Abstract
Background
High-grade internal rectal prolapse appears to be one of the contributing factors in the multifactorial origin of faecal incontinence. Whether it affects the outcome of sacral neuromodulation is unknown. We compared the functional results of sacral neuromodulation for faecal incontinence in patients with and without a high-grade internal rectal prolapse.
Method
One hundred six consecutive patients suffering from faecal incontinence, who were eligible for sacral neuromodulation between 2009 and 2012, were identified from a prospective database. All patients underwent preoperative defaecating proctography, anorectal manometry and ultrasound. Symptoms were assessed preoperatively and at 12 months after operation using a standardized questionnaire incorporating the Faecal Incontinence Severity Index (FISI range = 0–61) and the Gastrointestinal Quality of Life Index (GIQLI). Success was defined as a decrease in the FISI score of 50 % or more.
Results
High-grade internal rectal prolapse (HIRP) was found in 36 patients (34 %). The patient characteristics were similar in both groups. Temporary test stimulation was successful in 60 patients without HIRP (86 %) and in 25 patients with HIRP (69 %) (p = 0.03). A permanent pulse generator was then implanted on these patients. After 1-year follow-up, the median FISI was reduced in patients without HIRP from 37 to 23 (p < 0.01). No significant change in FISI score was observed in patients with a HIRP (FISI, 38 to 34; p = 0.16). Quality of life (GIQLI) was only improved in patients without HIRP. A successful outcome per protocol was achieved in 31 patients without HIRP (52 %) versus 4 patients with HIRP (16 %) (p < 0.01).
Conclusion
The presence of a high-grade internal rectal prolapse has a detrimental effect on sacral neuromodulation for faecal incontinence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
First described in 1995 by Matzel and co-workers, sacral neuromodulation (SNS) has evolved to an attractive method for the treatment of patients with faecal incontinence [1]. SNS offers significant improvement in patient symptoms on long-term follow-up [2]. Initially, it was thought that sacral neuromodulation was only effective in patients with an intact external anal sphincter [3]. However, it has recently been reported that sacral neuromodulation can also be used in patients with an external anal sphincter defect [4, 5].
Both the anal sphincters and the pelvic floor are thought to play an important role in maintaining faecal continence. It has been reported that pelvic floor injury is related to pelvic organ prolapse [6]. High-grade internal rectal prolapse appears to be one of the contributing factors in the multifactorial origin of faecal incontinence. It is possible that a high-grade (intra-anal) prolapse may cause stretching of the internal anal sphincter: previous studies have demonstrated that there is graduated worsening of anal resting pressures with higher grades of prolapse [7]. It is also considered that as the prolapse abuts the internal sphincter, it may lead to inappropriate firing of the recto-anal inhibitory reflex resulting in urge faecal incontinence [8]. Furthermore, incomplete rectal emptying due to the internal rectal prolapse might cause post-defaecatory leakage.
It is not known what influence the presence of a high-grade internal rectal prolapse has on the outcomes of sacral neuromodulation. The aim of this study was to compare the functional outcome and quality of life after sacral neuromodulation for faecal incontinence in patients with and without a high-grade internal rectal prolapse.
Methods
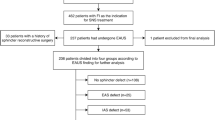
A consecutive series of 106 patients suffering from faecal incontinence, who underwent temporary sacral neuromodulation between August 2009 and August 2012, were identified from a prospectively maintained Pelvic Floor Registry (Filemaker Pro, Filemaker Pro Inc, Santa Clara, CA). In our institute, at that time, a trial sacral neuromodalation under local anaesthesia was the first step in the treatment of idiopathic faecal incontinence after unsuccessful maximum medical treatment, including 6 months of pelvic floor retraining or biofeedback. We described our technique of temporary sacral neuromodulation earlier in detail [9].
Before the procedure, patients underwent standardized defaecating proctography, ultrasound and anorectal manometry as previously described [10]. Proctograms were performed and reported by a radiologist with an interest in pelvic floor imaging. Prolapse grade was recorded using the Oxford Rectal Prolapse Grading system (Table 1) [11]. A comparison was performed on patients with high-grade internal rectal prolapse (grade 3–4) and the other of patients without high-grade internal rectal prolapse. Patients with an external rectal prolapse (grade 5) were excluded. The decision to perform an SNS test was taken independently but not necessarily blinded to the results of the proctogram.
