Abstract
Purpose
The relationship between emergency colon cancer resection and long-term oncological outcomes is not well understood. Our objective was to characterize the impact of emergency resection for colon cancer on disease-free and overall patient survival.
Methods
Data on patients undergoing resection for colon cancer from 2006 to 2015 were collected from a prospectively maintained clinical and administrative database. The median follow-up time was 4.4 years. Cox proportional hazards models were used to estimate the hazard ratios for recurrence and death for patients treated with surgery for an emergent presentation. Differences in initiation of, and timeliness of, adjuvant chemotherapy between emergently and electively treated patients were also examined.
Results
Of the 1180 patients who underwent resection for stages I, II, or III colon cancer, 158 (13%) had emergent surgery. After adjustment for patient, tumor, and treatment characteristics, the HR for recurrence was 1.64 (95% CI 1.12–2.40) and for death was 1.47 (95% CI 1.10–1.97). After adjustment for tumor characteristics, patients who underwent emergency resection were similarly likely to receive adjuvant chemotherapy (OR 1.1; 95% CI 0.70–1.76). The time from surgery to initiation of adjuvant chemotherapy was also similar between the groups.
Conclusions
Emergency surgery for localized or regional colon cancer is associated with a greater risk of recurrence and death. This association does not appear to be due to differences in adjuvant treatment. A focus on screening and colon cancer awareness in order to reduce emergency presentations is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is a major cause of cancer-related mortality worldwide. Survival is mainly dependent on disease stage, and modern treatment of patients with localized or regional disease achieves 70–90% 5-year survival [1]. Despite improvements in prevention and early detection, previous studies report that emergency presentation of colorectal cancer, including obstruction, perforation, and hemorrhage, comprises 26% of all colorectal cancer presentations [2].
The healthcare burden of emergent CRC presentation is considerable. Patients who undergo emergency surgery spend greater than 50% more days in hospital than those who do not and healthcare costs are significantly higher for their treatment [3]. Moreover, these patients may be at significantly higher risk of worse short- and long-term survival outcomes. Several studies have shown that postoperative morbidity is more common following emergent surgery compared to elective surgery, with higher rates of medical and surgical complications [4,5,6]. This has been associated with a greater need for re-operation, longer hospital stay, and an observed perioperative mortality incidence that is four to ten times higher amongst emergently treated individuals [2, 4, 7,8,9,10,11,12,13,14,15,16,17].
An association between emergency surgery and long-term outcomes is less well established. While it is clear that overall mortality is higher for those treated emergently, it remains unknown whether the surgical nature itself predisposes patients to lower long-term survival even after considering differences in patient characteristics [10, 11, 18, 19]. Recent studies with conflicting results have contributed to the uncertainty. A single-center cohort study which accounted for differences in patient characteristics using propensity score matching found no evidence of worse oncologic outcomes after urgent operation for colorectal cancer [20]. In contrast, a study using data from the National Cancer Data Base found that emergent colectomies were associated with 13% greater hazard of overall mortality, but disease-free survival was not examined [21].
Further investigation of the relationship between emergency surgery for colon cancer and oncological outcomes is warranted. If those who undergo emergency surgery have earlier tumor recurrence and lower survival after adjustment for differences in patient and tumor characteristics, then resources should be better directed towards screening for symptoms of impending colonic obstruction, bleeding, or perforation, as well as timely adjuvant treatment, follow-up, and cancer surveillance. Using our institutional colorectal cancer database, we conducted an observational study comparing the long-term survival of emergently and electively treated patients.
Methods
Study population and design
Data was prospectively collected in a clinical and administrative database maintained at the London Regional Cancer Centre in London, Ontario, Canada. The database was designed for administrative and research purposes with approval of the Western University Research Ethics Board (REB), and this specific study was also approved. Demographic, diagnostic, pathologic, treatment, and follow-up data on patients who underwent surgical resection for colorectal cancer from 2006 until present is included within the database. Follow-up data is recorded during routine follow-up appointments. If patients failed to attend the appointments, attempts were made to contact their family physician in order to determine whether recurrence or death had occurred. Quarterly quality assessment data checks and random chart audits are routinely performed to ensure accuracy of the data.
