Abstract
Purpose
Cancer risk assessment for ulcerative colitis patients by evaluating histological changes through colonoscopy surveillance is still challenging. Thus, additional parameters of high prognostic impact for the development of colitis-associated carcinoma are necessary. This meta-analysis was conducted to clarify the value of aneuploidy as predictor for individual cancer risk compared with current surveillance parameters.
Methods
A systematic web-based search identified studies published in English that addressed the relevance of the ploidy status for individual cancer risk during surveillance in comparison to neoplastic mucosal changes. The resulting data were included into a meta-analysis, and odds ratios (OR) were calculated for aneuploidy or dysplasia or aneuploidy plus dysplasia.
Results
Twelve studies addressing the relevance of aneuploidy compared to dyplasia were comprehensively evaluated and further used for meta-analysis. The meta-analysis revealed that aneuploidy (OR 5.31 [95 % CI 2.03, 13.93]) is an equally effective parameter for cancer risk assessment in ulcerative colitis patients as dysplasia (OR 4.93 [1.61, 15.11]). Strikingly, the combined assessment of dysplasia and aneuploidy is superior compared to applying each parameter alone (OR 8.99 [3.08, 26.26]).
Conclusions
This meta-analysis reveals that aneuploidy is an equally effective parameter for individual cancer risk assessment in ulcerative colitis as the detection of dysplasia. More important, the combined assessment of dysplasia and aneuploidy outperforms the use of each parameter alone. We suggest image cytometry for ploidy assessment to become an additional feature of consensus criteria to individually assess cancer risk in UC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1925, the first case of rectal carcinoma in ulcerative colitis (UC) was described [1]. Since this observation, an increased incidence of colorectal carcinoma in UC has been reported in numerous scientific publications. Reports on the frequency of UC-associated carcinoma (UCC) vary from 0.2 to 34 % depending on age at diagnosis, extent and duration of UC as well as study design [2]. In a comprehensive meta-analysis by Eaden et al., the cumulative incidence for UCC was stated as 1.6 % after 10 years, 8.3 % after 20 years, and 18.4 % after 30 years of disease duration [3]. However, the actual risk for carcinoma development in UC is still a matter of debate [4–7].
Histopathogenesis of UC-associated colorectal carcinogenesis is widely believed to involve a stepwise progression from inflamed and hyperplastic epithelium to flat dysplasia and finally adenocarcinoma [8, 9]. In contrast to sporadic colorectal cancer, UCC-related tumor development includes chronic inflammation, injury, dysplasia, and carcinoma, which arise without the formation of a well-defined adenoma [10].
To detect premalignant lesions or UCC at early stages, colonoscopy surveillance is the gold standard as stated in various national and international guidelines [11–15]. However, the sensitivity to detect premalignant lesions via endoscopical screening for dysplasia and cancer is rather low: Rubin et al. demonstrated that only 72 % of all colitis-related premalignant lesions were detected [16]. Furthermore, a subgroup of patients develop UCC after a short disease duration, e.g., Lutgens et al. could demonstrate that 21 % of 89 examined patients developed UCC at a time before cancer surveillance was recommended [17]. Strikingly, we recently found a high rate of preoperatively undetected high-grade intraepithelial neoplasia and carcinoma in UC patients with long-standing inflammation of the colon in a cohort of patients undergoing proctocolectomy [18].
At present, biopsies are analyzed for neoplastic changes of the intestinal mucosa (dysplasia) in order to assess the individual cancer risk. The severity of dysplasia usually is classified according to Riddell et al. [8]. However, the efficacy of surveillance programs based on histopathologic evaluation of dysplasia has been questioned for several reasons. Notably, the occurrence of dysplasia is not mandatory before an UCC develops [19–21]. Dysplasia is absent in 20–30 % of colectomy specimens containing cancer in UC [22]. Moreover, cancer risk assessment based on dysplasia as a marker is hampered by numerous methodical challenges. Many early lesions do not produce endoscopically recognizable abnormalities [23]. Due to the large area of the colon and a patchy distribution of dysplasia, sampling errors by the endoscopist are likely to occur. According to international guidelines, at least four biopsies per every 10 cm should be taken around the colon plus biopsies of macroscopically dysplastic lesions [24]. Nevertheless, a typical biopsy represents less than 0.05 % of the total colonic surface, and the number of biopsies taken by endoscopists in routine practice is often less [25, 26]. In addition to difficulties in sample collection, histopathological evaluation of dysplastic lesions in the inflamed colon mucosa is highly subjective. Classification of lesions according to Riddell et al. [8] is hampered by interindividual and intraindividual variation [19, 27–32]. Therefore, additional reliable parameters of high prognostic impact in individual risk assessment for development of UCC are necessary.
In 1984, Hammarberg et al. reported changes of the nuclear DNA content in colorectal biopsies, followed by several other publications addressing the possible use of ploidy analysis for the assessment of malignancy development [33]. Although an increased incidence of aneuploidy in correlation to an advancing degree of dysplastic mucosal changes has been observed [34–37], discordant occurrence of dysplasia and aneuploidy has been reported [38–40]. Particularly, aneuploidy has been shown to precede dysplasia by 1–2.5 years [23]; thus, the theory of a stepwise cancer genesis with the occurrence of genetic instability at early stages of tumor development resulting in aneuploid cells that transform via dysplasia toward malignancy has been evolved. Additionally, aneuploidy has been found frequently in non-malignant mucosa adjacent to UCCs and seems to be irrespective of dysplasia [41].