All patients completed a bowel diary before, during and after test stimulation. All patients underwent test stimulation for at least 2 weeks, but in most cases, for 3 weeks. If patients encountered a reduction of incontinence episodes of at least 50 % during the test stimulation, the test period was considered as successful. Only patients with successful test stimulation were selected for permanent implantation.
For symptom evaluation, all patients completed a standardized questionnaire before and 1-year after implantation of a permanent pulse generator. The questionnaire incorporated the Faecal Incontinence Severity Index (FISI range 0–61), Wexner constipation score (range 0–30) [12] and Gastrointestinal Quality of Life Index (GIQLI range 0–144) [13, 14].
A comparison was performed of patients with and without a high-grade internal rectal prolapse. Ethical board approval was sought prior to the commencement of the study. Patients gave written consent before both the test and permanent procedures.
Statistical analysis was performed using the Statistical Package for Social Sciences, version 18.0 (SPSS Inc., Chicago, IL, USA). All data were treated as nonparametric and analysed using the Mann-Whitney U test (continuous data) or Fisher’s exact test (categorical data). Wilcoxon’s signed-rank test was used to compare the FISI scores and quality of life before and 1-year after sacral neuromodulation. Comparison of these changes between patients with and without high-grade internal rectal prolapse was conducted using the Mann-Whitney U test. To analyse predictive factors of the clinical outcomes after permanent sacral neuromodulation, patients were divided into two groups according to improvement in FISI score. Success was defined as a decrease in the score of 50 % or more and failure as a decrease of less than 50 %. This cut-off level was chosen arbitrarily; however, a reduction of incontinence episodes of 50 % is widely accepted as a successful outcome after sacral neuromodulation. A multivariate logistic regression analysis of the significant clinical variables in univariate analysis was done with logistic regression models with success and failure as the outcome. The variables used were those with a p value ≤0.1 in univariate analysis. The results are reported as odds ratio and 95 % confidence intervals (CI). p < 0.05 (two-tailed) was considered the limit of significance.
Results
A total of 106 patients underwent a trial sacral neuromodulation between August 2009 and August 2012 after failed maximal medical therapy. A high-grade prolapse (HIRP) was found in 36 patients (34 %). The patient characteristics were similar in both groups (Table 2), except for the preoperative prevalence of post-defaecatory leakage, concomitant rectocele and concomitant enterocele. Previous, non-prolapse-related operations performed included hysterectomy (n = 35) and overlapping sphincteroplasty (n = 14). There was no difference in previous (surgical) treatment between both groups. Temporary test stimulation was successful in 60 patients without HIRP (86 %) and in 25 patients with HIRP (69 %) (p = 0.03).
All patients with successful test stimulation underwent implantation of a pulse generator. In one patient without HIRP, the pacemaker was removed within 1 year because of pain at the side of the pacemaker and towards the leg. The FISI, Wexner constipation score and QOL scores of the remaining 84 patients with and without a high-grade internal rectal prolapse are shown in Table 3. The baseline FISI score (p = 0.32), Wexner constipation score (p = 0.28) and GIQOL (p = 0.18) were similar in both groups. After 1-year follow-up, the median FISI was reduced in patients without HIRP from 37 to 23 (p < 0.01). No significant change in FISI score was observed in patients with a HIRP (FISI, 38 to 34; p = 0.16). When comparing the change from baseline in FISI score in patients with and without a high-grade internal rectal prolapse, a significant difference (p < 0.01) was observed with median changes, respectively 5 and 16. The Wexner constipation score improved significantly in patients without a high-grade internal rectal prolapse compared with no significant change in patients with a high-grade internal rectal prolapse. The postoperative Wexner constipation was not significantly different between the two groups (p = 0.14). Quality of life (GIQOL) was only improved in patients without HIRP (p < 0.01) (Table 3). When comparing the change from baseline between both groups, a statistically significant difference was observed (p = 0.04).
