, right hypochondrium incisions can cause atelectasis and alterations in respiratory function.
The literature contains many studies that confirm all the aspects described above, but most reports are non-randomized, retrospective, and carried out in heterogeneous groups of patients, which might induce patient selection bias. In eight studies in which the most recent meta-analyses are based, the sample size is less than 90, making it difficult to obtain statistically significant results and to reach reasonable conclusions [19, 22, 23, 27,28,29,30,31].
In the study by Franklin et al., the characteristics of the patients included in the IA and EA groups are not defined, so it is not clear whether or not the groups are comparable. In addition, some of the patients included in this study were patients operated on from the emergency department, which cannot be extrapolated to patients who had elective surgery. Furthermore, results from patients with benign pathology are compared with those from patients with oncological pathology [32]. Another author describes a series in which the patients in the two groups differ in terms of the ASA scale and in terms of pathology, and IA was performed in only 23 patients [30]. Other studies include patients with malignant diseases and patients with benign colonic pathology, which could lead to the creation of heterogeneous patient groups. Both the surgical strategy and the extension of the resection will be different if it is an oncological resection or a resection for a benign pathology. In addition, the age at presentation of a malignant pathology differs from that of a benign pathology, as do the possible post-surgical complications [20, 21, 23, 29, 31, 33].
Other points to be considered are that many studies are heterogeneous regarding the anastomosis approach performed. One author, for example, does not refer to the type of anastomosis [34], and other authors applied both stapled and manual procedures for extracorporeal anastomosis [23, 30, 32]. Furthermore, several studies changed their approach from IA to EA halfway through the inclusion period, using EA as the historic control group [20,21,22,23, 28]. And in various articles, the definition of post-surgical complications differs, or the period of time (30, 60, or 90 days) is not stated. Besides, only 25% of the authors use the Clavien-Dindo classification to determine morbidity [18].
The six meta-analysis published concluded that all data were collected from non-randomized retrospective studies, with significant heterogeneity in the studies. This leads to the conclusion that there is no evidence for one procedure being superior to the other and shows that prospective randomized studies are necessary.
All the above prompted us to perform a prospective randomized study to compare the two surgical techniques and to define the possible benefits of IA versus EA in a group of patients undergoing elective right hemicolectomy for oncological pathology.
Objective
This randomized controlled trial intends to measure postoperative variables and complications after IA and EA in order to evaluate the surgical technique. The study design allows objective assessment of the potential benefits and risks of IA compared to EA.
Trial design
The trial is a prospective, randomized, single-blind, and single-center clinical trial comparing intracorporeal anastomosis versus extracorporeal anastomosis for right laparoscopic hemicolectomy. Patients who met the criteria for inclusion in the study are randomized immediately before intraoperative anastomosis by means of randomization envelopes. The patients do not know which surgical technique they are going to receive.
Methods and design
Study population and eligibility criteria
All patients aged ≥ 18 years old referred for oncological pathology located in the right colon and requiring a right hemicolectomy assisted by laparoscopy with an R-0 purpose are considered for inclusion.
Trial location
The trial will be conducted at a single-center with expertise in laparoscopic colorectal surgery, Hospital de la Santa Creu I Sant Pau, Universidad Autonoma, Barcelona, Spain.
