Abstract
Purpose
There is no clear consensus on how to assess low rectal anastomotic integrity and patency prior to reversal of de-functioning stoma. The aim of this systematic review was to assess the utility of contrast enema (CE) in this context and to clarify the natural history of radiological leaks.
Methods
Keyword search of electronic databases (Embase, MEDLINE, Cochrane Library, Google Scholar) and bibliographic cross-referencing were performed to identify appropriate studies. Data extraction and synthesis was performed with the primary outcomes being the sensitivity and specificity of CE for detecting clinically significant abnormalities. Statistical analysis was performed using Open Meta-Analyst software. Narrative review of outcomes including those of clinical and radiological leaks was also undertaken.
Results
A total of 1,142 CE from 11 articles were included in the final meta-analysis. CE had high specificity (95.4; 95 % confidence interval = 92.0–97.4) and negative predictive value (98.4; 97.4–99.1) and moderate sensitivity (79.9; 63.9–89.9) and positive predictive value (64.6; 55.5–72.9) for the detection of clinically significant anastomotic problems. There was a high degree of correlation between CE and clinical examination findings (96.7 %). Occult radiological leaks were seen in 5.7 % of CE, and all but one (97 %) eventually underwent successful reversal. Only three quarters of patients with clinical leak underwent successful reversal.
Conclusion
CE is effective at excluding clinically significant anastomotic problems, especially after clinical anastomotic leaks. However, false positive results can be observed in asymptomatic patients, and it is unclear how much additional information CE provides over clinical assessment in the low uncomplicated anastomosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anastomotic leak after restorative low rectal surgery carries serious short- and long-term sequalae [1]. Consequently, most surgeons chose to protect such anastomoses with a loop stoma. As a result, the true incidence of anastomotic dehiscence may be somewhat masked, and the incidence of this complication varies widely in the literature from 3 to 21 % [2]. Nevertheless, significant leaks do become clinically evident even in the presence of faecal diversion [3], and occult leaks may be detected after postoperative recovery by widespread use of contrast enemas. The natural history of these leaks is not widely qualified, and figures for subsequent restoration of intestinal continuity may vary from 20 to 60 % [4]. Consequently, there are no best practice guidelines for timing of stoma closure, assessment of anastomotic integrity and management of radiological leaks.
Mostly, low anastomoses are evaluated by digital rectal examination (DRE), flexible endoscopy or a contrast enema. Although clinical examination is an integral part of this evaluation, the practice of performing a routine contrast enema has been challenged more recently [5–7] and even omitted in some cases [7–9]. The aims of this systematic review were to assess the utility of performing contrast enema for anastomotic assessment after low rectal surgery and to examine the natural history of radiological leaks.
Methods
Search strategy
Two authors (KH, AG) performed systematic Medical Subject Heading (MeSH) search using Embase, MEDLINE, Cochrane Library and Google Scholar. Time frame for search was from the inception of databases till December 2013 following Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. Keywords used for search included ‘anterior resection’ OR ‘low anterior resection’ OR ‘proctectomy’ OR ‘proctocolectomy’, AND ‘ileostomy’, OR ‘de-functioning ileostomy’ OR ‘de-functioning stoma’ AND ‘contrast enema’ OR ‘contrast study’, OR ‘water soluble contrast study’ AND ‘anastomotic leak’ OR ‘complications’. Advanced search options including synonyms, partial word and combinations were used. Bibliographies of the retrieved articles were hand searched for further articles.
Inclusion criteria
Studies pertaining to use of contrast enemas to assess low bowel anastomosis with a covering loop stoma following low anterior resection, proctectomy or procto-colectomy were included. The types of anastomoses included were straight colo-anal, colo-rectal as well as colonic J pouches. Studies involving restorative procto-colectomy and ileal pouch anal anastomosis were included only if they were reported as subgroup of a larger colorectal anastomosis assessment study. Conflict of opinion was resolved by discussion and consensus (KH, AG, DW, FM, TW).
Endpoints
The primary endpoint for meta-analysis was evidence of any clinically significant abnormality as reflected by alteration of clinical management prior to reversal or evidence of significant abnormality after reversal. Secondary endpoints were clinically relevant leaks or strictures. Narrative analysis of methodological variation and minor outcomes was also performed.