Predictors for successful outcome after sacral neuromodulation (defined as a reduction of FISI score of at least 50 %) were analysed using univariable logistic regression. A successful outcome per protocol was achieved in 31 patients without HIRP (52 %) versus 4 patients with HIRP (16 %) (p < 0.01). On ‘intention to treat’, the success rates were 44 % in patients without HIRP and 11% in patients with HIRP (p < 0.01). There was no significant difference between patients with or without successful outcome for age, gender and anorectal manometry findings (Table 4). Patients with a poor outcome had significant more preoperative post-defaecatory incontinence, concomitant rectocele or enterocele. Multivariate analysis revealed that only a preoperative HIRP was an independent predictive factor of the success or failure after sacral neuromodulation (Table 5). Patients without a HIRP had a 5.3 fold greater chance of improving their faecal incontinence 12 months after sacral neuromodulation than patients with HIRP (CI 1.42–22.13; p < 0.01).
Discussion
The management of faecal incontinence seems to be extremely difficult as faecal incontinence has multifactorial etiologies including obstetric trauma, congenital, neuropathic and iatrogenic causes. High-grade internal rectal prolapse is believed to be one of the contributing causes of faecal incontinence although its exact mechanism remains unclear [7]. Sacral neuromodulation has proven to be effective for faecal incontinence treatment in several studies, showing significant improvement in patients’ symptoms and quality of life [2, 3]. One advantage of SNS over other surgical therapies is the ability to evaluate the treatment outcomes before the permanent implantation of the neurostimulator device. Therefore, suitable patient selection is mandatory to achieve satisfactory outcomes. In accordance with a review published by Jarret and co-workers, it showed PNE success rate ranges between 27 and 100 % in several studies [15]. Hence, predictive factors for the clinical outcomes of sacral nerve stimulation in the treatment of faecal incontinence are needed to be identified to avoid unnecessary future surgeries and to justify the cost effectiveness of SNS therapy.
There have been several published literatures on the predictive factors of SNS outcomes for the treatment of faecal incontinence. None of the baseline variables predicted the SNS outcome such as demographic data, number of incontinence, duration of incontinence, type of incontinence, preoperative endoanal ultrasound, endorectal physiology test and the aetiologies of faecal incontinence [16–20]. Only identified predictors of the PNE outcome were the placement of lead (position of the lead tip and repeated PNE) [18–20] and sensory response threshold [17, 18]. After the permanent SNS implantation, 15–30 % of the patients with faecal incontinence fail to respond for unknown reasons [17, 20]. Loose stool consistency and low stimulation threshold for sensory response appeared to be good prognostic factors for permanent implantation [16]. However, most of these studies have not mentioned about internal rectal prolapse, and external rectal prolapse was also excluded in some studies. Maeda and co-workers reported a lower success rate in aetiologies related to a rectal capacity problem but none of these causes was a statistically significant predictor of SNS outcome [18].
The rectal capacity to maintain faecal continence occurs by retro-peristaltic contraction in the rectum, propelling stools for storage in the sigmoid, descending and transverse colon [21]. These retrograde motor patterns act as a ‘brake’, and their absence or diminished frequency may allow colonic content to move more rapidly into the rectum, resulting in faecal incontinence if weakened pelvic floor muscles are present. Recently, Patton and co-workers demonstrated in patients with faecal incontinence that sacral neuromodulation causes increase in these retrograde motor patterns in the distal colon [22]. The question arises whether this mechanism of action of sacral neuromodulation is blocked by the presence of a high-grade internal rectal prolapse. Therefore, it might be worthwhile to correct rectal abnormalities first, before proceeding to sacral neuromodulation rather than performing sacral nerve neuromodulation as the first line of treatment in this group of patients.
Despite the unclear exact mechanisms of internal rectal prolapse causing faecal incontinence, this study has demonstrated that patients without high-grade internal rectal prolapse have higher success rate (85 %) of test stimulation than patients with high-grade internal rectal prolapse (69 %). Furthermore, there was a significant reduction in the median FISI (from 37 to 23) and significant improvement of quality of life in the first group of patients after 1 year follow-up. A successful outcome per protocol was achieved in 52 % of patients without HIRP versus 16 % of patients with HIRP (p < 0.01). These results seems to be lower than the previous published results [2, 3]; however, the main reason is that we defined success as a decrease in FISI score of 50 % or more, instead of the definition of 50 % or more improvement over baseline in faecal incontinence episodes per week, as used in most other SNS publications. The multivariate analysis has shown that preoperative high-grade internal rectal prolapse is an independent predictive factor for the success or failure of SNS implantation.
