Abstract
Introduction
Anastomotic leak (AL) is a significant cause of morbidity and mortality associated with complications of colorectal surgery. Furthermore, AL results in prolonged hospital stays and significant increase in costs of medical resources.
Materials and methods
In this study, we investigated the impact of anastomosis technique on the rate of anastomotic leak. The rate of leak was compared between two groups performing end-to-end (E-E) vs. side-to-end (S-E) anastomosis. The impact of various risk factors was also compared between the two groups.
Results
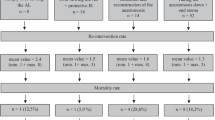
There were 382 E-E and 363 S-E anastomoses after left colectomy or rectal resections. The anastomotic leak rate was 8.64 % using E-E compared to 1.93 % using S-E anastomosis technique (p < 0.001).
Conclusions
These results indicate that the rate of anastomotic leak after left colon and rectum resections could be significantly reduced utilizing S-E anastomosis technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anastomotic leak (AL) is the most feared complication in colorectal surgery. An incidence rate as high as 16 % has been reported. Up to one third of all mortalities after colorectal surgery are associated with AL [1, 2, 5, 18, 30, 33]. Furthermore, AL results in significantly longer hospital stays. Due to high rate of mortality between 10 and 33 %, knowledge of the causes and prophylactic procedures to avoid peritonitis and subsequent lethal complications is of paramount importance [1, 5].
A bowel anastomosis represents a wound. Therefore, the healing mechanism is similar to other wounds. Many factors which can result in abnormal wound healing are known. These factors include immune disease, metabolic abnormalities (diabetes, obesity and malnutrition), mechanical factors such as tension on the anastomosis and others [2, 4, 7, 13, 20, 23, 27, 34].
The most important factor based on the literature review and our experience is however an abnormal blood supply in the area of the anastomosis [8, 20–22]. It is known that after dissection of the bowel for anastomosis, there could be macroscopic areas of poor blood supply at the resection margin of the bowel. It is generally accepted that performing an anastomosis utilizing these poorly vascularized bowel areas is associated with a high risk of anastomotic leak and that bowel anastomosis should always be performed using macroscopic bowel segments with adequate blood supply.
The question arises whether a macroscopic normal appearance of bowel wall precludes a decreased microscopic perfusion. In other words, whether a decreased microcirculation without visible discoloration of the resection margin could be a risk factor [1, 3, 9, 12, 16, 25, 29, 35].
The logical consequence of this hypothesis is to relocate the anastomosis from an area with poor blood supply, namely resection margin to an area away from the resection margin which is normally perfused. These anastomoses are called side-to-side (S-S) if they are performed on both sides and S-E if performed only on one side of the bowel. These types of anastomoses, which can also be performed using minimally invasive techniques [19, 26, 28], are not commonly performed, and their impact on the perfusion of the bowel wall and anastomotic leak has not been examined.
If this hypothesis is correct, the AL rate for an anastomosis which is performed in an area away from the resection margin (S-S or S-E) should be lower than an anastomosis which is performed at the resection margin of the bowel (E-E).
A Medline search found no study that has examined our hypothesis. There is only one study from Kracht et al. [24] which compared the AL rate after stapled and hand-sewn anastomoses for colon resection. Since the linear stapled anastomoses were technically conditioned, side-to-side, and the hand-sewn anastomoses were E-E, the comparison was indirectly between E-E and S-S anastomoses. The results demonstrated a leak rate of much higher for hand-sewn E-E anastomoses (8.3 %) compared to stapled S-S anastomoses (2.8 %) [24].
There are two studies comparing the rate of recurrence at the site of anastomosis in patients with Crohn’s disease comparing hand sewn E-E and stapled S-S anastomosis. The primary outcome in both studies was the rate of recurrence which was not statistically significant. As a secondary outcome in the study by McLeod et al. [29], no difference in the rate of anastomotic leak was noted. However, in the study by Zurbruchen et al. [39], the rate of AL in the E-E anastomosis was 6.5 % vs. none in the S-S anastomosis. The results of these studies therefore confirm our hypothesis.