Data extraction and synthesis
Data extraction was performed to identify true positive, true negative, false positive and false negative rates based on the above criteria. Sensitivity and specificity values of contrast enema were calculated for each study from the extracted data. Positive and negative predictive values were generated from the cumulative data. These parameters were used, as it is the accuracy of the positive or negative contrast enema result that is of interest to the clinician.
Statistical analysis
Data was analysed using Open Meta-Analyst, an open access, freely available software developed with funding from the National Centre for Research Resources, USA and Agency for Healthcare Research and Quality [10]. Analysis was performed using the random effects model based on DerSimonian-Laird method [11]. Cumulative analytic technique was used to assess the evolution of evidence over time. Forest plots were constructed for primary and secondary outcomes. Cumulative sensitivity and specificity were calculated and reported with 95 % confidence interval (CI). Heterogeneity in the studies was assessed and reported as I 2 statistic with P value. Heterogeneity was considered significant if the I 2 statistic exceeded 50 % and the P value was <0.05.
Results
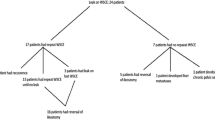
Six hundred and three articles were retrieved; out of which, 17 full-text articles were analysed after screening the abstracts. Ten articles fulfilled the inclusion criteria. Two articles were included from cross-referencing. A total of 12 studies were included in the review (Fig. 1). Out of these, ten studies were focused on role of contrast enema prior to ileostomy closure, whereas two studies also addressed the bowel function in these patients after ileostomy closure. Eleven studies were included in the final meta-analysis, and one study was excluded due to its case control design [12]. Details of these studies are given in Table 1.
Technique for contrast enema
One thousand one hundred sixty-nine contrast enema studies were performed in total. One case was excluded due to iatrogenic perforation. Technique of performing contrast enema was similar in most of the studies with minor variations. It involved passage of variable sized Foley catheter through the anal canal. The tip of which was placed just above the anastomosis. In majority of studies, the catheter balloon was not inflated to avoid false negative result from occlusion of anastomotic leak and to prevent potential disruption of the anastomotic site [8, 6]. Anastomosis was then distended using hydrostatic pressure of water-soluble contrast enema run from a container held at the height of 0.5 to 1 m [13]. Although Gastrografin and Urografin were the most commonly used contrast media, two studies mentioned using diluted barium [5, 14]. Only two papers mentioned the specific proximal height of contrast. In one study, the contrast was instilled till the proximal sigmoid [15] and in the other till the de-functioning ileostomy [6]. Although a control film was not routinely obtained, a post-evacuation view was taken in the majority of patients. Results were reported by gastrointestinal specialist radiologists and were deemed accurate.
Utility of contrast enema for all detecting all abnormalities
One thousand one hundred forty-two contrast enemas were performed in the 11 studies included in the final meta-analysis. Abnormalities (leak, stricture or fistula) were reported in 127 contrast enema studies (Table 1). Of these, 82 were considered true positive as clinically it was not deemed safe to reverse the stoma or because patients developed pelvic sepsis following attempted reversal. The sensitivity of contrast enema for all clinically significant abnormalities was 79.9 % (CI = 63.9–89.9 %) without significant heterogeneity (Fig. 2). The resulting positive predictive value was 64.6 % (CI = 55.5–72.7 %). Of the 1,015 studies that were reported as negative, significant problems that prevented reversal or were found after reversal were seen in 16, giving a specificity of 95.4 % (CI = 92.0–97.4 %) and negative predictive value of 98.4 % (CI = 97.4–99.1 %; Fig. 3).
