Abstract
Purpose
To assess the quality of life and disease-specific functioning of adults with anorectal malformations (ARM) or Hirschsprung disease (HD) compared to healthy reference scores.
Methods
Patients with the diagnosis of ARM or HD from the Adult Colorectal Research Registry completed the Short Form 36 Health Survey (SF-36), the Gastrointestinal Quality of Life Index (GIQoLI), and the Bowel Function Score (BFS) between October 2019 and August 2022. One-sample Wilcoxon test compared the results to reported healthy references with a significance level of < 0.05.
Results
The response rate was 67%. All three surveys were completed by 133 adults with a slight preponderance of males (51%). Median age was 31 years, 117 were born with ARM and 16 with HD. All subgroups had significantly lower BFS than healthy references. ARM patients scored significantly lower than the healthy reference population when assessed for GIQoL. All showed significant impairment with the mental component summary (MCS) of SF-36. Patients with a successful bowel management had significantly higher scores on all three questionnaires than those with fecal accidents.
Conclusion
Our results emphasize the importance of a successful bowel management and its impact on the quality of life and bowel function. Long-term follow-up is recommended with attention to mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients born with an anorectal malformation (ARM) or Hirschsprung disease (HD) require surgical treatment in childhood. In patients with ARM, fecal incontinence may occur despite correct surgical repair, as this also depends on the severity and type of the ARM and associated anomalies [1]. In patients with HD fecal control should not be impaired after surgery provided the anal canal is intact [2, 3].
Quality of life and bowel function in patients born with ARM or HD has been previously reported for children by their parents or caregivers and by adolescent and adult patients [4,5,6,7,8,9,10,11,12,13,14,15]. Long-term studies of adult patients with ARM have shown that fecal continence is a strong predictor of quality of life (QoL) [11]. For those with HD, bowel function has been shown to deteriorate with age, with only slight impact on QoL [12]. Conversely, it has been observed that adult patients with ARM reported an improvement in fecal incontinence or soiling over time [9]. It remains unclear if this improvement is real, or if it is due to an inherent adaption to the individual’s condition and change in their expectations [8, 11]. However, it has also been shown that soiling, constipation, associated anomalies, severity of ARM, and presence of abdominal pain, all correlated significantly with patients’ psychosocial morbidity [16]. Treatment of fecal incontinence with a comprehensive bowel management program was described in 2009 by the senior authors [17]. Its impact on the quality of life in children with fecal incontinence has previously been reported [18]. Three months after implementation of a successful bowel management program, the fecal incontinence index (FII) as well as the quality of life (PedsQL 4.0) have shown statistically significant improvement.
Given the importance of fecal control for patient wellbeing, this study sought to evaluate gastrointestinal quality of life, bowel function and the influence of successful bowel management in adult patients with ARM and HD. Three validated instruments were used, Bowel Function Score (BFS), 36-item short-form health survey (SF-36) and Gastrointestinal Quality of Life (GIQoL), which assesses bowel function, physical and mental health components and quality of life system specific in patients with gastrointestinal disorders. It was hypothesized that adult patients with ARM or HD that experienced fecal incontinence without proper bowel management would report lower levels of gastrointestinal quality of life compared to a healthy population.
Methods
This was a cross sectional study of male and female patients born with either an ARM or HD who underwent surgical intervention by our team. Patients who were older than 18 years of age in the Adult Colorectal Research Registry were contacted to participate in the research study to assess bowel function and quality of life. Patients were sent electronic surveys through REDCap. REDCap is a secure, web-based application to capture data for clinical research [19]. Study enrollment occurred between October 2019 and August 2022. In addition to basic demographic information, general health, bowel management, fecal control, stool accidents and soiling were assessed. Patients were asked to complete three validated questionnaires: Bowel Function Score (BFS), the Gastrointestinal Quality of Life Index (GIQoLI) and the Short Form 36 Health Survey (SF-36).