For this study, we took a subset cohort from the institutional database over a 10-year period (2006–2015) to ensure complete treatment and postoperative data for all cohort patients. The database included patients who underwent resection with curative intent for colon cancer, excluding those with rectal cancer and those who underwent diversion (i.e., ileostomy, colostomy) without resection of the tumor. We excluded all of the patients who were identified as having a tumor located in the rectum, those who underwent an abdominoperineal resection, and those who received neoadjuvant chemotherapy or radiation. We limited the study to patients who completed staging, and who had stages I, II, and III cancer. From an initial database containing 2253, the final cohort for analysis included 1180 patients, 158 (13%) of whom underwent emergency resection (Fig. 1).
Variables
Exposure was defined as having an emergency colon resection for obstruction, intestinal bleeding, and/or perforation caused by colon cancer, as recorded by the surgeon. Unexposed individuals were those who underwent an electively scheduled operation for colon cancer. The primary outcome was disease-free survival. Disease-free survival was defined as the time from surgical resection to the date of cancer recurrence as diagnosed during surveillance or symptom-directed investigations. Patients who died without recurrence or who were lost to follow-up without evidence of recurrence were censored on the date of death or date of last follow-up. The secondary outcome was overall survival which was defined as the time from surgical resection to the date of death, regardless of cause.
A number of variables were considered as potential confounders of the relationship between emergent resection and long-term survival. Various socioeconomic factors may be associated with a greater tendency to require emergent colectomy and may also impact survival [20,21,22]. We used Forward Sortation Areas (FSAs), defined by the first three digits of a patient’s postal code, in order to account for complex differences in geographic, social, and economic characteristics. Geographic-based measures, such as FSA, can be used as surrogates for individual-level health disparities when individual data is not available [23]. Emergent surgery is also more likely for patients with advanced cancers, defined by higher stage and potentially other high-risk pathologic features [8, 20]. We therefore recorded information on various pathological factors including stage, grade, lymph node yield, lymphovascular invasion, venous invasion, and perineural invasion. We also considered potential differences in treatment including margin status and treatment with adjuvant chemotherapy and/or radiation.
Statistical methods
Characteristics for exposed and unexposed patients were tabulated and compared descriptively, where patients who underwent emergency surgery were termed “exposed“ and patients who underwent elective surgery were termed “unexposed.“ Frequencies of margin positivity and inadequate lymph node yield were compared using chi-squared tests of independence. Unadjusted disease-free and overall survival was estimated using the Kaplan-Meier method, stratified by exposure status. Cox proportional hazards models, with stratification by FSA, were used to estimate hazards ratios (HRs) for the primary and secondary outcomes. Stratification, rather than regression adjustment, was performed for FSA so that the proportional hazards assumption could be relaxed for FSAs, and to improve efficiency of the model by reducing the number of parameters estimated. Models were also adjusted for demographic, treatment, and pathologic characteristics. Missing information for potential confounders (proportion of missing data is displayed in Table 1) was considered missing at random, conditional on values of other variables in the dataset. Multiple imputation of continuous and categorical variables was performed using additive regression, bootstrapping, and predictive mean matching to impute 100 complete datasets on which the analyses were performed and results combined [24, 25].
We used a logistic regression model, adjusted for tumor characteristics (stage, grade, lymphovascular invasion, venous invasion, and perineural invasion) to estimate the odds of receiving adjuvant chemotherapy, comparing emergently and electively treated patients. A cox proportional hazards model was used to compare time to initiation of adjuvant chemotherapy from time of surgery.
All statistical analysis was performed using R Statistical Software, Version 3.4.2.
Results
Between 2006 and 2015, there were 1180 patients who underwent resection for stages I, II, or III colon cancer. Of those patients, 158 (13%) had emergent surgery. Patient, tumor, and treatment characteristics are displayed in Table 1. The median follow-up time was 4.6 years.
Patients who required emergency resection tended to have tumors with more advanced stage and worse pathologic features. Margin positivity and proportion of patients with inadequate lymph node yields were similar in both groups (p = 0.23 and 0.27, respectively).
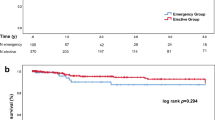
The proportion of recurrences [46 (29%) vs. 159 (16%)] and deaths [81 (51%) vs. 339 (33%)] during the entire follow-up period was higher for patients who underwent emergency resection compared to those who had elective surgery. The 5-year disease-free survival for those who had emergency surgery was 63% (95% CI 54–72%) compared to 83% (95% CI 81–86%) for patients who had elective surgery. Similarly, those who had emergent resection had poorer 5-year overall survival [50% (95% CI 42–59%) vs. 72% (95% CI 69–75%)]. Kaplan-Meier survival curves for disease-free and overall survival, stratified by exposure status, are displayed in Fig. 2.