Inclusion criteria
-
Patients admitted for elective right hemicolectomy due to right-sided colon cancer
-
Cancer-free resection expected
-
Age between 18 and 99 years informed consent
-
ASA score of I, II, or III
-
Tumor located in cecum, ascending or hepatic-angle colon
-
Single surgical procedure
Exclusion criteria
-
Inability to consent
-
Locally advanced tumor or metastatic disease
-
Patients with benign colon disease and patients with intestinal bowel disease (Crohn’s disease or ulcerative colitis)
-
Emergency surgery
-
ASA score of IV
-
Need for more than one surgical procedure
-
Tumor located in transverse, splenic-flexure, descending or sigmoid colon
-
Open surgery
Interventions
With the patient placed supine in neutral position, the surgeon and both assistants stand on the left, and the laparoscopy tower is situated on the right. The first trocar is positioned in the left flank using an optiview trocar, and exploratory laparoscopy is performed. The presence of carcinomatosis or hepatic lesions not visualized in CT before surgery is assessed, and the resectability of the lesion is determined. One trocar is then placed at the right iliac fossae, and another is placed at the hypogastrium to act as working ports. A fourth trocar is positioned in left flank for assistance. The dissection starts with identification, dissection, ligation with hemostatic clips, and section of the ileocolic vessels. The colon is mobilized systematically from medial-to-lateral with retroperitoneal dissection, identifying the duodenum and pancreas. The right branch of the middle colic artery is identified and ligated with hemostatic clips. Mobilization of distal ileum and right colon is then started, with the dissection of Told’s fascia until free mobilization of colon liver flexure is achieved.
The envelope is then opened. If IA is designated, the ileum and the transverse colon are transected using an Endo-GIA stapler, and the piece is placed over the liver. A side-to-side isoperistaltic or antiperistaltic anastomosis is created with the 60 mm endostapler, and the enterotomy is closed with continuous suture with 2–0 prolene. The specimen is extracted through a Pfannenstiel incision, which is protected with an Alexis device. A Blake surgical drainage is placed.
If EA is designated, a Kocher or middle-line incision is made, protected with an Alexis device. The ileum and colon are extracted, the dissection of the mesocolon is continued, the transection of ileum and colon is performed with a 60 mm GIA stapler, and the specimen is extracted. A side-to-side isoperistaltic or antiperistaltic anastomosis is created with a 60 mm GIA stapler, anastomosis with 3–0 vicryl is reinforced, and the transverse section of the ileum and the colon’s enterotomy is performed with a 90 mm TA proximate stapler. A Blake surgical drainage is placed if the surgeon deems this necessary.
Preoperative and perioperative management
All patients are diagnosed with right colon cancer through colonoscopy and biopsy of the lesion. Abdominal CT scan and routine blood test will be performed systematically. Patients will not undergo a mechanical colon preparation. They can drink hydrocarbonated beverages up to 2 h before surgery.
The surgery is performed under general anesthesia with endotracheal intubation, bladder catheterization, nasogastric tube, antithrombotic measures, and systematic antibiotic prophylaxis with ceftriaxone and metronidazole. Doses will be repeated if the surgery is prolonged more than 3 h, if the blood loss is greater than 1500 ml, or if the patient is obese. Special care will be taken regarding normothermia and control of glycaemia. A regimen of fluids and electrolytes will be established to maintain normovolemia.
All patients are managed using an enhanced recovery after surgery (ERAS) protocol following ERAS guidelines, as suggested by Gustafsson et al. [35]. Liquid tolerance will be started 6 h after surgery along with early mobilization. The same analgesic regimen will be administered in all patients.
Discharge criteria
-
Tolerance of oral intake
-
Absence of uncontrolled post-surgical complications requiring immediate medical or surgical treatment
Abandonment causes
-
Express will of the patient
-
Protocol violation
-
Withdrawal of informed consent
-
Loss of follow-up
-
Medical decision
Outcome parameters
Primary endpoint
The primary endpoint is to compare the hospital stay, which will be measured in days, between the two groups. The first day of hospital stay is considered the first postoperative day, beginning at 8:00 am. The last day of hospital stay is considered the day of medical discharge at 8:00 am.
Secondary endpoints
Secondary endpoints are as follows. We will compare intraoperative and postoperative events between the two groups in terms of operating time, anastomotic performance time, intraoperative complications (hollow organ perforation, solid organ lesion, bleeding), number of harvested lymph nodes, need for blood transfusion, length of the surgical wound, start and tolerance of oral intake, beginning of digestive functionality (the day the patient first passes stools), postoperative pain registry according to the analog visual scale, for analgesic administration needs, surgical wound infection, paralytic ileus, anastomosis leakage or dehiscence, need for surgical reintervention, hospital readmission within the first 30 days after surgery, and number and cause of death. All complications will be evaluated according to Clavien-Dindo classification.
