Abstract
Purpose
Hartmann’s procedure for rectal cancer patients is increasingly performed but few studies have reported the postoperative outcome. The purpose was to report postoperative complications and analyse risk factors in rectal cancer patients operated with Hartmann’s procedure. To describe the selection and postoperative complication patterns, all bowel-resected rectal cancer patients were included.
Methods
Population-based data were from the county of Västmanland, Sweden. All rectal cancer patients operated with an elective bowel resection between 1996 and 2012 were included. Demographics and postoperative complications were prospectively registered and data retrospectively analysed.
Results
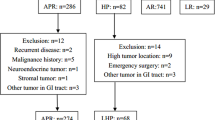
Of the 624 patients included, 396 (64 %) were operated with an anterior resection, 159 (25 %) with an abdominoperineal excision and 69 (11 %) a Hartmann’s procedure of which 90 % were low Hartmann’s. Patients operated with a Hartmann’s procedure were significantly older, had higher ASA-score, poorer WHO performance score and lower serum albumin levels. Operative time for Hartmann’s procedure was a median of 49 and 99 min shorter than after anterior resection and abdominoperineal excision, respectively, and entailed less bleeding. Complications related to the pelvic and perineal dissections were more common after abdominoperineal excision compared with anterior resection and Hartmann’s procedure (32 vs. 9 and 13 %, p < 0.001).
Conclusions
Few rectal cancer patients, operated with Hartmann’s procedure, developed pelvic complications despite a higher age, more co-morbidities, metastases in different localities and functional inferiority when compared with the patients operated with anterior resection or abdominoperineal excision. Hartmann’s procedure is a valid alternative procedure in the old and frail rectal cancer patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An increasing number of rectal cancer patients are being operated with Hartmann’s procedure (HP). Approximately 12 % of rectal cancer patients undergoing an abdominal operation in Sweden in 2003 were operated with HP [1]. Between 1996 and 2006, 30 % of rectal cancer patients with disseminated disease were also operated with this procedure [2]. A HP might be justified in patients with severe co-morbidities or impaired sphincter function in order to avoid the risk of anastomotic complications and poor function. The literature on morbidity after a HP is, however, scarce and inconclusive, even more so for patients operated with a low Hartmann’s procedure (LHP). During recent years, there have been some reports about high frequencies of pelvic abscesses, re-operations and re-admissions [3–5]. Abdominoperineal excisions (APE) have in some centres been performed to reduce the risk for pelvic abscesses after LHP. The outcome after HP has been compared with those after both anterior resection (AR) and abdominoperineal excision (APE) but previous studies have mostly been small, retrospective and not population-based and do not, therefore, allow one to make any clear conclusions about which procedure is best suited for a frail patient.
The aim of this population-based study was to describe the postoperative pelvic complications in rectal cancer patients operated with HP by analysing data and potential risk factors from a prospective database. In order to describe the selection of the procedure and the frequency of pelvic complications after HP, a comparison was also made with the alternative bowel resections AR and APE even though the groups were not directly comparable because of different pelvic complication patterns.
Methods
Since 1996, a comprehensive data base was set up at the Colorectal Unit, Västmanland’s Hospital, Västerås, with a catchment area of 260,000. All patients diagnosed with rectal cancer in the county of Västmanland were managed at the colorectal unit. Data were prospectively collected regarding demographics, radiology, surgery, histology, clinical course and oncology on all rectal cancer patients operated with a bowel resection [6]. Between 1996 and 2012, 624 patients underwent an elective bowel resection and were included in the study.