This forest plot represents the cumulative sensitivity of contrast enema for detecting clinically significant abnormality. Size of the solid boxes represents weight of each individual study, and the bars represent 95 % confidence interval. The blue diamond at the bottom of the plot on the left represents cumulative sensitivity with the edges of the diamond representing 95 % confidence interval. Estimates and plot on the right represent contribution of individual studies to the cumulative sensitivity estimate. CI confidence interval, TP true positive, FN false negative
This forest plot represents the cumulative specificity of contrast enema for detecting clinically significant abnormality. Size of the solid boxes represents weight of each individual study, and the bars represent 95 % confidence interval. The blue diamond at the bottom of the plot on the left represents cumulative specificity with the edges of the diamond representing 95 % confidence interval. Estimates and plot on the right represent contribution of individual studies to the cumulative specificity estimate. CI confidence interval, TN true negative, FP false positive
Clinical and radiological leaks and their natural history
Overt clinical leak rates varied from 0 to 17 % across nine studies, with a combined leak rate of 5.6 % in 1,003 patients (Table 1). Outcomes were available for 44 of the 56 patients with clinical leaks (Table 2). The initial post-recovery contrast enema showed no leak in 24 (54.5 %). The remaining 20 patients were all managed with delayed reversal and serial contrast enemas. After serial screening, nine (20.5 %) of these patients were subsequently found to have a negative contrast enema. Of the 11 (25 %) with persistent leaks, reversal was attempted in two cases. One of these developed pelvic sepsis thereafter. All 33 patients with negative contrast enemas were reversed without any adverse events.
Covert radiological leak rates varied from 0.7 to 16 % across 11 studies, with a combined covert radiological leak rate of 5.7 % in 1,142 examinations (Table 1). Outcomes were available for 36 patients, though two of these did not undergo reversal for reasons other than anastomotic leak. In 16 (44.4 %), clinical assessment of the anastomosis was deemed sufficiently satisfactory to proceed with reversal despite radiological leak. Of the remaining 18 patients, 16 (44.4 %) were subsequently found to have negative contrast enemas after serial examinations and were reversed. Only two (5.6 %) had persistent leaks and one of these was reversed with a satisfactory outcome. All 32 patients with negative contrast enemas were reversed without any adverse events.
A further eight patients underwent reversal of their ileostomies after a persistent leak was demonstrated on serial contrast enemas. However, it was not possible to determine whether these patients had overt clinical leaks at the outset or subsequent covert radiological leaks because these data were aggregated. Nevertheless, all eight patients had no problems after reversal. Consequently, only 1 of 11 patients (9 %) suffered from pelvic sepsis after reversal of an ileostomy in the face of a persistent radiological abnormality.
Sensitivity and specificity of contrast enema to detect a leak were 77.5 % (CI = 59.2–89.0 %) and 96.6 % (CI = 93.7–98.2 %), respectively (Supplementary Figs. 5 and Fig. 6). Positive and negative predictive values for the ability of contrast enemas to detect true leaks (both persistence of an overt clinical leak or an occult radiological leak) were 61.7 % (CI = 51.1–71.4 %) and 98.8 % (CI = 97.9–99.4 %), respectively.
Anastomotic stricture
Across 11 studies, 36 strictures were detected radiologically (5.5 %), though the rate of detected strictures varied from 0 to 25 %. Of the 36 detected strictures, 8 (22 %) were deemed to be clinically irrelevant. In those with no strictures detected on contrast enema, three (0.3 %) were found to be significant strictures clinically. The sensitivity of contrast enemas for detection of strictures was 73.9 % (CI = 52.4–87.9 %), whilst specificity was 98.4 % (CI = 96.8–99.2 %) without any significant heterogeneity (Supplementary Figs. 7 and 8). Positive and negative predictive values for the ability of contrast enema to detect clinically significant strictures that required dilation were 77.8 % (CI = 60.4–89.3 %) and 99.7 % (CI = 99.1–99.9 %), respectively.
Fistula
Only two studies detected fistulae on contrast enema in six patients [16, 15]. The clinical examination failed to pick up these fistulae, although in retrospect some patients had consistent symptoms including perineal pain and discharge. However, the numbers were too small to perform any meaningful statistical analysis.
Bowel function in patients with leak on contrast enema
Two studies assessed bowel function after closure of ileostomy in patients with radiological leaks [3, 12]. Bowel function was significantly poorer in patients with radiological leak compared to those without leaks. The median time to closure of ileostomy was 11 months in those with radiological leaks compared to median time of 1.5 to 5.2 months in those without.
Clinical assessment of anastomosis versus contrast enema
Clinical assessment of anastomosis was compared to contrast enema in six studies [5–8, 17, 15]. Methods used for assessment varied and included digital rectal examination, proctoscopy, rigid sigmoidoscopy, flexible sigmoidoscopy and examination under anaesthetic. Across the 6 studies, 754 pairs of examinations were comparable (Table 3). Clinical assessment and contrast enema were in agreement in 731 (96.7 %) comparisons.
