Abstract
Purpose
To evaluate outcomes of adopting the Swenson-like technique in transanal pull-through for Hirschsprung disease (HD) at a children’s institution in Southeast Asia.
Methods
A retrospective chart review was performed over 42 months at a safety-net pediatric hospital in Vietnam.
Results
From January 2019 to June 2022, the Swenson-like technique was implemented and performed on 139 patients (115 male, 24 female, mean age 6.4 ± 11.96 months). There were 123 transanal-only resections, 5 transanal plus laparoscopic, and 11 transanal plus laparotomy. The mean operative time was 70.9 ± 43.6 min. The average length of the resected specimen was 18.8 ± 10.9 cm. No urethral or vaginal injuries occurred. Postoperative complications included 1 anastomotic leak (0.7%), 4 anastomotic stenoses (2.8%), and 2 perianal abscesses in the setting of recurrent enterocolitis (1.4%). With a mean follow-up of 26 ± 11.9 months (range 3–48 months), there were 25 enterocolitis cases (17.9%), 45 patients with constipation (32.3%), 1 episode of fecal incontinence lasting longer than 6 months (0.7%), and 1 rectal-vestibular fistula noted one year postoperatively (0.7%). There were no deaths.
Conclusion
The Swenson-like technique in transanal pull-through for Hirschsprung's disease was safely adopted at our institution. The results show that applying this technique uniformly in a single institution led to excellent outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With an improved understanding of the pathogenesis and genetic roots of Hirschsprung disease (HD), the treatment of HD has significantly improved. However, diagnostic and postoperative obstructive complications remain especially problematic in low- and middle-income countries with limited resources. For example, many providers worldwide do not have access to anorectal manometry, have limited experience in pathology, lack any bowel management program, and are not able to use Botulinum toxin due to a lack of availability or approval for use in children in their country. In the face of these challenges, we set out to improve the surgical approach at our institution with the hope that we could minimize postoperative problems.
The standard Swenson procedure was previously felt to have many postoperative complications due to a deep pelvic dissection [1], while the Yancey-Soave procedure which was developed to avoid the problems with the Swenson can be complicated by a cuff consisting of aganglionic muscle [2]. In the Duhamel pouch, also adopted to respond to a problem encountered by the Swenson, a non-ganglionic bowel segment can cause chronic constipation or recurrent enterocolitis [3]. Swenson always believed that his original description was a good operation and that complications resulted from a rectal dissection in a perirectal plane that was too wide [4, 5]. In 2003, Weidner and Waldhausen brought back the Swenson approach and reported 15 cases of a transanal pull-through using the Swenson procedure [6] with excellent results. Following their success, several surgeons began applying the transanal Swenson technique, adhering to a strict perirectal dissection, with excellent results [7,8,9]. In 2013, the “Swenson-like” transanal pull-through was promoted and again became one of the standard techniques used [10]. This technique has both the advantages of a rectal dissection done through the anus (taking advantage of this idea offered by Langer and De la Torre [11]) as well as avoiding the use of a cuff of aganglionic segment except for the 0.5 to 1 cm of the original columnar epithelium left intact just proximal to the dentate line. This approach has been found to minimize postoperative mechanical and functional bowel obstruction.
Given this history, and in our attempt to reduce postoperative complications, our institution in Vietnam began adopting this technique in January 2019. Prior to this, a transanal endorectal pull-through (TEPT) using the Yancey/Soave procedure but without a standardized cuff length was the most common technique performed in Vietnam [12,13,14]. Liem et al. first reported in 1995 results with the standard Swenson procedure in Vietnamese Hirschsprung disease patients with 3 stages with satisfactory results [15]. No additional studies on the traditional Swenson technique or the transanal version of it have since been published in our country.
Materials and methods
We reviewed patients between January 2019 and June 2022 who underwent a transanal Swenson-like pull-through for Hirschsprung disease at a single institution. As a tertiary care children’s facility, our hospital serves patients under the age of 16 and is located in the largest metropolitan area in the country. Patient demographics, associated abnormalities, clinical signs, pathologic results, contrast enema, surgical features, and early and late postoperative complications were collected. We excluded 8 cases of total colonic aganglionosis using the "Swenson-like" technique in transanal pull-through due to incomplete data.