Sample size
Depending on the series, the incidence of postoperative complications after right hemicolectomy is highly variable. Some authors divide postoperative complications into minor complications (AI 7.4% vs EA 16.3%) and major complications (IA 2.4% vs EA 9.8%) [32], while others describe complications as early or late [23], and still others divide them into gastrointestinal and others [30].
Scatizzi distinguishes complications as surgical site versus non-surgical site complications: 2.5% in the IA group vs 5% in the EA group [27]. Fabozzi et al. divided complications into intraoperative and postoperative. There were 0% complication reported in the AI group, while a 30% overall complication rate was reported in the EA group [34].
The most recent meta-analysis to date reports an incidence of postoperative complications of 25% for the IA group vs − 34% for the EA group [18]. In addition, only 25% of the articles described postoperative complications with the Clavien-Dindo classification. In view of the great variability of data on the incidence of morbidity, together with the clear definition of complications and the non-use of the classification of Clavien-Dindo, we decided we could not use the morbidity data as a variable to calculate sample size.
The incidence of anastomotic leakage is very low both for IA (0–2.3%) and for EA (0–3.01%) [19,20,21,22,23, 27,28,29, 31, 33, 34]. In the same way, the definition of anastomotic leak varies according to the different authors. Therefore, we did not think it would be convenient to use either the morbidity or the anastomotic leak to calculate the sample size.
As the main variable for the calculation of the sample size, we chose a numerical and objective variable such as the hospital stay, instead of a subjective variable, making a calculation based on the hospital stay of articles prior to 2015. The average length of hospital stay with standard deviation in the IA group versus the stay in the EA group was 4 ± 6 vs 4 ± 7 days in the study of Hellan et al. [30]; 5.3 ± 1.6 vs 7.6 ± 1.2 days in Fabozzi et al. [34]; 5 ± 1 vs 5 ± 1 days in Sacatizi et al. [27]; 8 ± 6 vs 9 ± 5.7 days in Chavez et al. [23]; 6.2 ± 1.1 vs 7.2 ± 1.3 days in Roscio et al. [28]; 6.6 ± 6.3 vs 5.8 ± 5.7 days in Lee et al. [31]; 6.3 ± 3.2 vs 6 ± 1.8 days in Magistro et al. [29]; and 7.4 ± 3.2 vs 8. 5 ± 9 days in Anamia et al. [22].
The number of patients to be included in this trial will be 140. This number will be divided equally for each arm of the study. This size was determined for the primary endpoint: days of hospital stay, assuming that the variability will be approximately 3 days (standard deviation). This value would give a coefficient of variation between 50 and 100%, according to consulted articles. It has also been estimated that the difference between the two arms of the study will be a minimum of 1.5 days. A possible number of losses that may not exceed 10% have also been considered.
Additionally, to replicate these calculations, the value for type I error must be specified by 5% (alpha = 0.05), bilateral approximation, and a minimum power of 80% (probability of type II error = 0.20).
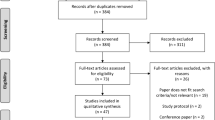
Recruitment and trial timeline
Patients from 18 to 90 years of age presenting with diagnosis of right colon cancer are studied for eligibility criteria by surgical consultants. The trial is explained, and informed consent must be signed before they can be included in the study. Once the screening and conditions for eligibility criteria are complete, they can be enrolled in the trial. If consultants note any reason for exclusion criteria, this will be recorded anonymously and presented at the end of the report. The trial will have 140 patients. They will be divided into two equal groups, and it is expected that the trial will be completed within 3 years. The trial will be finished within 30 days after the last surgical procedure.