In unadjusted analysis, the hazard ratio for recurrence was 2.34 (95% CI 1.68–3.24) for patients who underwent emergency resection compared to those who had elective resection. After adjustment for patient, tumor, and treatment characteristics, the HR was 1.64 (95% CI 1.12–2.40). Similarly, patients who underwent emergency resection had poorer overall survival with a HR of 1.47 (95% CI 1.10–1.97) even after adjustment for confounding (Table 2).
We explored whether age modified the effect of emergency resection on survival by examining whether continuous age interacted significantly with the primary exposure in our fully adjusted models. For both disease-free survival and overall survival, there was no evidence of a significant interaction with age.
We also examined whether there were differences in initiation of adjuvant chemotherapy amongst emergently and electively treated patients. After adjustment for tumor characteristics, patients who underwent emergency resection were not significantly more likely to receive adjuvant chemotherapy (OR 1.1; 95% CI 0.70–1.76; p = 0.65). The time from surgery to initiation of adjuvant chemotherapy was also similar between the groups with a median of 9.3 weeks (95% CI 9.0–9.9 weeks) for electively treated patients, and 9.6 weeks (95% CI 8.9–10.6 weeks) for emergently treated patients.
Discussion
This study identified that emergency resection for colon cancer was associated with worse long-term oncological outcomes. Emergency surgery was a significant predictor of both recurrence and death. Those treated emergently had similar odds of receiving adjuvant chemotherapy and did not have evidence of a delay to initiation of chemotherapy compared to electively treated patients.
Our study has a number of strengths. The institutional database represents all colorectal cancer patients treated in our region and is updated regularly, with routine audits, and has a high degree of accuracy. We were therefore able to collect data on and adjust for several important pathological variables. We were also able to account for potential differences in patient characteristics due to stratification by postal code defined regions as a surrogate for socioeconomic status. A patient’s place of residence provides information on various socioeconomic factors, as well as geographic ones such as distance to the nearest healthcare facility, which could be associated with reduced access to timely care.
The main limitations of this study are its observational design and the potential for unmeasured confounding. While we adjusted for place of residence as a proxy for socioeconomic factors, we did not have access to individualized patient data on socioeconomic status which may not be completely captured within FSAs. We also did not have information available regarding co-morbidities which may confound the relationship between exposure and overall survival. Moreover, while we designed the study to be limited to colon cancer cases, it is possible that some patients with upper rectal tumors were not excluded. Adjustment for procedure type, specifically low anterior resection, was intended to control for potential differences in the distribution of patients with rectal tumors amongst groups. Lastly, our exposure definition includes patients who were classified as emergently treated by the surgical team. As such, there may be some patients who had very urgent, but not emergent, symptoms and were treated using elective operating room resources and not captured as emergency presentations, and the results of our study cannot be generalized to them.
Although an observational design may result in bias due to residual confounding, an experimental study addressing this question is impossible, so improved data collection and granularity would be necessary in order to improve future analyses. Since observational studies rely on exchangeability conditional on confounders, it is questionable whether a causal effect of emergency surgery on survival can be estimated. Patients who have sufficient causes requiring emergency surgery cannot be treated electively, and those who do not have the set of conditions which require emergency surgery will not be treated emergently. As such, a study which is able to stratify on all variables that indicate the need for emergency surgery will not have electively and emergently treated patients within the same strata. Nonetheless, associational relationships between emergency surgery and survival, and the factors, such as timeliness of adjuvant therapy, which might drive such associations, are important to determine in order to improve the care of emergently treated patients.
We hypothesized that emergently treated patients may be less likely to have an adequate oncological resection, receive timely adjuvant chemotherapy, have routine surveillance investigations, and be more likely to present with tumors that have aggressive pathological features not accounted for in our statistical models. Further, more work is necessary in order to understand the ways, if any, that tumors requiring emergency treatment are biologically different than those treated electively.