Bowel function score (BFS)
Bowel function score (BFS) is a 7-item multivariate scoring system, including questions of fecal control and social impact due to bowel habits [5]. The participants score each question from zero to three, except for the question of stool frequency, which is scored from one to two. The scores are then summarized with a possible maximum score of 20, indicating good bowel control.
Gastrointestinal quality of life index (GIQOLI)
Gastrointestinal quality of life index (GIQOLI) was validated in 1995 and assesses the four dimensions of gastrointestinal symptoms, physical and social function, and emotional status. The participants answer each question on a five-point Likert scale from zero to four. Values are summed with a maximum score of 144 [20].
Short form 36 health survey (SF-36)
Short form 36 health survey (SF-36) was developed in 1992 and assesses eight health concepts, which are physical functioning, role limitations due to physical or emotional health problems, bodily pain, general health, vitality, social functioning, and mental health [20]. These scores are then presented as a physical component summary (PCS) and a mental component summary (MCS) subscore and understood as the physical and mental components of health, although these should always be interpreted in the context of all subscales [21, 22].
Patients were included in the study if they were confirmed to have a diagnosis of ARM or HD and completed all three questionnaires. The reported demographic data of the patients was linked to their surgical records to ensure accurate colorectal diagnoses. Bowel function and control was assessed and defined as clean, if no involuntary bowel movements occurred (fecal accidents or soiling), and not clean, when the patient reported to have fecal accidents or soiling, despite having a bowel regimen of either laxatives or enemas (antegrade or retrograde). Patients with an ostomy were excluded from the analysis of the BFS and analyzed separately.
Survey scores were summarized and reported as median (Q1, Q3) and compared to reported results of a healthy comparison study population in literature [20, 23, 24]. In addition, analysis was also performed comparing outcomes between the study population groups of ARM and HD to measures of patients with inflammatory bowel disease (IBD) reported in the literature [25,26,27].
One-sample Wilcoxon tests were used to compare BFS, GIQoL, and SF-36 scores to reference values from healthy and IBD populations [20, 23,24,25,26,27,28]. In some cases, the healthy reference values were the maximum possible subscore and thus no formal testing was conducting. Statistically significant p-values (< 0.05) indicate that the median score for a given diagnosis group within our study sample is significantly different from the reference value.
Additionally, two-sample Wilcoxon tests or Kruskal–Wallis tests were used to compare scores between bowel control subgroups. For statistically significant (p-value < 0.05) Kruskal–Wallis tests, post-hoc Dunn’s tests were used to identify statistically significant differences in pairwise comparisons between bowel control subgroups. Due to the exploratory nature of this study, p-values were not adjusted for multiple comparisons. Statistical analyses were performed using R Studio (versions 4.1.2). This study was approved by the Colorado Multiple Institutional Review Board (COMIRB #19–1050, 19–0899, 21–3153, 21–3154).
Results
Demographic summary
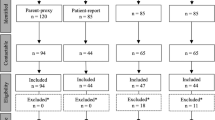
A total of 220 patients were contacted to participate in the study and 147 responded (67% response rate). There were 14 patients excluded due to missing documentation, diagnosis other than ARM or HD or because they did not answer all three questionnaires. One hundred and thirty-three adults completed all three surveys, with 63 females (47.4%), 68 males (51.1%), and two nonbinary participants (1.5%) (Table 1). Age ranged from 22 to 80 years, with a median of 31 years and a mean of 32.5 years. One hundred and seventeen were born with an ARM, of those, 38 (32.5%) were cloaca and seven (6%) had a complex malformation. Sixteen (12%) were born with HD. Four patients (3%) had a kidney transplant, three of whom were born with a cloaca. Thirty-six patients (27.1%) had an antegrade continence enema (ACE) procedure and seven patients (5.3%) have a permanent ostomy (colostomy or ileostomy).
Of these seven patients with an ostomy, six were female, one was male and their diagnoses included cloaca (4), covered cloacal exstrophy (1), total colonic aganglionosis (1), and ARM with recto-urethral prostatic fistula (1).