The value of ploidy measurements for the prediction of esophageal, gastric, and colorectal tumors was reviewed some years ago by Grabsch et al. [42]. They found aneuploid cell populations in biopsies from UC patients to be prevalent in 6–71.4 % of cases and an increase of aneuploid lesions with the extent of the disease as well as the disease duration [43, 44]. However, most of the chosen studies lack the consideration of individual UC patients progressing to UCC in comparison with ploidy development over time, although in general, the samples descended from surveillance programs. The potential value of ploidy assessment in cancer risk assessment during surveillance is not even considered in most international guidelines [11–15].
Thus, this meta-analysis focuses on the value of aneuploidy for individual cancer risk assessment compared with the actual gold standard of evaluating neoplastic mucosal changes in UC.
Material and methods
Search and extraction process
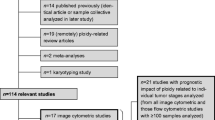
In January 2016, the PubMed database was searched in order to identify relevant studies without any restrictions in terms of the year of publication based on the following terms: “ulcerative colitis + cancer prognosis + ploidy,” “ulcerative colitis + risk assessment + ploidy,” “ulcerative colitis + surveillance + ploidy,” “ulcerative colitis + cancer prognosis + cytometry,” “ulcerative colitis + risk assessment + cytometry,” “ulcerative colitis + surveillance + cytometry,” and “ulcerative colitis + aneuploidy.” Each search was limited to studies on humans published in English. Studies on patients after colectomy and studies on inflammatory bowel diseases other than UC were excluded. There were 173 studies matching these criteria. Among these, surveillance studies considering the ploidy status as well as the actual risk assessment by rating neoplastic mucosal changes for the individual cancer risk during disease development were selected. In total, 12 studies fulfilled the requirements and were included (Table 1) [23, 38, 44–53]. Three of these studies were retrospective; the others were follow-up or prospective studies. In six included studies, patients were preselected for certain specific phenotypes including the presence of dysplasia and/or aneuploidy (Table 3). The remaining six studies were carried out on patients chosen for having UC for a certain duration or extent (Table 2). To allow a simplified comparison of the different study designs, the respective surveillance periods, the intervals of colonoscopy as well as the numbers of biopsy sites and the analysis methods with regard to sample preparation, staining, and evaluation criteria are listed in tabular form (Table 1). The histopathological rating of the biopsies was performed according to Riddell et al. [8] in all included studies, but there were variations in the assessment of the ploidy status with regard to method (flow cytometry (FC) or image cytometry (IC)), sample preparation (fresh, frozen, paraffin embedded) as well as staining and evaluation procedures (Table 1).
Meta-analysis
In order to address whether aneuploidy, dysplasia, or a combination of aneuploidy and dysplasia is associated with the occurrence of an UCC, the frequencies of UCCs, aneuploidy, and dysplasia of each study were summarized and a meta-analysis was conducted on these data. For each study, odds ratios (OR) and appropriate 95 % confidence intervals were calculated. The ORs were combined by assuming random effect models. A test for heterogeneity as well as for publication bias was performed. A p value <0.05 was considered significant. The results were illustrated in forest plots (Figs. 1, 2, and 3). Statistical analysis was performed by using the software R version 2.12.2 (package metafor).
Forest plot of the OR for detection of dysplasia and UCC occurrence. Studies are listed in order of their year of publication. The 95 % CI is shown for each study (horizontal line). The size of the square symbol is proportional to the weight of the study in the pooled estimate by using a random effects model. The diamond and the broken line represent the overall estimate including all studies and the according 95 % CI, respectively
Forest plot of the OR for detection of aneuploidy and UCC occurrence. Studies are listed in order of their year of publication. The 95 % CI is shown for each study (horizontal line). The size of the square symbol is proportional to the weight of the study in the pooled estimate by using a random effects model. The diamond and the broken line represent the overall estimate including all studies and the according 95 % CI, respectively
Forest plot of the OR for detection of dysplasia plus aneuploidy and UCC occurrence. Studies are listed in order of their year of publication. The 95 % CI is shown for each study (horizontal line). The size of the square symbol is proportional to the weight of the study in the pooled estimate by using a random effects model. The diamond and the broken line represent the overall estimate including all studies and the according 95 % CI, respectively
Results
Association of DNA aneuploidy and dysplasia in surveillance colonoscopy
Numerous studies concerning aneuploidy in UC have been published. However, only a small number of these have addressed the relevance of the ploidy status regarding the individual cancer risk during surveillance in comparison to the risk assessment by evaluating neoplastic mucosal changes (Table 1).
The first study was performed in 1987 by Lofberg et al. who focused on the correlation of aneuploidy with histological dysplasia during surveillance colonoscopy in UC patients [52]. The prospective study was comprised of 53 patients, and aneuploidy was detected in five of those patients (Table 2). There was aneuploidy but no dysplasia in one patient. Four of the patients also had dysplasia in the aneuploid mucosa. Aneuploidy was detectable in one of those patients before dysplasia was macroscopically diagnosable. In one patient, low-grade dysplasia evolved into high-grade dysplasia and adenocarcinoma was found after colectomy where aneuploidy had been detected before. In general, aneuploidy was detected multifocally but not necessarily in the same location as dysplasia. Additionally, eight patients had dysplastic lesions without detectable aneuploidy. Three of these patients had low-grade dysplasia, and five were indefinite for dysplasia.