In our study, patients treated emergently were not significantly more likely to have positive resection margins or an inadequate lymph node harvest. Previous studies have shown mixed results, with some reporting that patients undergoing emergency surgery were more likely to have an inadequate oncological resection [21, 26, 27]. Other studies examining lymph node yields in emergency versus elective resections corroborate the findings of this present study with no increased risk of nodal understaging in emergency cases [20, 28]. Some investigators have also reported that patients undergoing emergency surgery are less likely to receive adjuvant therapy; however, our study does not support their findings since emergently treated individuals in our cohort had similar odds of receiving adjuvant chemotherapy and similar time to initiation of the treatment [29]. In the non-emergency surgery group, the 9-week start time may be a system resource issue relating to timely access to medical oncology consultation, as it is longer than we would hope in the elective setting. This is a current area of quality improvement in our center.
In the absence of evidence suggesting less timely or adequate oncological treatment for patients who undergo emergency surgery, resources would best be allocated towards improving awareness of symptoms of impending colonic emergencies and screening for polyps before cancers develop. Implementation of a national bowel cancer awareness campaign in the UK was associated with a 62.5% decrease in the number of patients with colorectal cancer presenting as an emergency, and similar campaigns may have success elsewhere [30]. Other studies have demonstrated reductions in emergency presentations with colorectal cancer amongst patients who comply with screening, even those who only completed a single fecal occult blood test [31,32,33]. These findings provide promising evidence that population-level interventions can reduce the incidence of emergency CRC presentations.
Conclusion
Despite no apparent differences in adjuvant treatment, patients who underwent emergency resection for colon cancer had higher rates of recurrence and death compared to patients who had elective surgery. Emergency resection appears to be associated with poorer long-term outcomes, and a focus on screening and bowel cancer awareness in order to reduce emergency presentations is warranted.
References
Haggar F, Boushey R (2009) Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg 22:191–197
McPhail S, Elliss-Brookes L, Shelton J, Ives A, Greenslade M, Vernon S, Morris EJA, Richards M (2013) Emergency presentation of cancer and short-term mortality. Br J Cancer 109:2027–2034
Shah NA, Halverson J, Madhavan S (2013) Burden of emergency and non-emergency colorectal cancer surgeries in West Virginia and the USA. J Gastrointest Cancer 44:46–53
Chen Y-L, Chang W-C, Hsu H-H, Hsu C-W, Lin Y-Y, Tsai S-H (2013) An evolutionary role of the ED: outcomes of patients with colorectal cancers presenting to the ED were not compromised. Am J Emerg Med 31:646–650
Sjo OH, Larsen S, Lunde OC, Nesbakken A (2009) Short term outcome after emergency and elective surgery for colon cancer. Color Dis 11:733–739
Iversen LH, Antonsen S, Laurberg S, Lautrup MD (2009) Therapeutic delay reduces survival of rectal cancer but not of colonic cancer. Br J Surg 96:1183–1189
Bass G, Fleming C, Conneely J, Martin Z, Mealy K (2009) Emergency first presentation of colorectal cancer predicts significantly poorer outcomes: a review of 356 consecutive Irish patients. Dis Colon rectum 52:678–684
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg 91:605–609
In collaboration with the West of Scotland Colorectal Cancer Managed Clinical Network, Oliphant R, Mansouri D, Nicholson GA, McMillan DC, Horgan PG, Morrison DS (2014) Emergency presentation of node-negative colorectal cancer treated with curative surgery is associated with poorer short and longer-term survival. Int J Color Dis 29:591–598
Chiarugi M, Galatioto C, Panicucci S, Scassa F, Zocco G, Seccia M (2007) Oncologic colon cancer resection in emergency: are we doing enough? Surg Oncol 16:73–77
Biondo S, Martí-Ragué J, Kreisler E, Parés D, Martín A, Navarro M, Pareja L, Jaurrieta E (2005) A prospective study of outcomes of emergency and elective surgeries for complicated colonic cancer. Am J Surg 189:377–383
Anderson JH, Hole D, McArdle CS (1992) Elective versus emergency surgery for patients with colorectal cancer. Br J Surg 79:706–709