At our institution, all children with Hirschsprung disease underwent surgery at the time of their diagnosis. That diagnosis was based on consistent history, physical exam, contrast enema, and a full-thickness rectal biopsy. (suction rectal biopsy is not available at our hospital). All patients had a preoperative mechanical bowel preparation and a gradually reduced fiber diet three days before surgery. Colon cleansing was confirmed preoperatively by ensuring that the patient was expelling clear fluid without any stool. The patients’ families were trained to give their children rectal irrigations. Patients were given general anesthesia with a caudal block and then placed in the lithotomy position with pillows to raise the buttocks. The primary surgeon stood at the foot of the bed to operate with two assistant surgeons on either side. Foley catheter drainage of the bladder was used for male patients or patients with a transabdominal approach and was subsequently discontinued 24 h postoperatively.
First, an exam under anesthesia and anal dilation was performed. The Lone Star Retractor System (Lone Star [CooperSurgical]), a lightweight self-retaining ring retractor utilizing hooks designed for anorectal surgery, was placed at the level of the mucocutaneous junction of the anal canal and then moved deeper to lower the dentate line and protect the anal canal.
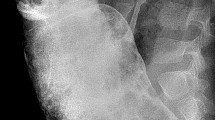
Interrupted 4–0 or 5–0 sutures were circumferentially sutured to the rectal mucosa 5 mm above the dentate line (≤ 3 months old) and 10 mm (> 3 months old) (Fig. 1) to provide uniform traction on the rectum during dissection. A needle-point monopolar electrocautery with the lowest possible energy level ensures tissue cutting and hemostasis without damaging surrounding tissue. After incising the mucosa with needle-point cautery, a full-thickness rectal wall dissection was performed. The hooks of the Lone star retractor were then moved deeper to expose the operative field. The dissection was continued in the Swenson plane until the colon was accessible in the abdominal cavity. Of note, intraoperative pathology and frozen sectioning were not available at our institution. The colon was grossly visualized gradually through its strictured segment, then through the transition zone, and to the dilated soft-walled colon above the transition zone for at least 10 cm. The healthy colon was then attached to the preserved anal canal just proximal to the dentate line by a single layer of 5–0 synthetic absorbable suture. A “donut” of the colon at the anastomotic line was resected and sent to the pathology department to analyze for the presence of hypertrophic nerves and the distribution of ganglion cells circumferentially.
After the operation, infants were breastfed on postoperative day 2. Infants older than six months and formula-fed infants were given clear liquid from postoperative day two and resumed routine oral feeding on postoperative day five. Pediatric patients are supported with parenteral nutrition while nil per os. All pediatric patients received intravenous antibiotics against Gram-negative and anaerobic bacteria during their hospital stay and were continued oral metronidazole after discharge until the day of clinic follow-up.
Discharge criteria included toleration of oral diet, presence of bowel movements, and lack of abdomen distension.
Patients were then scheduled for a follow-up visit in 2 to 3 weeks for postoperative examination and to guide parents on anal dilation. Families were educated on performing enemas when their child developed a distended abdomen and loose, smelling foul stools.
The data during follow-up visits were collected by a team of colorectal surgeons in person and by phone. Complications of enterocolitis were noted when the patient had loose, foul-smelling, or bloody stools and a distended abdomen requiring rectal irrigation. Constipation was defined as having fewer than three bowel movements in a week, having hard stools (Bristol Stool Form type 1 and 2), or requiring a laxative. Fecal soiling or stooling accidents were defined as small amounts of stool that required scraping off from underclothing at least twice per week in children greater than 3 years of age. Children over 3 years of age were assessed for fecal and urinary continence. Fecal continence was defined as the patient having voluntary bowel movements and ≤ 1 stooling accident per week.
Descriptive statistics were used to calculate quantitative data including mean values and proportions. Frequency and proportions were used to summarize the qualitative data.