In 1988, Rutegard et al. published a 3-year prospective study on 73 UC patients [51]. DNA aneuploidy was found in six patients, and there was aneuploidy but no dysplasia in two of these patients. In two patients, aneuploidy was found before detecting lesions classified as indefinite for dysplasia. No spatial relation between aneuploidy and dysplasia was observed. There were five patients without detectable aneuploidy presenting one carcinoma, one high-grade dysplasia, and three low-grade dysplasias.
The same group published a retrospective study on 23 patients preselected for dysplasia and indefinite mucosal changes [50] (Table 3). Eleven patients were indefinite for dysplasia; nine had low-grade dysplasia, and three had high-grade dysplasia. Aneuploidy was found in six of these patients. All of the patients with high-grade dysplasia had aneuploidy, and in one of these patients, aneuploidy preceded two diploid carcinomas.
Lofberg et al. followed up 59 patients with long-standing, total UC in a prospective surveillance program for 8 years [38]. Fifteen of these patients had aneuploid biopsies at least once (Table 2). Among these patients, aneuploidy was detected before development of definite dysplasia in six patients, simultaneously with development of dysplasia in another six patients, and after the development of dysplasia in one patient. The remaining two patients with a repeated finding of aneuploidy had no concomitant dysplasia. Remarkably, definite dysplasia developed in all six patients in which aneuploidy had been found before dysplasia after an average time of 2.7 years. During the follow-up period, aneuploidy spread throughout the locality with increasing duration of the disease but persisted in the same part of the colon.
Aneuploidy as a predictor of progression to dysplasia
In 1992, Rubin et al. published a prospective study on high-risk patients without dysplasia or cancer, who were identified by a prevalence study on 101 UC patients [23]. There was a significant trend for an increase of aneuploid lesions concordant with histological progression from indefinite for dysplasia to dysplasia to carcinoma in the prevalence study.
Out of the 101 UC patients, 25 high-risk patients (disease not confined to rectum and sigmoid, disease duration >8 years, or both) were prospectively examined by colonoscopy for at least 2 years. Six of the 25 patients progressed to dysplasia, and 5 of these 6 patients had aneuploidy preceding the finding of dysplasia by 1–2.5 years. The sixth patient had concurrent development of aneuploidy and dysplasia. Nineteen patients did not show aneuploidy at any time of follow-up. All of them had initially been negative for dysplasia; however, on termination of the follow-up, 15 patients were negative and 4 were indefinite for dysplasia. Rubin et al. concluded aneuploidy to be a significant predictor of progression to dysplasia and could show that considerably less biopsies are needed to detect aneuploidy compared with the histological finding of cancer. Ploidy assessment on up to 30 biopsies was needed to detect aneuploidy with 95 % confidence, whereas up to 64 biospies were needed to detect the highest degree of dysplasia with 95 % confidence. Rubin et al. concluded DNA ploidy measurement to be useful to identify aneuploidy in the absence of dysplasia as an indicator of an increased risk for development of dysplasia requiring a more frequent follow-up of the patients [23].
Aneuploidy measurement does replace detection of dysplasia
Befrits et al. published a follow-up study on 36 UC patients in 1994 [49]. The authors initially assessed DNA ploidy and histopathology, then performed annual colonoscopies for 10 years, and repeated the ploidy measurement after 10 years. Initially, 63 UC patients were included to the study, but 27 patients dropped out before the 10-year endpoint. One of those 27 patients received colectomy because of simultaneous finding of low-grade dysplasia and aneuploidy, and the colectomy specimen showed an adenocarcinoma in the same dysplastic/aneuploid area. None of the 36 patients who completed the 10-year follow-up had dysplasia on the first examination. Aneuploidy was initially detected in six of these patients. After 10 years, all 30 initially diploid patients still had no detectable aneuploidy, but low-grade dysplasia was found in 2 patients. Of the initial six aneuploid patients, neither aneuploidy nor dysplasia was found in two patients, one patient was reclassified as diploid, and three patients presented again with aneuploidy and in addition now presented also low-grade dysplasia. In accordance with Lofberg et al. [38], the authors suggest the simultaneous finding of aneuploidy and low-grade dysplasia to be an indication for surgical treatment since they also found one unexpected adenocarcinoma after colectomy.
Karlen et al. prospectively evaluated the mucin-associated sialyl-Tn (STn) antigen as a marker in cancer risk assessment in relation to dysplasia in 1998 [48]. The authors performed a matched case-control study on UC patients who underwent colectomy either for dysplasia (six cases) or for medical reasons (six controls). The control patients by definition showed neither dysplasia nor aneuploidy nor cancer during a surveillance period of 2 to 13 years. This was in contrast to the matched cases: Two cases showed aneuploidy before the finding of dysplasia, and four cases presented aneuploidy and dysplasia simultaneously. In one case, multiple high-grade and low-grade dysplasia as well as widespread aneuploidy was found during surveillance colonoscopies and the colectomy specimen showed a carcinoma. In another case of widespread aneuploidy and repeated findings of indefinite and low-grade dysplasia, the colectomy specimen confirmed indefinite dysplasia only.