The goal of this retrospective study was to examine the impact of anastomosis technique on the leak rate of colorectal anastomoses. The question was if the differences in bowel wall perfusion (resection margin vs. distant area) have a significant impact on the leak rate of the anastomoses.
Materials and methods
As preliminary anatomical studies at our institution, we have performed anatomical and physiological studies of the bowel wall and various anastomoses to study the normal anatomic blood circulation of the bowel wall and the microcirculation in the area of the resection using laser duplex sonography.
Following these studies, we have reviewed our clinical experience comparing E-E and S-E anastomosis techniques.
At the Helios hospital of Schleswig, E-E colorectal anastomoses were routinely performed until 2004. Since 2004, bowel anastomoses have been mainly performed using S-E (Figs. 1 and 2).
The S-E anastomoses after left colon, sigmoid, and rectum resection performed from 2007 to 2011 were compared to E-E anastomoses between 2000 and 2004.
Furthermore, we examined the impact of various risk factors for anastomotic leak including gender, indication, stoma, diabetes, steroid use, neoadjuvant therapy, emergency procedures, chronic inflammatory bowel diseases, surgeon, and technique (open vs. laparoscopic). All patients who had a left colon or rectal resection between 2000 and 2004 and between 2007 and 2011 were included.
An anastomotic leak was diagnosed if at least one of the following criteria was present:
-
1.
contrast leak in the area of anastomosis during CT exam or illumination using rectal contrast application
-
2.
visible stool leak out of drains
-
3.
proof of a leak using rectoscopy or colonoscopy
A major leak was defined as an anastomotic leak resulting in redo operation using either abdominal or rectal approach. An AL was defined as minor, when it was treated conservatively or using only interventional procedures [6, 10, 14, 37, 38].
Statistical analysis was performed using chi-square test to examine significant differences and one-way classification using Yates correction for comparison.
Results
The results of anatomical, physiological studies are demonstrated in Figs. 3, 4, 5, 6, 7, 8, 9, 10 and 11:
Close-up of Fig. 1, longitudinal collaterals connect the perpendicular small arteries which penetrate the bowel wall (vasa recta)
Figures 3, 4 and 5 demonstrate intramural microcirculation of colon (which was visualized by a special polymer staining technique). It is visible that the longitudinal collaterals connect the perpendicular small arteries, which penetrate the bowel wall (vasa recta). These arteries are severed during a bowel resection. The blood circulation after resection at the dissected edge is not from both sides (vasa recti) but from one side only. This could result in an area of decreased blood circulation compared to an area away from the anastomosis. We examined this hypothesis with a laser duplex sonography. This demonstrated an area of decreased blood circulation at the edge about 2 cm from the end of the colon (Fig. 6). Furthermore, the laser study showed that the blood circulation is best using S-S anastomosis followed by S-E anastomosis and worse using E-E technique (Figs. 7, 8 and 9).
Following these studies, it follows that anastomotic leak rate should be highest using E-E anastomosis and lowest using S-S anastomosis (Figs. 10 and 11).
There were 382 E-E and 363 S-E anastomoses. Thirty-three (8.64 %) of 382 patients with E-E anastomosis developed an AL. There were 19 (4.97 %) major and 14 (3.66 %) minor leaks. Of 363 patients with S-E anastomosis, 7 (1.93 %) suffered an AL. Five patients (1.38 %) had a major and two (0.55 %) had a minor leak.
All anastomosis were performed using a double stapling technique with a linear stapler for resection of the rectum and a circular stapler for completion of the anastomosis.
The mean operative time was 164 min in the S-E vs. 132 min in E-E anastomosis groups. The differences were not statistically significant. The longer operative time in the S-E group is due to the fact that more procedures were done laparoscopically.