Definitions
Postoperative complications and death were defined as those that occurred within 30 days of the primary operation. To be able to compare the complications that could occur in the pelvis and perineum after the various resection methods, another variable was introduced, namely, a pelvic-perineal complication. It was defined as follows: anastomotic leakage after AR (including colovaginal fistula, infected hematoma and pelvic abscess), pelvic hematoma, abdominal or pelvic abscess, perineal wound infection (after APE) and urinary catheter at discharge. Postoperative surgical complications that were listed as “others” included prolonged small-bowel obstruction, stoma complications (necrosis, peristomal infections, stenosis and stoma retractions), pancreatitis, bile leakage, abdominal wound infections and deep wound dehiscence. To ensure that all postoperative complications were included in patients that had undergone a HP, we also performed a review of the medical records and the complications were also classified according to the Clavien-Dindo score of postoperative complications [7]. Low Hartmann’s procedure (LHP) was defined as transection of the rectum just above or at the pelvic floor.
Surgery
All patients were discussed at a multidisciplinary meeting regarding preoperative oncological treatment. During the study period, there was a clear intention to restrict the number of rectal cancer surgeons to no more than three surgeons experienced in total mesorectal excision (TME), and one of the surgeons (KS) either performed or supervised the procedures in 94 % of all cases. The aim was to deliver a specimen with complete and undamaged mesorectal fascia and if necessary to perform multi-organ en bloc resections of invaded adjacent organs as previously described [8].
The decision to perform a HP was made preoperatively in all cases. The primary indication was patients with severe co-morbidities, and/or poor functional status, malnutrition and/or presence of metastases where a HP was considered as a procedure with less severe postoperative complications compared with APE and AR. Another indication was impaired sphincter function in order to avoid the risk of anastomotic complications and poor function.
In HP, the TME was performed as for patients with an AR and in the majority the anorectum was divided at the level of the levator ani muscle. In all cases operated with HP and AR, the ano-rectum distal to the tumour was rinsed with at least 500 ml of an alcoholic solution before transection. All patients had open surgery.
Statistical analysis
Data were analysed using the Statistical Package for Social Sciences (SPSS™), version 19. Differences in proportions were calculated using the chi-square test or the t test for independent samples. Fisher’s exact test was used for low numbers. A binary multivariate logistic regression analysis of risk factors for the pelvic-perineal complications was performed including age, sex, ASA-score, WHO performance score, cardiovascular disease, preoperative albumin level, tumour tethering, preoperative radiotherapy, type of operation and en bloc resections. A p value of <0.05 was considered statistically significant.
Results
Of the 624 patients included, 396 (64 %) had undergone an AR, 159 (25 %) an APE and 69 (11 %) a HP. Of the 396 patients operated with an anterior resection, 290 (73 %) had a defunctioning loop-ileostomy. Patients that were operated with a HP were significantly older, had a higher ASA score, a poorer WHO performance score and lower serum albumin levels; see Table 1. There were no differences in the inflammatory response (C-reactive protein and white blood cell count), body mass index or frequency of smokers between the groups (data not shown).
The surgical details are listed in Table 2. In all groups, the surgery was performed with the intent of local radicality, but the rate of metastases was higher for HP (25 %) when compared with APE (14 %) and LAR (8 %). HP was performed as a LHP in 90 % of cases. Operative time for HP lasted for a median of 49 min less than for AR and 99 min less than for APE. There was also less operative bleeding.
Overall complications are listed in Table 3. Urinary catheter at discharge was a relatively common surgical complication in all groups. In total, 34 complications occurred in the 69 patients that were operated with HP. Majority of the complications were minor and could be managed pharmacologically. There were three patients with Clavien-Dindo 3b (two abdominal wound infections and one stoma complication).
Complications related to the pelvic-perineal dissection are presented in Table 4. These complications were more common in patients operated with APE than those operated with AR and HP (32 vs. 9 and 13 %, p < 0.001), mostly due to the high frequency of perineal wound infections (23 %). In patients that were operated with HP, two (3 %) developed a pelvic hematoma (Clavien-Dindo 3a), two (3 %) a pelvic abscess (Clavien-Dindo 3a) and five (7 %) were discharged with a urinary catheter in situ (Clavien-Dindo 2). Two patients operated with HP died within 30 days after surgery, one on the eighth postoperative day without any signs of postoperative surgical complications, no autopsy was performed and it was presumed that a cardiovascular event was the cause of death. The other died of heart failure after having been discharged.