Aneuploidy as a marker for development of dysplasia is highly specific
In 1999, Lindberg et al. published a surveillance study on 147 patients with long-standing UC followed for 13 years in intervals of 1 to 2 years [47]. Aneuploidy was found in 20 patients: Six patients had aneuploidy without dysplasia, and in three patients, aneuploidy and dysplasia were detected simultaneously. In four patients, aneuploidy preceded the finding of dysplasia, while in seven patients, dysplastic changes preceded the finding of aneuploidy. Additionally, there were 21 patients without aneuploidy but dysplasia. Eight of these patients were indefinite for dysplasia, seven had low-grade dysplasia, two had a dysplasia-associated lesion/mass (DALM), and four patients had a carcinoma. Three of these carcinomas were diploid, whereas one was aneuploid. Lindberg et al. calculated the sensitivity of aneuploidy to indicate the development of dysplasia (low-grade dysplasia or higher) to be 0.5 and the specificity to be 0.94. Thus, detection of aneuploidy during surveillance is associated with an increased risk to develop severe dysplasia.
A study on 368 UC patients by Holzmann et al. focused on the prevalence of aneuploidy dependent on the extent of UC and the correlation of aneuploidy with clinical characteristics [44]. Aneuploidy was found in 32 of the 368 patients, and its frequency increased with disease extent and duration. The frequency of aneuploidy increased from 2.9 % in biopsy specimens without dysplasia to 39.6 % in biopsy specimens classified as indefinite for dysplasia and 35.7 % in biopsy specimens classified as low-grade dysplasia up to 80 % in high-grade dysplasia. All carcinomas were aneuploid.
Moreover, Holzmann et al. conducted a surveillance study on 63 UC patients, which were preselected for aneuploidy (10 patients), dysplasia (8 patients), dysplasia and aneuploidy (6 patients) as well as extent and duration of UC (39 patients) [44]. Five out of the ten patients preselected for aneuploidy developed dysplasia and two a carcinoma during follow-up. Aneuploidy was widely distributed throughout the colon.
In a retrospective study on 24 patients, Habermann et al. focused on independent cellular markers including aneuploidy as a predictor for malignant transformation in UC [46]. Patients were divided into two groups: Group A comprised eight patients who underwent surgery for UCC, and group B comprised 16 patients without clinical or morphological signs of malignancy. In group A, aneuploidy was detectable on average 7.8 years before the UCC diagnosis throughout the entire colon and rectum unrelated to dysplasia. In one patient, there was no detection of dysplasia prior to cancer diagnosis. All eight UCCs were aneuploid. Remarkably, there was one UCC patient without any detection of dysplasia prior to cancer diagnosis. In contrast, DNA aneuploidy was found in only seven of 16 patients in group B. Among these seven patients, aneuploidy was found in two patients at the beginning of the observation period and could not be detected in subsequent biopsies. The remaining five patients were found to be aneuploid at the end of the observation period.
Sjoqvist et al. conducted a double-blind, controlled pilot trial in which the potential of the preventing or reverting effect of ursodeoxycholic acid (UDCA) on patients with long-standing colorectal inflammatory bowel disease with existing premalignant findings was analyzed [45]. Thirteen UC patients with extensive colitis and low-grade dysplasia and/or aneuploidy were included. Seven UC patients were included to the treatment group, while the remaining six received placebos. Six out of seven and four out of six patients in the treatment and placebo group, respectively, showed aneuploidy. Two of the UC patients in the treatment group underwent surgery before inclusion to the study because of DALM with high-grade dysplasia and a carcinoma, respectively. During the study, one UC patient of the placebo group developed dysplasia and underwent colectomy, but there was no carcinoma found in the colectomy specimen.
Choi et al. recently published a retrospective analysis on the correlation of ploidy and the outcome of UC and Crohn’s disease patients [53]. In a total of 29 UC patients who were diagnosed with a lesion indefinite for dysplasia, DNA ploidy was measured by flow cytometry and patients were followed up for 1 to 96 months. Aneuploidy or dysplasia was found in seven and two of those patients, respectively, and aneuploidy and dysplasia were found in one patient. None of the included UC patients developed an UCC during follow-up. However, in general, Choi et al. found a strong correlation between the finding of aneuploidy in patients who were initially classified as indefinite for dysplasia on histological examination and subsequent detection of neoplastic lesions [53].
Meta-analysis on prognostic impact of either aneuploidy, dysplasia, or aneuploidy plus dysplasia for UCC development
To evaluate the significance of aneuploidy, dysplasia, or a combination of aneuploidy and dysplasia as prognostic markers for the development of an UCC, the frequencies of UCCs, aneuploidy, and dysplasia of each study were summarized (Table 4) and meta-analyses of these data were conducted subsequently (Figs. 1, 2, and 3). The test for heterogeneity was not rejected for all three analyses. Neither funnel plots (data not shown) nor rank correlation tests revealed evidence for a potential publication bias. ORs were calculated for all studies for aneuploidy, dysplasia, and the combination of aneuploidy and dysplasia, with the exception of dysplasia in Rutegard et al. (1989) as there were no patients without dysplasia in the group of patients without detection of an UCC [50].
Almost all point estimations of the OR give evidence that there is a significantly higher chance to develop an UCC if aneuploidy or dysplasia or aneuploidy plus dysplasia has been detected. Based on all studies included, for aneuploidy, the overall OR is 5.3 [95 % CI 2.03, 13.93], for dysplasia 4.93 [1.61, 15.11], and for aneuploidy plus dysplasia 8.99 [3.08, 26.26].