Smothers L, Hynan L, Fleming J, Turnage R, Simmang C, Anthony T (2003) Emergency surgery for colon carcinoma. Dis Colon rectum 46:24–30
Cuffy M, Abir F, Audisio RA, Longo WE (2004) Colorectal cancer presenting as surgical emergencies. Surg Oncol 13:149–157
Coco C, Verbo A, Manno A, Mattana C, Covino M, Pedretti G, Petito L, Rizzo G, Picciocchi A (2005) Impact of emergency surgery in the outcome of rectal and left colon carcinoma. World J Surg 29:1458–1464
Formisano V, Di Muria A, Connola G, Cione G, Falco L, De Angelis CP, Angrisani L (2014) Our experience in the management of obstructing colorectal cancer. Ann Ital Chir 85:563–568
Kelly M, Sharp L, Dwane F, Kelleher T, Comber H (2012) Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. BMC Health Serv Res 12:77
Abdelrazeq AS, Scott N, Thorn C, Verbeke CS, Ambrose NS, Botterill ID, Jayne DG (2008) The impact of spontaneous tumour perforation on outcome following colon cancer surgery. Color Dis 10:775–780
Jiang JK, Lan YT, Lin TC, Chen WS, Yang SH, Wang HS, Chang SC, Lin JK (2008) Primary vs. delayed resection for obstructive left-sided colorectal cancer: impact of surgery on patient outcome. Dis Colon rectum 51:306–311
Weixler B, Warschkow R, Ramser M, Droeser R, von Holzen U, Oertli D, Kettelhack C (2016) Urgent surgery after emergency presentation for colorectal cancer has no impact on overall and disease-free survival: a propensity score analysis. BMC Cancer 16:208
Xu Z, Becerra AZ, Aquina CT, Hensley BJ, Justiniano CF, Boodry C, Swanger AA, Arsalanizadeh R, Noyes K, Monson JR, Fleming FJ (2017) Emergent colectomy is independently associated with decreased long-term overall survival in colon cancer patients. J Gastrointest Surg 21:543–553
Pruitt SL, Davidson NO, Gupta S, Yan Y, Schootman M (2014) Missed opportunities: racial and neighborhood socioeconomic disparities in emergency colorectal cancer diagnosis and surgery. BMC Cancer 14:927
Denny K, Davidson MJ (2012) Area-based socio-economic measures as tools for health disparities research, policy and planning. Can J Public Health 103:S4–S6
Harrell Jr FE, Harrell Jr MFE (2018) Package ‘Hmisc.’ R Found. Stat. Comput
Moons KGM, Donders RART, Stijnen T, Harrell FE (2006) Using the outcome for imputation of missing predictor values was preferred. J Clin Epidemiol 59:1092–1101
Amri R, Bordeianou LG, Sylla P, Berger DL (2014) Treatment delay in surgically-treated colon cancer: does it affect outcomes? Ann Surg Oncol 21:3909–3916
Kye B-H, Lee YS, Cho H-M, Kim JG, Oh ST, Lee IK, Kang WK, Ahn CH, Lee SC, Park JK, Kim HJ (2016) Comparison of long-term outcomes between emergency surgery and bridge to surgery for malignant obstruction in right-sided colon cancer: a multicenter retrospective study. Ann Surg Oncol 23:1867–1874
Patel SV, Patel SVB, Brackstone M (2014) Emergency surgery for colorectal cancer does not result in nodal understaging compared with elective surgery. Can J Surg J Can Chir 57:349–353
Ha GS, Kim YW, Choi EH, Kim IY (2017) Factors associated with the lack of adjuvant chemotherapy following curative surgery for stage II and III colon cancer: a Korean National Cohort Study. Anticancer Res 37:915–922
Pande R, Leung E, McCullough P, Smith S, Harmston C (2014) Impact of the United Kingdom national bowel cancer awareness campaign on colorectal services. Dis Colon rectum 57:70–75
Scholefield JH, Robinson MH, Mangham CM, Hardcastle JD (1998) Screening for colorectal cancer reduces emergency admissions. Eur J Surg Oncol 24:47–50
Libby G, Brewster DH, Steele RJC (2014) Impact of faecal occult blood test screening on emergency admissions and short-term outcomes for colorectal cancer: faecal occult blood test screening for colorectal cancer. Br J Surg 101:1607–1615
Hwang M-J, Evans T, Lawrence G, Karandikar S (2014) Impact of bowel cancer screening on the management of colorectal cancer. Color Dis 16:450–458
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The database was designed for administrative and research purposes with approval of the Western University Research Ethics Board (REB), and this specific study was also approved.
Rights and permissions
About this article
Cite this article
Wanis, K.N., Ott, M., Van Koughnett, J.A.M. et al. Long-term oncological outcomes following emergency resection of colon cancer. Int J Colorectal Dis 33, 1525–1532 (2018). https://doi.org/10.1007/s00384-018-3109-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3109-4