Safety of contrast enema
Of 1,169 contrast enemas examined across the 12 studies, there was one reported incidence of an iatrogenic perforation from barium enema [5]. No other enema-associated morbidity was reported.
Discussion
It has long been known that rates of permanent stoma between different centres are highly variable [18, 19]. Increasing patient expectations, technological developments and the advancing front of colorectal surgery is driving surgeons to consider performing low rectal and anal anastomoses for a much wider patient group. Since the consequences of an unprotected leak in the low pelvis can be so devastating, it follows that increasing numbers of diverting stoma are being fashioned [4, 19]. Despite this trend, there is no clear guidance as to when and how to assess anastomotic integrity and patency and to how best manage the patient with an established leak. This study examines the use of contrast enema to assess the patency and integrity of low rectal and anal anastomoses. This investigation has a high negative predictive value (98.4 %), suggesting that reversal after a negative result is exceptionally unlikely to result in anastomotic problems. However, the less favourable positive predictive value (64.6 %) suggests that a reasonable proportion of patients with a positive result could be safely reversed.
Despite reasonable positive and negative predictive values, there is a paucity of data to answer the question as to whether contrast enema gives any additional useful information over clinical examination alone. The majority of patients in this study had low anastomoses, palpable with digital rectal examination. Comparisons of clinical examination and contrast enema show a high degree of correlation between the two tests, although contrast enema appears to miss a large number of anastomotic strictures in comparison to digital rectal examination. Consequently, we would usually recommend that all patients with a low rectal anastomosis have manual palpation of this prior to reversal. For anastomoses beyond the reach of the examining finger, direct examination is more problematic and contrast enema would be advisable [20].
It is clear from this study, and from the wider literature, that performing contrast enema early after surgery results in a higher rate of radiological leaks [13]. Two studies that assessed anastomoses at a median of 4 weeks or less both had radiological leak rates in the region of 15 % [15, 21], compared to a rate of 1 to 6 % for those whose studies were performed typically after 6 weeks [16, 17, 8, 6, 5, 20]. This suggests that assessment of anastomoses with contrast enema should be 6 to 8 weeks after surgery to minimise radiological leaks whilst avoiding unnecessary delay in stoma reversal.
Two schools of thought existed with regard to the management of radiological leaks in those patients who had not previously demonstrated any clinical evidence of a leak. Some centres proceeded to reverse these patients if concurrent clinical examination confirmed an intact anastomosis [17, 6, 16, 15]. No problems were seen after reversal in 16 such cases. Other centres took a more cautious approach, reversing the stoma only after the leaks had resolved on serial enemas [3, 21, 12]. It is likely that a reasonable proportion will have no clinical evidence of a leak and could be safely reversed. Comparison of contrast enema with clinical examination in the study by Tang et al. might suggest that at least a third of patients with a radiological leak might be in this situation (18). In view of this, the positive predictive value for contrast enema is likely to be slightly lower than that estimated by this study. It is clear from our data, however, that vast majority of radiological leaks will resolve and become suitable for reversal.
Those patients with clinical leaks appear to have a very different postoperative course from those with radiological leaks. Although around half of patients will have no evidence of leak at their first contrast enema and undergo uneventful reversal, less than a half of those with an initial leak will eventually settle and come to reversal. As with radiological leaks, no problems were encountered after reversal following a negative contrast enema, suggesting that this investigation is valuable in assessing whether patients who have previously had leaks can be safely reversed.
It is less clear whether patients with a persistent radiological leak can be safely reversed. Only 11 patients were identified who underwent such a reversal. A problem with pelvic sepsis was only encountered in one of these patients after reversal. The patient in question had an identified clinical leak prior to the initial contrast enema. Due to aggregated data, it is not possible to determine how many of other 11 patients also had clinical leaks at the outset. However, data suggest that the risk of sepsis after reversal in such patients is at least 10 %.
Two papers examined the influence of the morphological appearance of the leak as seen on contrast study on its subsequent resolution, but there was little consistency in their findings. Lim et al. found that anatomical characteristics of the track seen on X-rays were of no clinical importance, but the presence of a cavity or stricture at anastomotic site was associated with non-healing [3]. Palmisano et al. suggested that track characteristics were significant, and a short linear track and non-dependent cavity with natural drainage were favourable factors for healing of anastomotic leak [21].