Bowel function score (BFS—Table 2)
All subgroups had significantly lower composite scores when compared to healthy reference values. Within the sub-scores statistically significant impairment was found for patients with cloaca and ARM for all categories except for stool frequency and social problems.
Gastrointestinal quality of life (GIQoLI—Tables 3, 4, 5)
Patients with ARM, cloaca or complex malformations had significantly lower composite scores when compared to healthy reference values. Patients with the diagnosis of cloaca (median score 99) or complex malformations (median score 100) had even lower composite scores than patients suffering from Crohn’s disease (reference score 103), or ulcerative colitis (reference score 110) [20, 25, 26]. In contrast, the HD group reached similar composite scores (reference score 125) as the healthy population (reference score 125.8).
SF-36 (Table 6)
Patients with cloaca were the only subgroup who had statistically significant lower scores for PCS. All patients scored lower for MCS, compared to healthy reference values, indicating impaired mental health. Patients with complex malformations, had the lowest scores for PCS and MCS within the subgroups. In comparison to patients with IBD, patients with complex malformations had lower scores across subscales, except for the subscores of role functioning-physical and emotional wellbeing.
Outcome based on fecal control (Tables 7, 8, 9, 10)
The study population was stratified by functional outcome (fecal accidents and soiling) and bowel management (either laxatives or enemas) regardless of their diagnosis. The majority of patients (51%) were clean with or without laxatives and 9.8% were clean with enemas (Table 7). Fecal accidents with laxative treatment occurred in 7.5% of patients and in 11.3% with enemas. Twenty patients who were having fecal accidents did not undergo formal bowel management (neither laxatives nor enemas) were excluded from the analysis.
Patients with bowel control or successful bowel management with laxatives had the highest scores among the patient subgroups, followed by patients who were clean on daily enemas (Table 8). There was a statistically significant difference the scores of BFS, GIQoL and PCS among the subgroups. This did not apply to MCS where all subgroups had similar low scores regardless of the bowel management type and outcome. Patients with an unsuccessful bowel management either on laxatives or enemas scored even lower than patients with an ostomy in the MCS.
When the patients were grouped as clean and not clean in the underwear (Table 9), the patients who stayed clean had statistically significantly higher scores (p < 0.05) than those who had fecal accidents, on all three questionnaires. Compared to healthy reference scores for all three validated instruments (BFS, SF-36 and GIQoL) all patients, regardless if they were clean or not clean in the underwear, scored significantly lower throughout all questionnaires (Table 10).
Ostomy
Seven patients had an ostomy. One respondent stated that she had the ostomy by choice and, but no further information was provided by the other six participants about why they had an ostomy. Significant differences in GIQoL and PCS score were seen when patients with an ostomy were compared to patients who were clean in the underwear (with or without laxatives). Ostomy patients had significantly lower scores (unadjusted p-values < 0.05) (Table 11). There was no statistical significance in GIQoL and PCS in patients with unsuccessful bowel management and accidents compared to patients with an ostomy (Table 11).
Discussion
This study assessed bowel function, gastrointestinal quality of life, and general health of adult ARM and HD patients using three different validated questionnaires. When available, scores were also compared with patients with inflammatory bowel disease, since this population also suffers from a chronic condition that impacts the gastrointestinal tract.
Consistent with prior published data [7], all patients in this study reported significant impairment on the BFS, suggesting poor bowel functioning and control. It is known that patients with ARM and HD require long-term follow-up, because even when they receive a technically correct operation, 75% of patients will require bowel management, most commonly laxatives or enemas. Due to the nature of this study, many enrolled patients were lost to follow-up at the time that questionnaires were sent and were not offered, or declined, bowel management. We believe that the next generation of adult patients will have stricter follow-up, as well as a more structured bowel management regimen, thanks to the spread of knowledge, awareness of patients and families, availability of colorectal centers offering bowel management, and initiatives for proper transition of care.