Hence, aneuploidy is an equally effective parameter for UCC risk assessment as dysplasia. Strikingly, the combined assessment of dysplasia and aneuploidy is superior compared to applying each parameter alone. Interestingly, ploidy analysis by image cytometry compared to flow cytometry was a more accurate predictor.
Discussion
At present, dysplasia is used as a marker of impending malignant transformation in surveillance colonoscopy in UC. However, the efficacy of surveillance programs based on histopathologic evaluation of dysplasia has been questioned for several reasons, and additional reliable parameters of high prognostic impact in individual risk assessment for development of UCC are necessary.
Nuclear DNA assessment is considered to be a promising marker in risk assessment during surveillance. Measurement of aneuploidy in comparison to dysplasia is in fact more objective and less sensitive to assessment error, one of the major obstacles associated with dysplasia [29]. Overall, the mean age at first detection of aneuploidy was 40.2 ± 11.8 years, and the mean duration of the disease was 20.0 ± 8.6 years.
Dysplastic lesions were found considerably more frequently than aneuploidy, considering all studies on unselected UC patients (Table 2). However, numerous dysplastic lesions were reactive, inflammatory changes of the colonic mucosa, which were considered to be indefinite for dysplasia. Aneuploidy was absent in the majority of these cases [23, 47, 51, 52]. In the collective of Lofberg et al., five patients underwent surgery because of detection of dysplasia and aneuploidy [38]. Aneuploidy was more reproducible in the surgical specimens than dysplasia, and in one case, severe inflammatory changes made histopathologic evaluation impossible, but aneuploidy was detectable reliably. Thus, DNA assessment is a useful tool in discrimination of inflammatory changes and dysplasia.
In numerous cases, aneuploidy tended to be found more widespread in the course of the disease, but occasionally, aneuploidy was detected once but could not be found again in subsequent examinations [38, 46, 47, 49, 50]. In two patients, aneuploidy was intermittently undetectable [48, 52]. This observation raises the question whether changes in DNA content are reversible or aneuploidy has not been detected again due to sampling errors. Indeed, there are several studies indicating that aneuploidy is reversible in the bronchial mucosa in dogs [54, 55].
Aneuploidy as well as dysplasia was found to be patchy over the colon and rectum without any obvious spatial relation to each other, but aneuploidy tended to be found more widespread throughout the entire colon and rectum [38, 44, 46]. Rubin et al. calculated the number of biopsies needed for reliable detection of the highest category of aneuploidy or dysplasia with a confidence of 95 %. At least 56 biopsy specimens are needed for the detection of definite dysplasia, while 30 biopsy specimens are sufficient for detection of the respective grade of aneuploidy [23]. Although at least four biopsies per every 10 cm around the colon for assessment of dysplasia are recommended by international guidelines [24], there was little consent about the number of biopsies needed for nuclear DNA assessment (Table 1). In Rubin et al., samples were taken from four quadrants in intervals of 10 cm [23]. Samples were subdivided into two parts for histopathologic evaluation and ploidy measurement, respectively. We suggest this procedure of sampling to become part of the consensus criteria for clinical routine standard. There were several cases of aneuploidy without detection of dysplasia; thus, progression from aneuploidy to dysplasia could not be demonstrated consistently. However, this phenomenon might be attributable to a lag of long-term follow-up of patients. There is also evidence to suggest that malignant transformation arises before or without preceding detectable dysplasia [51].
Almost all included studies were based on nuclear DNA assessment by flow cytometry. However, we favor ploidy evaluation by means of image cytometry, since it allows the measurement of single nuclei in combination with (histo-/cyto-)morphological assessment. This enables the investigator to avoid inflammatory cells, to analyze small sample sizes, and to identify small aneuploid subpopulations. Image cytometry was found to be more sensitive for detection of aneuploidy in comparison to flow cytometry [56, 57]. Particularly, DNA assessment by flow cytometry on paraffin-embedded samples may be hampered by several measurement errors [58]. Besides methodological differences in assessment of DNA content, a number of different methods in terms of preparation of the biopsy specimens (fresh, frozen, paraffin embedded) used controls and the definition of aneuploidy was found in the included studies. Since preparation and storage of the biopsy specimens as well as the analysis and interpretation of aneuploidy assessment are crucial, common guidelines in DNA content analysis are essential for adequate evaluation of biopsies.
In conclusion, our meta-analysis revealed that aneuploidy is an equally effective parameter for UCC risk assessment as dysplasia. Strikingly, the combined assessment of dysplasia and aneuploidy is superior compared to applying each parameter alone. Thus, detection of dysplasia and/or aneuploidy will indicate high-risk patients affording timely follow-up. Conversely, patients with normal findings on DNA content and histopathologic evaluation can be examined less frequently. Thus, aneuploidy assessment should become part of consensus guidelines as complementing risk parameter.