The chief limitation of this review is that the included studies are heterogeneous and mostly of weak evidence. Heterogeneity observed can be attributed to a large number of variables including study designs, variable endpoints, underlying pathology, indications for diversion, operative approach, anastomotic level, provision of adjuvant treatment and variations in performing contrast enema.
Conclusion
Contrast enema is useful to predict when patients with clinical leaks may be safely reversed. Its use in asymptomatic patients is less certain, as a reasonable proportion of patients will have false positive results and can undergo safe reversal. Contrast enema should be deferred until 6 to 8 weeks after surgery. Clinical examination should be used in addition to contrast enema for anastomoses within reach of the finger to further minimise false negative results. Figure 4 summarises the recommendations of this review.
References
Karanjia ND, Corder AP, Bearn P, Heald RJ (1994) Leakage from stapled low anastomosis after total mesorectal excision for carcinoma of the rectum. Br J Surg 81(8):1224–1226, http://www.ncbi.nlm.nih.gov/pubmed/7953369
Phillips BR, Harris LJ, Maxwell PJ, Isenberg GA, Goldstein SD (2010) Anastomotic leak rate after low anterior resection for rectal cancer after chemoradiation therapy. Am Surg 76(8):869–871, http://www.ncbi.nlm.nih.gov/pubmed/20726419
Lim M, Akhtar S, Sasapu K, Harris K, Burke D, Sagar P, Finan P (2006) Clinical and subclinical leaks after low colorectal anastomosis: a clinical and radiologic study. Dis Colon Rectum 49(10):1611–1619. doi:10.1007/s10350-006-0663-6
Makela JT, Kiviniemi H, Laitinen S (2003) Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum 46(5):653–660. doi:10.1097/01.DCR.0000059328.10563.8C
Hong SY, Kim do Y, Oh SY, Suh KW (2012) Routine barium enema prior to closure of defunctioning ileostomy is not necessary. J Korean Surg Soc 83(2):88–91. doi:10.4174/jkss.2012.83.2.88
Kalady MF, Mantyh CR, Petrofski J, Ludwig KA (2008) Routine contrast imaging of low pelvic anastomosis prior to closure of defunctioning ileostomy: is it necessary? J Gastrointest Surg Off J Soc Surg Aliment Tract 12(7):1227–1231. doi:10.1007/s11605-008-0510-2
Karsten BJ, King JB, Kumar RR (2009) Role of water-soluble enema before takedown of diverting ileostomy for low pelvic anastomosis. Am Surg 75(10):941–944, http://www.ncbi.nlm.nih.gov/pubmed/19886140
Khair G, Alhamarneh O, Avery J, Cast J, Gunn J, Monson JR, Hartley J (2007) Routine use of gastrograffin enema prior to the reversal of a loop ileostomy. Dig Surg 24(5):338–341. doi:10.1159/000107713
Cowan T, Hill AG (2005) Ileostomy closure without contrast study is safe in selected patients. ANZ J Surg 75(4):218–219. doi:10.1111/j.1445-2197.2005.03369.x
Wallace BC, Schmid CH, Lau J, Trikalinos TA (2009) Meta-analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol 9:80. doi:10.1186/1471-2288-9-80
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188, http://www.ncbi.nlm.nih.gov/pubmed/3802833
Killeen S, Souroullas P, Ho Tin H, Hunter IA, O’Grady H, Gunn J, Hartley JE (2013) Outcomes of asymptomatic anastomotic leaks found on routine postoperative water-soluble enema following anterior resection for cancer. World J Surg 37(11):2700–2704. doi:10.1007/s00268-013-2193-4
Shorthouse AJ, Bartram CI, Eyers AA, Thomson JP (1982) The water soluble contrast enema after rectal anastomosis. Br J Surg 69(12):714–717, http://www.ncbi.nlm.nih.gov/pubmed/7171972
Lee MR, Lee MJ, Kim JH, Hwang Y (2006) Is barium enema prior to ileostomy closure necessary? J Korean Soc Coloproctology 22:298–300
Tang CL, Seow-Choen F (2005) Digital rectal examination compares favourably with conventional water-soluble contrast enema in the assessment of anastomotic healing after low rectal excision: a cohort study. Int J Color Dis 20(3):262–266. doi:10.1007/s00384-004-0652-y
da Silva GM, Wexner SD, Gurland B, Gervaz P, Moon SD, Efron J, Nogueras JJ, Weiss EG, Vernava AM, Zmora O (2004) Is routine pouchogram prior to ileostomy closure in colonic J-pouch really necessary? Colorectal disease. Off J Assoc Coloproctology Great Brit Irel 6(2):117–120, http://www.ncbi.nlm.nih.gov/pubmed/15008910