In the S-E anastomosis group, there were no blood transfusions. In the E-E group, there were two patients who required blood transfusions. None had AL.
A comparison between E-E and S-E anastomoses demonstrates a statistically significant difference regarding anastomotic leak rate (p < 0.0001).
Of the total 40 anastomotic leaks, 9 were diagnosed with a CT scan. Twenty had contrast studies to confirm the diagnosis. Eight patients had stool or air in the abdominal drains. In four patients, the diagnosis was made using endoscopy.
Twenty-six (65 %) patients had elevated inflammatory parameters (leucocytes or C reactive protein). Twenty-eight (70 %) developed clinical symptoms (abdominal pain, peritonitis, fever, dyspnoea, vomiting, restlessness, etc.). Six (15 %) patients developed fever over 38.5 °C. Five patients (12.5 %) developed systemic inflammatory response syndrome (SIRS). Eleven patients (27.5 %) developed peritonitis, and one patient (2.5 %) died during hospital stay of respiratory failure due to SIRS.
The mortality rate of anastomotic leak in patients with E-E anastomoses was 3.03 % compared to none undergoing S-E anastomoses. This corresponds to an overall mortality rate of 2.5 %. Patients with an AL had a significantly longer hospital stay of 33 and 30 days after E-E and S-E anastomosis, respectively.
Aside from the distribution of neoadjuvant radiation, which because of an earlier therapy regimen in our hospital was significantly different in two groups, the distribution of other risk factors was statistically identical (Table 1).
The impact of other risk factors which were equally distributed between the two groups was examined and statistically compared with regard to the anastomotic leak rate (Table 2). However, no significant impact of these factors on anastomotic leak rate could be demonstrated. A statistically significant correlation between oncological indication and anastomotic leak could not be determined.
Neoadjuvant radiation therapy was administered in 30 patients in the E-E anastomosis group (a common approach at that time). There were no patients who underwent this treatment in the S-E group. Therefore, the distribution of patients with preoperative radiation was statistically significant comparing the two groups.
In the group of patients who underwent E-E anastomosis, no patients underwent minimally invasive procedure. In patients with S-E anastomosis, 45.73 % were performed minimally invasive, 50.14 % had open surgery and 3.86 % underwent conversion to open surgery. Of the seven patients with an AL, one was after laparoscopic technique, one after open conversion and five after open surgery. There was no correlation between surgical technique (open vs. laparoscopic) and the rate of anastomotic leak.
The number of surgeons was similar in both groups (five). Four surgeons were identical in both groups. One surgeon in the E-E anastomosis group had retired and was replaced with new surgeons. The difference between surgeons with regard to the rate of anastomotic leak in both groups was statistically not significant.
Discussion
Anastomotic leak (AL) is a major complication after colon resections. The incidence of this severe complication in literature is between 1.6 and 16 % . Anastomotic leak is associated with high morbidity and significant mortality rate. In the literature of the past 25 years, the reported mortality rate is up to 33 % [1, 3, 9, 12, 16, 25, 29, 35].
A bowel anastomosis represents a wound. Therefore, the healing mechanism is similar to any other wounds. Many factors which can result in abnormal wound healing are known. These factors include immune disease, metabolic abnormalities (diabetes, obesity and malnutrition), mechanical factors such as tension on the anastomosis and others [2, 4, 7, 13, 20, 23, 27, 34].
The most important factor based on the literature review and our experience is however an abnormal blood circulation in the area of the anastomosis [8, 20–22]. It is known that after dissection of the bowel for anastomosis, there are macroscopic areas of abnormal blood circulation at the resection margin of the bowel. There is general agreement that performing an anastomosis utilizing these poorly vascularized bowel segments is associated with higher risk of anastomotic leak and that bowel anastomosis should always be performed using macroscopic well vascularized bowel segments.