The median postoperative stay in hospital was 12 days for patients who had undergone an HP and 13 days after an APE. The postoperative hospitalization was longer for both of these interventions, compared with 9 days after an AR (p < 0.001).
At the 1-year follow-up, there were no patients found with late symptomatic abscess or fistula after HP. However, no routine endoscopic assessment of anorektum was performed.
In the multivariate logistic regression analysis, the only factor associated with less pelvic-perineal complications was operation with a HP and AR (Table 5). In several APEs, en bloc resections of adjacent organs were performed but this did not seem to influence the rate of perineal complications.
Discussion
In this population-based study of rectal cancer patients operated with a predominantly low HP, the frequency of pelvic complications was low, even though patients who were operated with HP were older and had more co-morbidities, a higher ASA score and poorer WHO performance score than patients who underwent an AR or APE. The HPs were also more frequently performed in patients with metastases. Operative times were shorter, the amount of bleeding was less and most complications were minor and managed without the need of laparotomy in patients operated with HP. These results indicate that HP is a safe and valid alternative procedure in the old and frail rectal cancer patient.
All patients were followed up prospectively but routine postoperative endoscopy or radiology to detect pelvic complications were not performed in the non-symptomatic patient during the study period. This may have led to some suture line deficiencies or small abscesses being missed. To minimise the risk of poor registration of complications in the specifically studied group of HP, all medical records of patients operated with HP were retrieved and studied thoroughly.
Few studies on the postoperative complications after HP have been published and they are all small and retrospective. Majority have indicated a high frequency of pelvic complications compared with either APE or AR. Frye et al. described a 17.2 % pelvic abscess rate in 29 patients undergoing HP operations [3]. Rodriquez et al. reported a 12.2 % abscess rate in 41 patients undergoing a low HP, a re-operation rate of 15 % and a high re-admission rate, indicating that APE was a valid alternative to HP [4]. Töttrup et al. reported an overall pelvic sepsis frequency of 18.6 % after HP procedures. In patients who had undergone a low transection of the rectum, the pelvic abscess rate was 33 % compared with 8 % if the upper rectum was transected [5]. In the present study, which included 62 patients operated with a low HP, only two patients developed a pelvic abscess; one was managed by percutaneous drainage and the other with rectal lavage. Reasons for the high rate of pelvic complications in previous studies might be selection of even more unfit patients than in the present study, although our demographic data indicate a very old, co-morbid and functionally inferior cohort. The surgical technique, especially the transection of the rectum at the pelvic floor is probably also of importance. We have used the broadest possible transverse stapler that fits into the pelvis in order to avoid tension in the stapler line (mostly 45 and 60 mm), and we have also routinely used two pelvic drains that were removed 2 days postoperatively. Pelvic complications after both HP and AR are more common in males [4, 5]. In the present study, which demonstrates a low number of complications, half of the patients were males.
In the study by Frye et al., there was no difference in operative time between HP and APE [3], but in the present study, the operative time for a HP was significantly shorter than that for AR and APE. The number of abdominal wound infections in the present study was low in all groups, probably due to lack of registration of minor wound infections.
The literature on postoperative outcomes after HP is astonishingly scarce despite the fact that this method is being increasingly used in the old and frail and no clear conclusions can be drawn from these few reports. Despite our favorable results, there seems to be a problem with high rates of pelvic complications after HP in the surgical community. Another problem could be disabling secretion and bleeding from the ano-rectal stump. We have not been able to find any reports of this in non-inflammatoric bowel disease (IBD) patients.