Regarding quality of life, patients with cloaca and other types of anorectal malformation had statistically significant lower scores compared to the healthy reference population. A possible explanation is again the fact that even in malformations with good prognosis for bowel control, who have received a technically correct operation, bowel management with daily routines is still needed. Previous reports of adult patients born with ARM and HD scored lower in GIQoL compared to a healthy population, indicating that bowel control affects quality of life [4, 8, 11, 12]. Our study did not confirm these findings for patients with HD, who in this study, had a similar score to the healthy population. We believe this may be due to the fact that HD is usually an isolated condition, and when the surgery is done correctly, these patients do not suffer from fecal incontinence, even though some of them may require laxatives.
As we chose patients with inflammatory bowel disease as a comparison group for GIQoL, and most scores had no statistical significance, we should also acknowledge that the majority of IBD cases have a later onset than ARM and HD (that are typically diagnosed at birth). This difference may reflect upon the ability to cope and adapt for patients with ARM and HD.
When examining health concepts, ARM and HD patients reported the same level of physical impairment in their daily life as healthy references. On the other hand, all patients showed significant lower scores, concerning for notable impairment of mental health in this population. These findings are supported by a recent study that reported ARM patients had a higher prevalence of depression and anxiety than the general population [28]. No significant association was found in regards of type and severity of malformation with the prevalence of depression or anxiety. This is also supported by our data, that regardless of the type of diagnosis, patients with congenital ARM or HD experience mental health problems. These findings highlight the importance of a multidisciplinary clinic, with long-term follow up including psychosocial providers to support those individuals who face mental health challenges, as a result of their congenital colorectal diagnoses. In addition, patients with ARM, cloacal anomaly, and complex malformations, frequently have associated anomalies that may impact their social functioning. For example, the need for intermittent catheterization, and frequency of UTI, these would not be commonly present for patients with HD and IBD.
Besides comparing patients by their diagnosis, patients were additionally compared by their bowel function, success of bowel management and fecal control. In both subgroups, clean versus not clean in the underwear, scoring was significantly worse than healthy references; however, the population who stayed clean in the underwear had scores closer to the healthy reference values. These results highlight the importance of a successful bowel management in patients born with ARM or HD, which likely leads to better overall functioning and quality of life. On the other hand, they also show that patients with an ostomy had similar scores as patients with unsuccessful bowel management. While it is challenging to understand why patients with ostomies may have impaired quality of life, it may be that this patient population is more medically complex or that the presence of an ostomy can affect on the patient’s functioning. Further studies are warranted to assess and compare patients with an ostomy versus patients with unsuccessful bowel management. One of the seven patients with an ostomy, stated that she had the ostomy by choice. Due to the small sample size, no statement can be made, but we could postulate that a patient who gets an ostomy by choice, might not have as low of scores in these assessed areas, compared to patients who required an ostomy.
Limitations of this study are the small sample size with respect to the specific types of ARMs. We were underpowered to compare them adequately, we suspect, the prognosis for bowel control and level of complexity will have a direct impact on functioning and quality of life. All results were self-reported data and therefore subject to various biases, however this was minimized by the use of validated instruments. In addition, this study was conducted during the COVID pandemic, where social restrictions occurred, which may have impacted the overall quality of life and mental health of the participants, to a various degree [29]. Since this is a cross-sectional study and reflects only a single evaluation in these adult patients, further longitudinal studies are warranted to better assess this patient population over time.