As the results of our anatomical and physiological studies demonstrate (Figs. 3, 4 and 5), the blood circulation after resection at the dissected edge is no longer provided from both sides (vasa recti) but from one side only. This could result in an area of decreased blood circulation compared to an area away from the anastomosis. We examined this hypothesis with a laser duplex sonography. This demonstrated an area of decreased blood circulation at the edge about 2 cm from the end of the colon (Fig. 6). Furthermore, the laser study showed that the blood circulation is best using S-S anastomosis followed by S-E anastomosis and worse using E-E technique (Figs. 7, 8 and 9). Following these studies, we conclude that anastomotic leak rate should be highest using E-E anastomosis and lowest using S-S anastomosis (Figs. 10 and 11).
These anatomical and physiological findings are in accordance with our clinical observation which demonstrated that by utilizing the technique of S-E anastomosis, the incidence of AL can be significantly reduced (from 8.64 to 1.93 %).
A literature review showed the following other risk factors: male gender, diabetes, chronic inflammatory bowel disease (Crohn and ulcerative colitis), emergency indications, corticosteroid usage, neoadjuvant chemotherapy or radiation, and finally a questionable association with the experience and technical capability of the surgeon. The significant difference in both groups could not be attributed to any in the literature-reported risk factors, since these factors were either similarly distributed in both groups or, if different, did not show any correlation with the rate of anastomotic leak [11, 15, 17, 31, 32].
There are two previously reported studies comparing the rate of disease recurrence at the site of anastomosis in patients with Crohn’s disease using E-E hand-sewn vs stapled S-E anastomosis. As a secondary end point, they compared the rate of anastomotic leak. In the study by McLeod et al., there was no difference in the rate of anastomotic leak that was noted. However, Zurbruchen et al. [39] demonstrated a higher rate of AL in the E-E anastomosis (6.5 %) compared to the S-S anastomosis (0 %).
The neoadjuvant radiation therapy of 30 patients after rectal resection between 2000 and 2004 was performed based on an established earlier therapy concept at our institution.
Theoretically, an impact of radiation on the healing of the bowel anastomosis is possible. It could also be hypothesized that the neoadjuvant radiation is associated with a higher rate of anastomotic leak in the E-E anastomosis group. A negative impact of radiation on wound healing has been reported in the literature [11, 17, 34]. Of the 30 radiated patients, 3 (10 %) developed anastomotic leak, while 30 of 352 (8.52 %) of not radiated patients developed anastomotic leak. The difference was statistically not significant. Also, considering all 715 patients who did not receive radiation in both groups, the rate of anastomotic leak was 5.12 % and not significantly different between radiated and not radiated patients.
In conclusion, our results indicate that the performance of S-E anastomosis after colorectal resection results in significantly lower rate of anastomotic leak compared to standard E-E anastomosis.
References
Abete M, Ronchetti V, Casano A, Pescio G (2003) Anastomotic leakage after traditional surgery of the colon and rectum. Minerva Chir 58:167–174
Alberts JC, Parvaiz A, Moran BJ (2003) Predicting risk and deminishing the consequences of anastomotic dehiscence following rectal resection. Colorectal Dis 5:478–482