A limitation of the present study was that the surgical groups (AR, HP, APE) were not directly comparable due to differences in the complexity of the surgical procedures and their complication patterns. Still, a comparison between patients operated with major abdominal operation in this population-based setting, is necessary to be able to draw conclusions on the frequency and severity of pelvic complications after HP. Despite the heterogeneity between the groups, it is important to compare them and, furthermore, to attempt to define the type of patients selected for HP. It would appear that HP is a valid alternative in the old and frail patients characterized by co-morbidities, malnutrition and metastasic spread. In this audit, the pelvic complication rate was as low as that observed after AR, despite the obvious selection of much younger, healthier and functionally more fit patients.
One can speculate as to what an anastomotic leak would entail for the HP group, if they were to undergo an AR.
An APE with intersphincteric dissection has been proposed as an alternative to HP in order to minimise the surgical complications, especially the high rate of pelvic sepsis and also the high rate of perineal infections observed after APE. A much smaller perineal wound and better healing when the ano-pelvic muscles are left in place and the exclusion of a rectal suture line should mean a reduced risk of perineal wound infection and pelvic abscess. However, this technique has only been reported in patients with IBD, and not in patients with rectal cancer [9]. To determine the optimal operative technique for rectal cancer patients not suitable for anastomosis, we have set up a multi-centre randomized controlled study comparing the surgical complications after HP and intersphincteric APE (HAPirect, NCT01995396).
In conclusion, our data show in contrast to most other studies a low pelvic complication rate after HP. A low Hartmann procedure should not be abandoned for selected patients that are very old and frail, co-morbid and functionally inferior. The role of an intersphincteric APE as a better alternative than HP will hopefully be clarified in the upcoming HAPirect trial.
References
Pahlman L, Bohe M, Cedermark B, Dahlberg M, Lindmark G, Sjodahl R, Ojerskog B, Damber L, Johansson R (2007) The Swedish rectal cancer registry. Br J Surg 94(10):1285–1292
Hosseinali Khani M, Pahlman L, Smedh K (2012) Treatment strategies for patients with stage IV rectal cancer: a report from the Swedish Rectal Cancer Registry. Eur J Cancer 48(11):1616–1623
Frye JN, Carne PW, Robertson GM, Frizelle FA (2004) Abdominoperineal resection or low Hartmann’s procedure. ANZ J Surg 74(7):537–540
Molina Rodriguez JL, Flor-Lorente B, Frasson M, Garcia-Botello S, Esclapez P, Espi A, Garcia-Granero E (2011) Low rectal cancer: abdominoperineal resection or low Hartmann resection? A postoperative outcome analysis. Dis Colon Rectum 54(8):958–962
Tottrup A, Frost L (2005) Pelvic sepsis after extended Hartmann’s procedure. Dis Colon Rectum 48(2):251–255
Smedh K, Olsson L, Johansson H, Aberg C, Andersson M (2001) Reduction of postoperative morbidity and mortality in patients with rectal cancer following the introduction of a colorectal unit. Br J Surg 88(2):273–277
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Smedh K, Khani MH, Kraaz W, Raab Y, Strand E (2006) Abdominoperineal excision with partial anterior en bloc resection in multimodal management of low rectal cancer: a strategy to reduce local recurrence. Dis Colon Rectum 49(6):833–840
Sher ME, Bauer JJ, Gorphine S, Gelernt I (1992) Low Hartmann’s procedure for severe anorectal Crohn’s disease. Dis Colon Rectum 35(10):975–980
Acknowledgments
The authors wish to thank Professor Kent Nilsson, Centre for Clinical Research, Uppsala University, for the statistical support.
Compliance with ethical standards funding
The study was supported by a research grant from the county of Västmanland, Sweden.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the local ethics committee of Uppsala University, Sweden (Dnr 2013/467) and followed the Declaration of Helsinki guidelines.
Informed consent
All patients in the study have given their informed consent prior to their inclusion in the study as they are all registered in the Swedish Rectal Cancer Registry (SRCR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sverrisson, I., Nikberg, M., Chabok, A. et al. Hartmann’s procedure in rectal cancer: a population-based study of postoperative complications. Int J Colorectal Dis 30, 181–186 (2015). https://doi.org/10.1007/s00384-014-2069-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-2069-6