Randomization, allocation concealment, and blinding
Randomization will be performed using an opaque, sealed envelope, and the patient will not know the surgical technique performed. The randomization list will be generated by the Methodology and Statistical Support Unit at the Institut de Recerca of Santa Creu i Sant Pau Hospital. The randomization envelopes are to be generated following the corresponding normalized work procedures and documenting their opening in each case. The randomization program has been explicitly designed for this project, in syntax with the SPSS package and by a researcher outside the clinical team of surgery. Once the randomization list has been made, individualized envelopes will be prepared to allow the patient to be assigned to their group.
The envelope will be opened in the operating room at the beginning of the surgical intervention, once the resectability of the lesion is verified as being oncologically radical and feasible.
Patients will be included in the study consecutively from the inclusion of the first eligible patient according to the selection criteria. When a patient is included in the study, the researcher will assign a patient code, which must be consecutive to the previous code assigned and take the date and time when the surgery is planned as a reference.
External validity
All patients with right colon cancer who are scheduled for an elective laparoscopic right hemicolectomy and who are not included or randomized in any other study will be registered. The registry will include information regarding date, gender, age, ASA classification, and type of surgery. In the case of any reason for non-inclusion or exclusion from the study, this will be recorded in the registry.
Data management
An operative case report form (CRF) including reasons for surgery and patient data, together with measurements from the surgical procedure, will be filled out by one of the investigators. For the hospitalization period, another surgeon will control the first postoperative days, and for each follow-up visit, another investigator will complete a CRF. This will be a single-blind study because patients will not know of the type of anastomosis they have. Participant names and collected data are subject to medical confidentiality. In the case of withdrawal, collected data will be erased. A logistic database with patient’s complete ID will be used and kept within a separate system from the result database with all study information. Data will be entered into the CRF as soon as possible after data retrieval. At the end of the trial, the original CRFs and final database will be archived by the principal investigator, who is responsible for providing data to trial investigators.
Statistical analysis
Initially, a comparative analysis will be carried out between the two groups to evaluate whether they are comparable with each other. The categorical variables will be described by the number of cases and their percentage for each group, while inference will be described with contingency tables and the corresponding chi-square test. The quantitative variables will be described by averaging their standard deviation and the inference comparison with the t test of independent data.
A multivariate approach will also be used for the primary endpoint, including those variables that are clinically relevant and those where a bivariate approach has shown a tendency; this model will be a multiple linear regression model. In all cases, the level of significance will be the usual 5% (alpha = 0.05). The analyses will be carried out using the statistical package SPSS.
Auditing
Both the investigator and the auditor will allow direct access to the data or CRFs to perform the monitoring, the audit, the review by the research institute, and inspection of the trial by the health authorities if required.
Safety and reporting of serious adverse events
Serious adverse events (SAEs), defined according to the guidelines for good clinical practice by the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH-GCP), will be reported from the day of first enrolment until the end of the trial.
Dissemination policy
The results obtained from the clinical research will be reviewed and discussed by the research team and the research institute for later publication, either in the form of a conference, communication in congresses, or publication.
Discussion
The advent of laparoscopic surgery has been a technical breakthrough in colorectal surgery, facilitating faster recovery for patients, lowering morbidity, and improving esthetic results when compared to traditional open surgery. In recent years, minimally invasive surgery has become a major focus of development, with the aim of causing the least possible impact on the patient and allowing the earliest possible recovery.
Findings from several studies performing intracorporeal anastomosis in patients with right colon cancer indicate that this approach is superior to extracorporeal anastomosis in terms of intestinal recovery, surgical wound size, surgical wound infection, eventration, esthetic results, analgesic requirements, hospital stay, and morbidity. All these important factors could enhance postoperative recovery and decrease the impact on the patients’ quality of life.
However, most of the studies to date are retrospective, non-randomized trials. We thus propose a prospective randomized trial in order to demonstrate the superiority of IA over EA.
Trial status
The trial is currently ongoing at Hospital de la Santa Creu i Sant Pau in Barcelona, Spain, and it is planned that is should be completed within 3 years, depending on the volume of patients.