Alves A, Panis Y, Trancart D, Regimbeau J-M, Pocard M, Valleur P (2002) Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patients. World J Surg 26:499–502
Bernstein EF, Salomon GD, Harisiadis L, Talbot T, Harrington F, Russo A, Uitto J (1993) Collagen gene expression and wound strength in normal and radiation-impaired wounds. A model of radiation-impaired wound healing. J Dermatol Surg Oncol 19(6):564–570
Bokey EL, Chapuis PH, Fung C, Hughes WJ, Koorey SG, Brewer D, Newland RC (1995) Postoperative morbidity and mortality following resection of the colon and rectum for cancer. Dis Colon Rectum 38(5):480–486
Braun A, Flohr C, Hopt UT (2012) Endoskopischer Vakuum-assistierter Verschluss (VAC) bei Anastomoseninsuffizienzen nach anteriorer Rektumresektion. Z Gastroenterol. doi:10.1055/s-0032-1308813
Burns JL, Mancoll JS, Phillips LG (2003) Impairments to wound healing. Clin Plast Surg 30(1):47–56
Carus T, Emmert A (2011) Die laparoskopische Fluoreszenzangiographie mit Indocyaningrün zur intraoperativen Beurteilung der Perfusion bei kolorektalen Anastomosen. Z Gastroenterol. doi:10.1055/s-0031-1285178
Choi H-K, Law W-L, Ho JWC (2006) Leakage after resection and intraperitoneal anastomosis for colorectal malignancy: analysis of risk factors. Dis Colon Rectum 49:1719–1725
Eckmann C, Kujath P, Schiedeck TH, Shekarriz H, Bruch HP (2004) Anastomotic leakage following low anterior resection: results of s standardized diagnostic and therapeutic approach. Int J Dis 19:128–133
El Malt M, Ceelen W, van den Broecke C, Cuvelier C, Van Belle S, De Neve W, de Hemptinne B, Pattyn P (2001) Healing of experimental colonic anastomoses: effects of combined preoperative high-dose radiotherapy and intraperinoneal 5- fluorouracil. Int J Cancer 96(5):297–304
Elton C, Makin G, Hitos K, Cohen CRG (2003) Mortality, morbidity and functional outcome after ileorectal anastomosis. Br J Surg 90:59–65
Fink M (2011) Welsch, Büchler Anastomoseninsuffizienz im Gastrointestinaltrakt, Intensivmedizin up2date 7
Frieling T, Lüthen R, Heintges T, Niederau C, Oette M, Vogt C, Vom Dahl S (2011) Endoskopische Therapie von Leckagen im Gastrointestinaltrakt, an den Gallenwegen und im Pankreas. Z Gastroenterol 49(6):740–748
Furst MB, Stromberg BV, Blatchford GJ, Christensen MA, Thorson AG (1994) Colonic anastomoses: bursting strength after corticosteroid treatment. Dis Colon Rectum 37(1):12–15
Golub R et al (1997) J Am Surg 184:364–372
Hendriks T, Wobbes T, de Man BM, Hoogenhout J, Seifert WF (1998) Moderate doses of intraoperative radiation severely suppress early strength of anastomoses in the rat colon. Radiat Res 150(4):431–435
Herrle, F. Schattenberg T, Post S, Kienle P (2012) Verhindert die Omentumplastik Anastomoseninsuffizienzen in der colorektalen Chirurgie?- Ein systematisches Cochrane Review. Z Gastoenterol doi:10.1055/s-0032-1324320
Ito M et al (2009) Einfluss der Lernkurve auf Kurzzeitresultate nach laparoskopischer Resektion wegen Rektumkarzinom. Coloproctology 31(6):345–351
Jähne J (2010) Intestinale Anastomosentechniken. Der Chirurg 82:5–6. doi:10.1007/s00104-010-1904-8
Jahnson S, Holtz A, Gerdin B (1998) Anastomotic blood-flow reduction in rat small intestine with chronic radiation damage. Digestion 59(2):134–141
Johansson K, Ahn H, Herder A, Lindhagen J (1988) Assessment of gastrointestinal bloodflow with laser doppler flowmetry in patients with chronic radiation injury. Acta Chir Scand 154(4):291–296
Kehler A (2011) Wie unterscheiden sich Patienten mit Anastomoseninsuffizienzen hinsichtlich der Operationsmethode (offen vs. Laparoskopisch)? Inauguraldissertation der Universität Regensburg. urn:nbn:de:bvb:355-epub-214338