Therefore, this data suggests several new and important concepts. Firstly, high-grade internal rectal prolapse is one of the predictors for SNS treatment failure. In accordance to our study, this is the only published literature which significantly proved that internal rectal prolapse is a predictive factor for SNS outcome. Secondly, for faecal incontinence patients who underwent SNS and treatment appear to have loss efficacy, high-grade internal rectal prolapse should be (re)assessed when other mechanical issues (such as lead fracture, lead migration) have been ruled out. Thirdly, proctography or MR defecography should be a standard work up for faecal incontinence, although MR defecography tends to underestimate the grade of internal rectal prolapse [23]. Therefore, a decision to perform SNS should be made prior to SNS test stimulation. Otherwise resources may be wasted on a failed implantation after a successful SNS test in patients with internal rectal prolapse. Lastly, correction of the prolapse, e.g. by laparoscopic ventral rectopexy (LVR), resection rectopexy or the STARR procedure might be considered as the treatment method for faecal incontinence patients with high-grade internal rectal prolapse before offering SNS.
Nevertheless, this study has possible limitations. Firstly, there was a lack of data with reference to anorectal manometry and pelvic floor imaging following sacral neuromodulation. Secondly, sacral nerve stimulation may not have been effective in patients with a high-grade internal rectal prolapse because the faecal incontinence was mainly caused by poor rectal emptying. However, surprisingly, the Wexner constipation score was similar in patients with or without a rectal prolapse prior to the procedure. Furthermore, multivariate analysis showed that preoperative post-defaecatory incontinence was not an independent predictive factor.
Many studies have reported the improvement in faecal incontinence following LVR. Our recent data revealed that in a total of 72 patients who had high-grade internal rectal prolapse and underwent LVR, 21 patients (29 %) were completely continent 1 year after surgery and 40 patients (56 %) had significant improvement in continence [24]. The functional bowel problems remain in a substantial number of patients despite restoration of the external rectal prolapse. In 2005, Jarrett and co-workers [25] described sacral neuromodulation in four patients who had persistent faecal incontinence for more than a year after surgery for external rectal prolapse. This study showed marked improvement in faecal incontinence episodes in three of the four patients. Yap and co-authors (2010) [26] performed sacral neuromodulation in 11 patients with persistent or newly diagnosed faecal incontinence following repair of external rectal prolapse. Nine of eleven patients (82 %) had a successful sacral neuromodulation trial, and all patients with a permanent stimulator had a reduction of incontinence score of more than 50 %.
Consequently, the question arises whether patients with faecal incontinence associated with a high-grade internal rectal prolapse should initially be treated by an LVR with possible neuromodulation added later if the desired effect is not achieved. In analogy of the studies concerning sacral neuromodulation after surgery for external rectal prolapse, it might be worthwhile to perform sacral neuromodulation in patients with persistent bowel disturbances after restoration of the internal rectal prolapse.
In conclusion, we have demonstrated that a high-grade internal rectal prolapse has a negative effect on the outcome of SNS for the treatment of faecal incontinence.
References
Matzel KE, Stadelmaier U, Hohenfellner M, Gall FP (1995) Electrical stimulation of sacral spinal nerves for treatment of faecal incontinence. Lancet 346:1124–1127
Maeda Y, Lundby L, Buntzen S, Laurberg S (2013) Outcome of sacral nerve stimulation for fecal incontinence at 5 years. Ann Surg
Matzel KE, Kamm MA, Stosser M et al (2004) Sacral spinal nerve stimulation for faecal incontinence: multicentre study. Lancet 363:1270–1276
Chan MK, Tjandra JJ (2008) Sacral nerve stimulation for fecal incontinence: external anal sphincter defect vs. intact anal sphincter. Dis Colon Rectum 51:1015–1025
Melenhorst J, Koch SM, Uludag O, van Gemert WG, Baeten CG (2008) Is a morphologically intact anal sphincter necessary for success with sacral nerve modulation in patients with faecal incontinence? Colorectal Dis 10:257–262