Conclusion
Patients with ARM and HD reported an impairment of quality of life measurements compared to healthy controls. This impairment is associated with poorer GI/fecal control symptoms which indicate that proper bowel management can positively impact overall quality of life. Our study also emphasizes the importance of long-term follow-up with special attention to mental health support.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Levitt MA, Peña A (2007) Anorectal malformations. Orphanet J Rare Dis 2:1–13. https://doi.org/10.1186/1750-1172-2-33
De la Torre L, Cogley K, Santos K, Morales O, Calisto J (2017) The anal canal is the fine line between “fecal incontinence and colitis” after a pull-through for Hirschsprung disease. J Pediatr Surg 52:2011–2017. https://doi.org/10.1016/j.jpedsurg.2017.08.040
Bischoff A, Frischer J, Knod JL, Dickie B, Levitt MA, Holder M et al (2017) Damaged anal canal as a cause of fecal incontinence after surgical repair for Hirschsprung disease—a preventable and under-reported complication. J Pediatr Surg 52:549–553. https://doi.org/10.1016/j.jpedsurg.2016.08.027
Neuvonen MI, Kyrklund K, Lindahl HG, Koivusalo AI, Rintala RJ, Pakarinen MP (2015) A population-based, complete follow-up of 146 consecutive patients after transanal mucosectomy for Hirschsprung disease. J Pediatr Surg 50:1653–1658. https://doi.org/10.1016/j.jpedsurg.2015.02.006
Rintala RJ, Lindahl HG, Rasanen M (1997) Do children with repaired low anorectal malformations have normal bowel function? J Pediatr Surg 32:823–826. https://doi.org/10.1016/S0022-3468(97)90628-X
Meinds RJ, van der Steeg AFW, Sloots CEJ, Witvliet MJ, de Blaauw I, van Gemert WG et al (2019) Long-term functional outcomes and quality of life in patients with Hirschsprung’s disease. Br J Surg 106:499–507. https://doi.org/10.1002/bjs.11059
Nah SA, Ong CCP, Saffari SE, Ong LY, Yap TL, Low Y et al (2018) Anorectal malformation & Hirschsprung’s disease: a cross-sectional comparison of quality of life and bowel function to healthy controls. J Pediatr Surg 53:1550–1554. https://doi.org/10.1016/j.jpedsurg.2017.08.018
Rintala R, Mildh L, Lindahl H (1994) Fecal continence and quality of life for adult patients with an operated high or intermediate anorectal malformation. J Pediatr Surg 29:777–780. https://doi.org/10.1016/0022-3468(94)90368-9
Fernandes M, Aminoff D, Violani C, Grano C (2020) Positive orientation and health-related quality of life in adult patients born with anorectal malformations. J Pediatr Gastroenterol Nutr 71:298–303. https://doi.org/10.1097/MPG.0000000000002803
Grano C, Bucci S, Aminoff D, Lucidi F, Violani C (2013) Quality of life in children and adolescents with anorectal malformation. Pediatr Surg Int 29:925–930. https://doi.org/10.1007/s00383-013-3359-8
Grano C, Aminoff D, Lucidi F, Violani C (2011) Long-term disease-specific quality of life in adult anorectal malformation patients. J Pediatr Surg 46:691–698. https://doi.org/10.1016/j.jpedsurg.2010.10.016
Jarvi K, Laitakari EM, Koivusalo A, Rintala RJ, Pakarinen MP (2010) Bowel function and gastrointestinal quality of life among adults operated for hirschsprung disease during childhood: a population-based study. Ann Surg 252:977–981. https://doi.org/10.1097/SLA.0b013e3182018542
Kyrklund K, Pakarinen MP, Rintala RJ (2017) Long-term bowel function, quality of life and sexual function in patients with anorectal malformations treated during the PSARP era. Semin Pediatr Surg 26:336–342. https://doi.org/10.1053/j.sempedsurg.2017.09.010
Davidson JR, Kyrklund K, Eaton S, Pakarinen MP, Thompson DS, Cross K et al (2021) Long-term surgical and patient-reported outcomes of Hirschsprung disease. J Pediatr Surg 56:1502–1511. https://doi.org/10.1016/j.jpedsurg.2021.01.043