References
Crohn UB, Rosenberg H (1925) The sigmoidoscopic picture of chronic ulcerative colitis (non-specific). Am J Med Sci 170:220–228
Campbell S, Ghosh S (2002) Ulcerative colitis and colon cancer: strategies for cancer prevention. Dig Dis 20(1):38–48 doi: ddi20038 [pii]
Eaden JA, Abrams KR, Mayberry JF (2001) The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut 48(4):526–535
Winther KV, Jess T, Langholz E, Munkholm P, Binder V (2004) Long-term risk of cancer in ulcerative colitis: a population-based cohort study from Copenhagen County. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association 2(12):1088–1095
Lutgens MW, van Oijen MG, van der Heijden GJ, Vleggaar FP, Siersema PD, Oldenburg B (2013) Declining risk of colorectal cancer in inflammatory bowel disease: an updated meta-analysis of population-based cohort studies. Inflamm Bowel Dis 19(4):789–799. doi:10.1097/MIB.0b013e31828029c0
Jess T, Simonsen J, Jorgensen KT, Pedersen BV, Nielsen NM, Frisch M (2012) Decreasing risk of colorectal cancer in patients with inflammatory bowel disease over 30 years. Gastroenterology 143(2):375–381 . doi:10.1053/j.gastro.2012.04.016e371; quiz e313-374
Herrinton LJ, Liu L, Levin TR, Allison JE, Lewis JD, Velayos F (2012) Incidence and mortality of colorectal adenocarcinoma in persons with inflammatory bowel disease from 1998 to 2010. Gastroenterology 143(2):382–389. doi:10.1053/j.gastro.2012.04.054
Riddell RH, Goldman H, Ransohoff DF, Appelman HD, Fenoglio CM, Haggitt RC, Ahren C, Correa P, Hamilton SR, Morson BC et al (1983) Dysplasia in inflammatory bowel disease: standardized classification with provisional clinical applications. Hum Pathol 14(11):931–968
Seril DN, Liao J, Yang GY, Yang CS (2003) Oxidative stress and ulcerative colitis-associated carcinogenesis: studies in humans and animal models. Carcinogenesis 24(3):353–362
Terzic J, Grivennikov S, Karin E, Karin M (2010) Inflammation and colon cancer. Gastroenterology 138(6):2101–2114 e 2105. doi: S0016-5085(10)00176-9 [pii] 053/j.gastro.2010.01.058
Stange EF, Travis SP (2008) The European consensus on ulcerative colitis: new horizons? Gut 57(8):1029–1031 doi: gut.2007.146761 [pii] 1136/gut.2007.146761
Itzkowitz SH, Present DH (2005) Consensus conference: colorectal cancer screening and surveillance in inflammatory bowel disease. Inflamm Bowel Dis 11(3):314–321 doi: 00054725-200503000-00012 [pii]
Carter MJ, Lobo AJ, Travis SP (2004) Guidelines for the management of inflammatory bowel disease in adults. Gut 53(Suppl 5):V1–16. doi:10.1136/gut.2004.043372 53/suppl_5/v1 [pii]
Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, Ganiats T, Levin T, Woolf S, Johnson D, Kirk L, Litin S, Simmang C (2003) Colorectal cancer screening and surveillance: clinical guidelines and rationale-update based on new evidence. Gastroenterology 124(2):544–560. doi:10.1053/gast.2003.50044 S0016508502158951 [pii]
Kornbluth A, Sachar DB (2004) Ulcerative colitis practice guidelines in adults (update): American College of Gastroenterology, practice parameters committee. Am J Gastroenterol 99(7):1371–1385. doi:10.1111/j.1572-0241.2004.40036.x AJG40036 [pii]
Rubin DT, Rothe JA, Hetzel JT, Cohen RD, Hanauer SB (2007) Are dysplasia and colorectal cancer endoscopically visible in patients with ulcerative colitis? Gastrointest Endosc 65(7):998–1004 doi: S0016-5107(06)02950-6 [pii] 1016/j.gie.2006.09.025
Lutgens MW, Vleggaar FP, Schipper ME, Stokkers PC, van der Woude CJ, Hommes DW, de Jong DJ, Dijkstra G, van Bodegraven AA, Oldenburg B, Samsom M (2008) High frequency of early colorectal cancer in inflammatory bowel disease. Gut 57(9):1246–1251 doi: gut.2007.143453 [pii] 1136/gut.2007.143453
Meyer R, Laubert T, Sommer M, Benecke C, Lehnert H, Fellermann K, Bruch HP, Keck T, Thorns C, Habermann JK, Buning J (2015) Colorectal neoplasia in IBD-a single-center analysis of patients undergoing proctocolectomy. Int J Color Dis 30(6):821–829. doi:10.1007/s00384-015-2217-7
Connell WR, Lennard-Jones JE, Williams CB, Talbot IC, Price AB, Wilkinson KH (1994) Factors affecting the outcome of endoscopic surveillance for cancer in ulcerative colitis. Gastroenterology 107(4):934–944 doi: S0016508594003082 [pii]
Lynch DA, Lobo AJ, Sobala GM, Dixon MF, Axon AT (1993) Failure of colonoscopic surveillance in ulcerative colitis. Gut 34(8):1075–1080
Riddell RH (1998) How reliable/valid is dysplasia in identifying at-risk patients with ulcerative colitis? J Gastrointest Surg 2(4):314–317 doi: S1091-255X(98)80068-1 [pii]