References
Torre L, Bray F, Siegel R, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global Cancer Statistics, 2012. CA Cancer J Clin 65:87–108
El-Shami K, Oeffinger K, Erb N, Willis A, Bretsch J, Pratt-Chapman M, Cannady R, Wong S, Rose J, Barbour A, Stein K, Sharpe K, Brooks D, Cowens-Alvarado R (2015) American Cancer Society colorectal cancer survivorship care guidelines. CA Cancer J Clin 65:428–455
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pâlman L, Cuesta MA, Msika S, Morino M, Lacy AM, COLOR study group (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Guillou P, Quirke P, Thorpe H, Walker J, Jayne D, Smith A, Heath R, Brown J (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASSICC trial): multicenter, randomized controlled trial. Lancet 365:1718–1726
Simillis C, Purkayastha S, Yamamoto T, Strong SA, Darzi AW, Tekkis PP (2007) A meta-analysis comparing conventional end-to-end anastomosis vs other anastomotic configurations after resection in Crohn’s disease. Dis Colon Rectum 50:1674–1687
Docherty JG, McGregor JR, Akyol AM, Murray GD, Galloway DJ, West of Scotland and Highland Anastomosis Study Group (1995) Comparison of manually constructed and stapled anastomoses in colorectal surgery. Ann Surg 221:176–184
Kracht M, Hay J-M, Fagniez P-L, Fingerhut A (1993) Ileocolonic anastomosis after right hemicolectomy for carcinoma: stapled or hand-sewn? Int J Colon Dis 8:29–33
MacRae HM, McLeod RS (1998) Handsewn vs stapled anastomoses in colon and rectal surgery: a meta-analysis. Dis Colon Rectum 41(2):180–189
Choy PYG, Bisset IP, Docherty JG, Parry BR, Merrie A, Fitzgerald A (2011) Stapled versus handsewn methods for ileocolic anastomoses (Review). Cochrane Database Syst Rev (9):CD004320. https://doi.org/10.1002/14651858.CD004320.pub3
Frasson M, Granero-Castro P, Ramos J, Flor-Lorente B, Braithwaite M, Martínez E, Álvarez J, Codina A, Espí A, García-Granero E (2016) Risk factors for anastomotic leak and postoperative morbidity and mortality after elective right colectomy for cancer: results from a prospective, multicentric study of 1102 patients. Int J Color Dis 31:105–114
Ibañez N, Abrisqueta J, Luján J, Hernández Q, Parrilla P (2017) Isoperistaltic versus antiperistaltic side-to-side anastomosis after right laparoscopic hemicolectomy for cancer (ISOVANTI) trial: study protocol for a randomised clinical trial. Int J Color Dis 32:1349–1356
Cirocchi R, Trastulli S, Farinella E, Guarino S, Desiderio J, Boselli C, Parisi A, Noya G, Slim K (2013) Intracorporeal versus extracorporeal anastomosis during laparoscopic right hemicolectomy – systematic review and meta-analysis. Surg Oncol 22:1–13
Feroci F, Lenzi E, Garzi A, Vannucchi A, Cantafio S, Scatizzi M (2013) Inracorporeal versus extracorporeal anastomosis after laparoscopic right hemicolectomy for cancer: a systematic review and meta-analysis. Int J Color Dis 28:1177–1186
Tarta C, Bishawi M, Bergamaschi R (2013) Intracorporeal ileocolic anastomosis: a review. Tech Coloproctol 17:479–485
Carnuccio P, Jimeno J, Pares D (2014) Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Tech Coloproctol 18:5–12
Wu Q, Jin C, Hu T, Wei M, Wang Z (2017) Intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A 27:348–357
van Oostendorp S, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J, Tuynman J (2017) Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc 31:64–77
Marchesi F, Pinna F, Percalli L, Cecchini S, Ricco M, Costi R, Pattonieri V, Roncoroni L (2013) Totally laparoscopic right colectomy: theoretical and practical advantages over the laparo-assited approach. J Laparoendosc Adv Surg Tech A 23:418–424
Vergis AS, Steigerwald SN, Bhojani FD, Sullivan PA, Hardy KM (2015) Laparoscopic right hemicolectomy with intracorporeal versus extracorporeal anastomosis: a comparison of short-term outcomes. Can J Surg 58:63–68