Kracht M, Hay JM, Fagniez PL, Fingerhut A (1993) Ileocolonic anastomosis after right hemicolectomy for carcinoma: stapled or hand-sewn? Int J Colorectal Dis 8(1):29–33
Köckerling F, Rose J, Schneider C, Scheidbach H, Scheuerlein H, Reymond MA, Reck T, Konradt J, Bruch HP, Zornig C (1999) Laparoscopic colorectal anastomosis: risk of postoperative leakage; Results of a multicenter study. Surg Endosc 13:639–644
Lang RA, Hüttl TP, Winter H, Meyer G, Jauch KW (2005) How safe are laparoscopic intracorporal anastomoses? Zentralbl Chir 130(1):65–70
Law WI, Chu KW, Ho JWC, Chan CW (2000) Risk factors for anastomotic leakage after low anterior resection for rectal cancer with total mesorectal excision. Am J Surg 179:92–96
Mann B, Blase M, Kranz D, Soenmez M Y (2012) Robotik-assistierte laparoskopische kolorektale Resektionen mit dem Da Vinci System-Erfahrungsbericht der ersten 73 Fälle. Z Gastroenterol. doi: 10.1055/s-0032-1323920
McLeod RS, Wolff BG, Ross S, Parkes R, McKenzie M, Investigators of the CAST rial (2009) Recurrence of Crohn’s disease after ileocolic resection is not affected by anastomotic type: results of a multicenter, randomized, controlled trial. Dis Colon Rectum 52(5):919–27
Platell C, Barwood N, Dorfmann G, Makin G (2007) The incidence of anastomotic leaks in patients undergoing colorectal surgery. Colorectal Dis 9:71–79
Polat A, Nayci A, Polat G, Aksoyek S (2002) Dexamethasone down-regulates endothelial expression of intercellular adhesion molecule and impairs the healing of bowel anastomoses. Eur J Surg 168(8–9):500–506
Rodriguez-Ramirez SE, Uribe A, Ruiz-Garcia EB, Labastida S, Luna-Perez P (2006) Risk factors for anastomotic leakage after preoperative chemoradiation therapy and low anterior resection with total mesorectal excision for locally advanced rectal cancer. Rev Invest Clin 58(3):204–210
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer. Brit j surg 85:355–358
Seifert WF, Wobbes T, Hoogenhout J, de Man BM, Huyben KM, Hendriks T (1997) Intraoperative Sing, S., Cheng, T. The effect of systemic and local irradiation on wound macrophages and the repair promoting action of phenytoin sodium. Zhonghua Yi Xue Za Zhi 77(1):54–57
Sörensen LT, Jörgensen T, Kirkeby LT, Skovdal J, Vennits B, Wille-Jörgensen P (1999) Smoking and alcohol abuse are major risk factors for anastomotic leakage in colorectal surgery. Br J Surg 86:927–931
Takashi A et al (2011) Incidence of and risk factors for anastomotic leakage after laparoscopic anterior resection with intracorporeal rectal transection and double-stapling technique anastomosis for rectal cancer. Am J Surg 202(3):259–264
Wedemeyer J, Schneider AS, Winkler M, Manns MP (2011) Endoskopische Vakuumtherapie bei Perforationen und Anastomoseninsuffizienzen. Gastroenterologe 6(2):120–123
Weidenhagen R et al (2008) Endoluminale Vakuumtherapie im Management der Anastomoseninsuffizienz am oberen und unteren GI-Trakt. Endoskopie 21:30
Zurbuchen U, Kroesen AJ, Knebel P, Betzler MH, Becker H, Bruch HP, Senninger N, Post S, Buhr HJ, Ritz JP, German Advanced Surgical Treatment Study Group (2013) Complications after end-to-end vs. side-to-side anastomosis in ileocecal Crohn’s disease—early postoperative results from a randomized controlled multi-center trial Langenbecks. Arch Surg 398(3):467–74
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shekarriz, H., Eigenwald, J., Shekarriz, B. et al. Anastomotic leak in colorectal surgery: are 75 % preventable?. Int J Colorectal Dis 30, 1525–1531 (2015). https://doi.org/10.1007/s00384-015-2338-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2338-z