Dobbins WO 3rd (1977) Current status of the precancer lesion in ulcerative colitis. Gastroenterology 73(6):1431–1433
Rubin CE, Haggitt RC, Burmer GC, Brentnall TA, Stevens AC, Levine DS, Dean PJ, Kimmey M, Perera DR, Rabinovitch PS (1992) DNA aneuploidy in colonic biopsies predicts future development of dysplasia in ulcerative colitis. Gastroenterology 103(5):1611–1620
Collins PD, Mpofu C, Watson AJ, Rhodes JM (2006) Strategies for detecting colon cancer and/or dysplasia in patients with inflammatory bowel disease. Cochrane Database Syst Rev 2:CD000279. doi:10.1002/14651858.CD000279.pub3
Bernstein CN, Weinstein WM, Levine DS, Shanahan F (1995) Physicians’ perceptions of dysplasia and approaches to surveillance colonoscopy in ulcerative colitis. Am J Gastroenterol 90(12):2106–2114
Eaden JA, Ward BA, Mayberry JF (2000) How gastroenterologists screen for colonic cancer in ulcerative colitis: an analysis of performance. Gastrointest Endosc 51(2):123–128 doi: S0016510700310124 [pii]
Dixon MF, Brown LJ, Gilmour HM, Price AB, Smeeton NC, Talbot IC, Williams GT (1988) Observer variation in the assessment of dysplasia in ulcerative colitis. Histopathology 13(4):385–397
Odze RD, Tomaszewski JE, Furth EE, Feldman MD, Diallo R, Poremba C, Becker I, Hoefler H, Goldblum JR, Rybicki LA, Alsaigh N, Fogt F (2006) Variability in the diagnosis of dysplasia in ulcerative colitis by dynamic telepathology. Oncol Rep 16(5):1123–1129
Melville DM, Jass JR, Shepherd NA, Northover JM, Capellaro D, Richman PI, Lennard-Jones JE, Ritchie JK, Andersen SN (1988) Dysplasia and deoxyribonucleic acid aneuploidy in the assessment of precancerous changes in chronic ulcerative colitis. Observer variation and correlations. Gastroenterology 95(3):668–675 doi:S001650858800280X [pii]
Eaden J, Abrams K, McKay H, Denley H, Mayberry J (2001) Inter-observer variation between general and specialist gastrointestinal pathologists when grading dysplasia in ulcerative colitis. J Pathol 194(2):152–157. doi:10.1002/path.876 [pii] 1002/path.876
Dundas SA, Kay R, Beck S, Cotton DW, Coup AJ, Slater DN, Underwood JC (1987) Can histopathologists reliably assess dysplasia in chronic inflammatory bowel disease? J Clin Pathol 40(11):1282–1286
Melville DM, Jass JR, Morson BC, Pollock DJ, Richman PI, Shepherd NA, Ritchie JK, Love SB, Lennard-Jones JE (1989) Observer study of the grading of dysplasia in ulcerative colitis: comparison with clinical outcome. Hum Pathol 20(10):1008–1014. doi:10.1016/0046-8177(89)90273-6
Hammarberg C, Slezak P, Tribukait B (1984) Early detection of malignancy in ulcerative colitis. A flow-cytometric DNA study. Cancer 53(2):291–295
Burum-Auensen E, Deangelis PM, Schjolberg AR, Roislien J, Andersen SN, Clausen OP (2007) Spindle proteins aurora a and BUB1B, but not Mad2, are aberrantly expressed in dysplastic mucosa of patients with longstanding ulcerative colitis. J Clin Pathol 60(12):1403–1408 doi: jcp.2006.044305 [pii] 1136/jcp.2006.044305
Sjoqvist U, Hertervig E, Nilsson A, Duan RD, Ost A, Tribukait B, Lofberg R (2002) Chronic colitis is associated with a reduction of mucosal alkaline sphingomyelinase activity. Inflamm Bowel Dis 8(4):258–263
Keller R, Foerster EC, Kohler A, Floer B, Winde G, Terpe HJ, Domschke W (2001) Diagnostic value of DNA image cytometry in ulcerative colitis. Dig Dis Sci 46(4):870–878
Burmer GC, Rabinovitch PS, Haggitt RC, Crispin DA, Brentnall TA, Kolli VR, Stevens AC, Rubin CE (1992) Neoplastic progression in ulcerative colitis: histology, DNA content, and loss of a p53 allele. Gastroenterology 103(5):1602–1610 doi:S0016508592004360 [pii]
Lofberg R, Brostrom O, Karlen P, Ost A, Tribukait B (1992) DNA aneuploidy in ulcerative colitis: reproducibility, topographic distribution, and relation to dysplasia. Gastroenterology 102(4 Pt 1):1149–1154
Porschen R, Molsberger G, Reis C, Borchard F, Reis HE, Eckardt VF, Purrmann J, Hengels KJ, Strohmeyer G (1992) DNA ploidy and dysplasia in ulcerative colitis—interim analysis of a prospective study. Zeitschrift Fur Gastroenterologie 30(12):857–862
Levine DS, Rabinovitch PS, Haggitt RC, Blount PL, Dean PJ, Rubin CE, Reid BJ (1991) Distribution of aneuploid cell populations in ulcerative colitis with dysplasia or cancer. Gastroenterology 101(5):1198–1210 doi:S0016508591003712 [pii]
Meyer KF, Nause SL, Freitag-Wolf S, Kruger S, Bruch HP, Roblick UJ, Habermann JK (2013) Aneuploidy characterizes adjacent non-malignant mucosa of ulcerative colitis-associated but not sporadic colorectal carcinomas: a matched-pair analysis. Scand J Gastroenterol 48(6):679–687. doi:10.3109/00365521.2013.783103