Trastulli S, Coratti A, Guarino S, Piagnerelli R, Annecchiarico M, Coratti F, Di Marino M, Ricci F, Desiderio J, Cirocchi R, Parisi A (2015) Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicenter study. Surg Endosc 29:1512–1521
Anania G, Santini M, Scagliarini L, Marzetti A, Vedana L, Marino S, Gregorio C, Resta G, Cavallesco G (2012) A totally mini-invasive approach for colorectal laparoscopic surgery. World J Gastroenterol 18:3869–3874
Chaves JA, Idoate CP, Fons JB, Oliver MB, Rodriguez NP, Delgado AB, Lizoain JLH (2011) A case-control study of extracorporeal versus intracorporeal anastomosis in patients subjected to right laparoscopic hemicolectomy. Cir Esp 89:24–30
Kisielinski K, Conze J, Murken H, Lenzen NN, Klinge U, Schumpelick V (2004) The Pfannenstiel or so called “bikini cut”: still effective more than 100 years after first description. Hernia 8:177–181
Singh R, Omiccioli A, Hegge S, McKinley C (2008) Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 22:2596–2600
Winslow ER, Fleshman JW, Birnbaum EH, Blunt LM (2002) Wound complications of laparoscopic vs open colectomy. Surg Endosc 16:1420–1425
Scatizzi M, Kroning KC, Borrelli A et al (2010) Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study. World J Surg 34:2902–2908 21
Roscio F, Bertoglio C, De Luca A et al (2012) Totally laparoscopic versus laparoscopic assisted right colectomy for cancer. Int J Surg 10:290–295 22
Magistro C, Lernia SD, Ferrari G, Zullino A, Mazzola M, de Martini P, de Carli S, Forgione A, Bertoglio CL, Pugliese R (2013) Totally laparoscopic versus laparoscopic-assisted right colectomy for colon cancer: is there any advantage in short-term out- comes? A prospective comparative assessment in our center. Surg Endosc 27:2613–2618
Hellan M, Anderson C, Pigazzi A (2009) Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS 13:312–317
Lee KH, Ho J, Akmal Y, Nelson R, Pigazzi A (2013) Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc 27:1986–1990
Franklin ME Jr, Gonzalez JJ Jr, Miter DB et al (2004) Laparoscopic right hemicolectomy for cancer: 11-year experience. Rev Gastroenterol Mex 69(Suppl 1):65–72 30
Milone M, Elmore U, Di Salvo E et al (2015) Intracorporeal versus extracorporeal anastomosis. results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc 29:2314–2320
Fabozzi M, Allieta R, Contul RB, Grivon M, Millo P, Lale-Murix E, Nardi M (2010) Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc 24:2085–2091
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught C, Macfie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O, Enhanced Recovery After Surgery (ERAS) Society, for Perioperative Care, European Society for Clinical Nutrition and Metabolism (ESPEN), International Association for Surgical Metabolism and Nutrition (IASMEN) (2013) Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS((R))) society recommendations. World J Surg 37(2):259–284
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study will rigorously follow the international ethical recommendations for research and clinical trials in humans. Likewise, the standards contained in the Declaration of Helsinki will be guaranteed and will be developed in accordance with the protocol and standardized work procedures.
The ethical approval of this study has been obtained from the ethics committee at Hospital de la Santa Creu i Sant Pau and the research institute.
Additional information
Protocol version
This manuscript presents the second version of the full study protocol issued on May 15, 2015. Modifications to the protocol will be reported to all investigators, all trial participants, the local ethics committee, and the journal.
Rights and permissions
About this article
Cite this article
Bollo, J., Salas, P., Martinez, M.C. et al. Intracorporeal versus extracorporeal anastomosis in right hemicolectomy assisted by laparoscopy: study protocol for a randomized controlled trial. Int J Colorectal Dis 33, 1635–1641 (2018). https://doi.org/10.1007/s00384-018-3157-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3157-9