Moore SW, Albertyn R, Cywes S (1996) Clinical outcome and long-term quality of life after surgical correction of Hirschsprung’s disease. J Pediatr Surg 31:1496–1502. https://doi.org/10.1016/S0022-3468(96)90164-5
Hamid CH, Holland AJA, Martin HCO (2007) Long-term outcome of anorectal malformations: the patient perspective. Pediatr Surg Int 23:97–102. https://doi.org/10.1007/s00383-006-1841-2
Bischoff A, Levitt MA, Peña A (2009) Bowel management for the treatment of pediatric fecal incontinence. Pediatr Surg Int 25:1027–1042. https://doi.org/10.1007/s00383-009-2502-z
Colares JHF, Purcaru M, da Silva GPF, Frota MA, da Silva CAB, Melo-Filho AA et al (2016) Impact of the bowel management program on the quality of life in children with fecal incontinence. Pediatr Surg Int 32:471–476. https://doi.org/10.1007/s00383-016-3874-5
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E et al (1995) Gastrointestinal quality of life index: development, validation and application of a new instrument. Br J Surg 82:216–222. https://doi.org/10.1002/bjs.1800820229
Taft C, Karlsson J, Sullivan M (2001) Do SF-36 summary component scores accurately summarize subscale scores? Qual Life Res 10:395–404. https://doi.org/10.1023/A:1012552211996
Ware J E, Snow K K, Kosinski M, Gandek B. SF-36 health survey: Manual and Interpretation Guide. 1993. The Health Institute, New England Medical Center, Inc., Box 345, 750 Washington Street, Boston Massachusetts 02111.
Kyrklund K, Koivusalo A, Rintala RJ, Pakarinen MP (2012) Evaluation of bowel function and fecal continence in 594 finnish individuals aged 4 to 26 years. Dis Colon Rectum 55:671–676. https://doi.org/10.1097/DCR.0b013e31824c77e4
Ware JE, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P et al (1998) The factor structure of the SF-36 Health Survey in 10 countries: Results from the IQOLA Project. J Clin Epidemiol 51:1159–1165. https://doi.org/10.1016/S0895-4356(98)00107-3
Thaler K, Dinnewitzer A, Oberwalder M, Weiss EG, Nogueras JJ, Wexner SD (2005) Assessment of long-term quality of life after laparoscopic and open surgery for Crohn’s disease. Color Dis 7:375–381. https://doi.org/10.1111/j.1463-1318.2005.00769.x
Leowardi C, Hinz U, Tariverdian M, Kienle P, Herfarth C, Ulrich A et al (2010) Long-term outcome 10 years or more after restorative proctocolectomy and ileal pouch-anal anastomosis in patients with ulcerative colitis. Langenbeck’s Arch Surg 395:49–56. https://doi.org/10.1007/s00423-009-0479-7
Ling F, Tu L, Li J, Chen Y, Xu M, Zhu L (2021) Psychological aspect of patients with inflammatory bowel disease, which may be related to the quality of life, sleep and disease characteristics. Scand J Gastroenterol 56:1328–1336. https://doi.org/10.1080/00365521.2021.1966093
Judd-Glossy L, Ariefdjohan M, Ketzer J, Wehrli LA, Pena A, de la Torre L et al (2022) Long-term outcomes of adult patients following surgery for congenital colorectal conditions: analysis of psychosocial functioning. Pediatr Surg Int 38:1685–1692. https://doi.org/10.1007/s00383-022-05212-0
Ferreira LN, Pereira LN, da Fé BM, Ilchuk K (2021) Quality of life under the COVID-19 quarantine. Qual Life Res 30:1389–1405. https://doi.org/10.1007/s11136-020-02724-x
Author information
Authors and Affiliations
Contributions
L.A.W. and M.L.R. wrote the main manuscript text. L.A.W., J.M.R. and E.H.C. prepared the tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wehrli, L.A., Reppucci, M.L., De La Torre, L. et al. Gastrointestinal quality of life and bowel function in adults born with anorectal malformation and hirschsprung disease. Pediatr Surg Int 39, 234 (2023). https://doi.org/10.1007/s00383-023-05516-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05516-9