Grabsch H, Kerr D, Quirke P (2004) Is there a case for routine clinical application of ploidy measurements in gastrointestinal tumours? Histopathology 45(4):312–334 doi: HIS1901 [pii] 1111/j.1365-2559.2004.01901.x
Fozard JB, Quirke P, Dixon MF, Giles GR, Bird CC (1986) DNA aneuploidy in ulcerative colitis. Gut 27(12):1414–1418
Holzmann K, Klump B, Borchard F, Gregor M, Porschen R (2001) Flow cytometric and histologic evaluation in a large cohort of patients with ulcerative colitis: correlation with clinical characteristics and impact on surveillance. Dis Colon rectum 44(10):1446–1455
Sjoqvist U, Tribukait B, Ost A, Einarsson C, Oxelmark L, Lofberg R (2004) Ursodeoxycholic acid treatment in IBD-patients with colorectal dysplasia and/or DNA-aneuploidy: a prospective, double-blind, randomized controlled pilot study. Anticancer Res 24(5B):3121–3127
Habermann J, Lenander C, Roblick UJ, Kruger S, Ludwig D, Alaiya A, Freitag S, Dumbgen L, Bruch HP, Stange E, Salo S, Tryggvason K, Auer G, Schimmelpenning H (2001) Ulcerative colitis and colorectal carcinoma: DNA-profile, laminin-5 gamma2 chain and cyclin a expression as early markers for risk assessment. Scand J Gastroenterol 36(7):751–758
Lindberg JO, Stenling RB, Rutegard JN (1999) DNA aneuploidy as a marker of premalignancy in surveillance of patients with ulcerative colitis. Br J Surg 86(7):947–950. doi:10.1046/j.1365-2168.1999.01133.x
Karlen P, Young E, Brostrom O, Lofberg R, Tribukait B, Ost K, Bodian C, Itzkowitz S (1998) Sialyl-Tn antigen as a marker of colon cancer risk in ulcerative colitis: relation to dysplasia and DNA aneuploidy. Gastroenterology 115(6):1395–1404 doi:S0016508598006015 [pii]
Befrits R, Hammarberg C, Rubio C, Jaramillo E, Tribukait B (1994) DNA aneuploidy and histologic dysplasia in long-standing ulcerative colitis. A 10-year follow-up study. Dis Colon rectum 37(4):313–319 discussion 319-320
Rutegard J, Ahsgren L, Stenling R, Roos G (1989) DNA content and mucosal dysplasia in ulcerative colitis. Flow cytometric analysis in patients with dysplastic or indefinite morphologic changes in the colorectal mucosa. Dis Colon rectum 32(12):1055–1059
Rutegard J, Ahsgren L, Stenling R, Roos G (1988) DNA content in ulcerative colitis. Flow cytometric analysis in a patient series from a defined area. Dis Colon rectum 31(9):710–715
Lofberg R, Tribukait B, Ost A, Brostrom O, Reichard H (1987) Flow cytometric DNA analysis in longstanding ulcerative colitis: a method of prediction of dysplasia and carcinoma development? Gut 28(9):1100–1106
Choi WT, Rabinovitch PS, Wang D, Westerhoff M (2015) Outcome of "indefinite for dysplasia" in inflammatory bowel disease: correlation with DNA flow cytometry and other risk factors of colorectal cancer. Hum Pathol 46(7):939–947. doi:10.1016/j.humpath.2015.03.009
Auer G, Ono J, Nasiell M, Caspersson T, Kato H, Konaka C, Hayata Y (1982) Reversibility of bronchial cell atypia. Cancer Res 42(10):4241–4247
Ono J, Auer G, Caspersson T, Nasiell M, Saito T, Konaka C, Kato H, Hayata Y (1984) Reversibility of 20-methylcholanthrene-induced bronchial cell atypia in dogs. Cancer 54(6):1030–1037
Lanigan D, McLean PA, Curran B, Leader M (1993) Comparison of flow and static image cytometry in the determination of ploidy. J Clin Pathol 46(2):135–139
Bauer TW, Tubbs RR, Edinger MG, Suit PF, Gephardt GN, Levin HS (1990) A prospective comparison of DNA quantitation by image and flow cytometry. Am J Clin Pathol 93(3):322–326
Willenbucher RF, Aust DE, Chang CG, Zelman SJ, Ferrell LD, Moore DH 2nd, Waldman FM (1999) Genomic instability is an early event during the progression pathway of ulcerative-colitis-related neoplasia. Am J Pathol 154(6):1825–1830 doi: 1016/S0002-9440(10)65438-7 S0002-9440(10)65438-7 [pii]
Acknowledgments
This study was conducted in connection to the North German Tumor Bank of Colorectal Cancer (ColoNet), generously supported by the German Cancer Aid Foundation (DKH e.V. #108446). Rüdiger Meyer is supported by a Mildred Scheel postdoctoral scholarship of the German Cancer Aid.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Meyer, R., Freitag-Wolf, S., Blindow, S. et al. Combining aneuploidy and dysplasia for colitis’ cancer risk assessment outperforms current surveillance efficiency: a meta-analysis. Int J Colorectal Dis 32, 171–182 (2017). https://doi.org/10.1007/s00384-016-2684-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-016-2684-5