MacLeod I, Watson AJ, Hampton J, Hussey JK, O’Kelly TJ (2004) Colonic pouchography is not routinely required prior to stoma closure. Color Dis Off J Assoc Coloproctology Great Brit Irel 6(3):162–164. doi:10.1111/j.1463-1318.2004.00626.x
Morris E, Quirke P, Thomas JD, Fairley L, Cottier B, Forman D (2008) Unacceptable variation in abdominoperineal excision rates for rectal cancer: time to intervene? Gut 57(12):1690–1697. doi:10.1136/gut.2007.137877
Codd RJ, Evans MD, Davies M, Harris DA, Chandrasekaran TV, Khot UP, Morgan AR, Beynon J (2014) Permanent stoma rates: a misleading marker of quality in rectal cancer surgery. Colorectal disease : Off J Assoc Coloproctology Great Brit Irel 16(4):276–280. doi:10.1111/codi.12509
Nabi H, Morgan M, Ooi K, Turner C, Kozman D (2013) The routine use of contrast enemas performed prior to the reversal of loop ileostomies does affect management. World J Colorectal Surg 3(4)
Palmisano S, Piccinni G, Casagranda B, Balani A, de Manzini N (2011) The reversal of a protective stoma is feasible before the complete healing of a colorectal anastomotic leak. Am Surg 77(12):1619–1623, http://www.ncbi.nlm.nih.gov/pubmed/22273219
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 5
This forest plot represents the cumulative sensitivity of contrast enema for detecting clinically significant anastomotic leak. Size of the solid boxes represents weight of each individual study and the bars represent 95 % confidence interval. The blue diamond at the bottom of the plot on the left represents cumulative sensitivity with the edges of the diamond representing 95 % confidence interval. Estimates and plot on the right represents contribution of individual studies to the cumulative sensitivity estimate. CI—Confidence interval, TP—True positive, FN—False negative. (GIF 3 kb)
Supplementary Fig. 6
This forest plot represents the cumulative specificity of contrast enema for detecting clinically significant anastomotic leak. Size of the solid boxes represents weight of each individual study and the bars represent 95 % confidence interval. The blue diamond at the bottom of the plot on the left represents cumulative specificity with the edges of the diamond representing 95 % confidence interval. Estimates and plot on the right represents contribution of individual studies to the cumulative specificity estimate. CI—Confidence interval, TN—True negative, FP—False positive. (GIF 3 kb)
Supplementary Fig. 7
This forest plot represents the cumulative sensitivity of contrast enema for detecting clinically significant anastomotic stricture. Size of the solid boxes represents weight of each individual study and the bars represent 95 % confidence interval. The blue diamond at the bottom of the plot on the left represents cumulative sensitivity with the edges of the diamond representing 95 % confidence interval. Estimates and plot on the right represents contribution of individual studies to the cumulative sensitivity estimate. CI—Confidence interval, TP—True positive, FN—False negative. (GIF 3 kb)
Supplementary Fig. 8
This forest plot represents the cumulative specificity of contrast enema for detecting clinically significant anastomotic stricture. Size of the solid boxes represents weight of each individual study and the bars represent 95 % confidence interval. The blue diamond at the bottom of the plot on the left represents cumulative specificity with the edges of the diamond representing 95 % confidence interval. Estimates and plot on the right represents contribution of individual studies to the cumulative specificity estimate. CI—Confidence interval, TN—True negative, FP—False positive. (GIF 3 kb)
Rights and permissions
About this article
Cite this article
Habib, K., Gupta, A., White, D. et al. Utility of contrast enema to assess anastomotic integrity and the natural history of radiological leaks after low rectal surgery: systematic review and meta-analysis. Int J Colorectal Dis 30, 1007–1014 (2015). https://doi.org/10.1007/s00384-015-2225-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2225-7