DeLancey JO, Morgan DM, Fenner DE et al (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109:295–302
Harmston C, Cunningham C, Lindsey I (2011) The relationship between intenal rectal prolapse and internal anal sphincter function. Colorectal Dis 13:791–795
Farouk R, Duthie GS, Bartolo DC, MacGregor AB (1992) Restoration of continence following rectopexy for rectal prolapsed and recovery of the internal anal sphincter electromyogram. Br J Surg 79:439–440
Prapasrivorakul S, Gorissen, KJ, Gosselink MP, Curran K, Jones OM, Cunningham C, Lindsey I, Hompes R Temporary sacral neuromodulation under local anaesthesia using new anatomical reference points. Tech Coloproctology. Accepted 2014
Gosselink MP, Adusumilli S, Harmston C, Wijffels NA, Jones OM, Cunningham C, Lindsey I (2013) Impact of slow transit constipation on the outcome of laparoscopic ventral rectopexy for obstructed defaecation associated with high grade internal rectal prolapse. Colorectal Dis 15(12):e749–e756
Lindsey I Internal rectal prolapse. In: Lindsey I, Nugent K, Dixon T. (eds) Pelvic floor disorders for the colorectal surgeon (pp 93). Oxford, Oxford University Press
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD (1996) A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 39(6):681–685
Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC (1999) Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum 42:1525–1532
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmülling C, Neugebauer E, Troidl H (1995) Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg 82:216–222
Jarret ME, Mowatt G, Glazener CM et al (2004) Systematic review of sacral nerve stimulation for faecal incontinence and constipation. Br J Surg 91:1559–1569
Gallas S, Michot F, Faucheron FJ, Leroi AM Predictive factors for successful sacral nerve stimulation in the treatment of faecal incontinence: results of trial stimulation in 200 patients. Color Dis 13:689–696
Dudding TC, Parés D, Vaizey CJ, Kamm MA Predictive factors for successful sacral nerve stimulation in the treatment of faecal incontinence: a 10-year cohort analysis. Color Dis 10:249–256
Maeda Y, Norton C, Lundby L, Buntzen S, Laurberg S (2010) Predictors of the outcome of percutaneous nerve evaluation for faecal incontinence. Br J Surg 97:1096–1102
Gourcerol G, Gallas S, Michot F, Denis P, Leroi AM (2006) Sacral nerve stimulation in fecal incontinence: are there factors associated with success? Dis Colon Rectum 50:3–12
Govaert B, Melenhorst J, Nieman FH, Bols, van Gemert WG, Baeten CG (2009) Factors associated with percutaneous nerve evaluation and permanent sacral nerve modulation outcome in patients with fecal incontinence. Dis Colon Rectum 52:1688–1694
Rao SS, Welcher K (1996) Periodic rectal motor activity: the intrinsic colonic gatekeeper? Am J Gastroenterol 91:890–897
Patton V, Wiklendt L, Arkwright JW, Lubowski DZ, Dinning PG (2013) The effect of sacral nerve stimulation on distal colonic motility in patients with faecal incontinence. Br J Surg 100(7):959–968
Pilkington SA, Nugent KP, Brenner J, Harris S, Clarke A, Lamparelli M, Thomas C, Tarver D (2012) Barium proctography vs magnetic resonance proctography for pelvic floor disorders: a comparative study. Colorectal Dis 14(10):1224–1230
Gosselink MP, Adusumilli S, Gorissen K, Fourie S, Tuynman JB, Jones OM, Cunningham C, Lindsey I (2013) Laparoscopic Ventral Rectopexy for faecal incontinence associated with high grade internal rectal prolapse. Dis Colon Rectum 56:1409–1414
Jarrett ME, Matzel KE, Stösser M, Baeten CG, Kamm MA (2005) Sacral nerve stimulation for fecal incontinence following surgery for rectal prolapse repair: a multicenter study. Dis Colon Rectum 48:1243–1248
Yap JR, Zufferey G, Rosen H, Lechner M, Wunderlich M, Roche B (2010) Sacral nerve modulation in the treatment of fecal incontinence following repair of rectal prolapse. Dis Colon Rectum 53:428–431
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Read at the Tripartite Colorectal Conference, Birmingham, United Kingdom, from 30 June to 3 July 2014.
Rights and permissions
About this article
Cite this article
Prapasrivorakul, S., Gosselink, M., Gorissen, K.J. et al. Sacral neuromodulation for faecal incontinence: is the outcome compromised in patients with high-grade internal rectal prolapse?. Int J Colorectal Dis 30, 229–234 (2015). https://doi.org/10.1007/s00384-014-2078-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-2078-5