Results
During the study period of 42 months, 139 patients (115 boys and 24 girls) who underwent the transanal Swenson-like pull-through procedure for Hirschsprung disease at our institution were identified for analysis. The mean age of the children at the time of operation was 6.4 ± 11.96 months with an age range of 13 days – 8 years old. There were 28 neonatal cases (20.1%) (under one month of age). There were 9 patients who were diagnosed after the age of 2 years (6.5%). Only 14 children lived in Ho Chi Minh City (10.1%). Most children lived outside of the city (89.9%) with an average travel time of 5.8 h and nearly half (43.7%) traveling more than 5 h (range 5–31 h) to reach our institution.
Patients demonstrated classic preoperative signs and symptoms including failure to pass meconium within 24 h (95.7%), abdominal distension (93.5%), and high-pressure rectal decompression (“blast sign”) (41.0%). Enterocolitis was found to occur in 30.2% of patients preoperatively. Three patients (2.2%) had a stoma. One patient presented with associated congenital abnormalities: Tetralogy of Fallot and Down syndrome (0.7%).
The contrast enema revealed a transition zone in the rectum (51.1%), the lower half of the sigmoid colon (23.7%), the upper half of the sigmoid colon (10.1%), descending colon (6.5%), and the splenic flexure (8.6%). In this study, 16 patients (11.5%) received genetic testing, seven of whom had anomalies (43.7%). Genetic defects included RET, NRG1, NDNRB, and ZEB2.
Of the 139 patients who underwent surgery, 123 (88.5%) cases had a transanal-only resection, 11 (7.9%) had transanal plus laparotomy, and 5 (3.6%) had transanal plus laparoscopy. The average length of the resected colon was 18.8 ± 10.9 cm, which subdivided as 16.1 ± 6.8 cm for the transanal-only group, 41 ± 15.6 cm for laparotomy-assisted group, 41.2.1 ± 20.9 cm for laparoscopy-assisted group. There were 79 (56.8%) cases that had a size mismatch between the two bowel ends that required intestinal plication, of which 54 (38.9%) had medial plication only and 25 (17.9%) required medial and lateral plication of the bowel. The mean operative time was 70.9 ± 43.6 min. No injuries to the urethra or vagina were observed during surgery. There were no patients who required intraoperative blood transfusions.
The time to the first bowel movement was 2 ± 0.8 days. The mean time for initiating a regular diet was 4.1 ± 0.9 days. The length of postoperative hospitalization was 8.6 ± 3.8 days.
The operative complications have been assessed. There was one (0.7%) incident of anastomotic leakage. This was a 29-month-old boy who presented with delayed passage of meconium and persistent constipation since the age of 6 months. The transition zone was found in the rectum, and the anastomosis was performed in the setting of a large size mismatch, requiring intestinal plication at both medial and lateral positions. On postoperative day 5, he developed distension and fever prompting his return to the operating room. A transverse colostomy was matured and then reversed 3 months later. No cases of intraabdominal abscesses were identified.
The mean follow-up period after surgery was 26 ± 11.9 months. There were 25 (17.9%) cases of post-operative enterocolitis occurring in the first 6 months. The youngest child presented with enterocolitis at 37 days of age while the oldest presented at age 4 years. Nine patients had a history of preoperative enterocolitis (36%). Four cases had long-segment aganglionosis (16%). An additional four children were found to have genetic anomalies, including 2 cases with RET mutations (8%), 1 case with ZEB2 mutations (4%), and 1 case with both EDNRB and NRG1 mutations (4%). Seventeen patients had only one episode of enterocolitis (68%), while eight had more than 2 episodes (32%). Six patients (24%) were hospitalized for treatment of enterocolitis with intravenous antibiotics and rectal irrigations, of which 4 patients (66.7%) had anastomotic strictures that responded well to anal dilation. The remaining 19 cases of enterocolitis were treated as outpatients with oral metronidazole and rectal irrigations (76%).
Two patients (1.4%) presented with postoperative perianal abscesses. The first patient was a 12-month-old girl who had two episodes of post-operative enterocolitis and subsequently developed an abscess and then anal fistula 6 weeks after surgery. She returned to the operating room, where a transverse colostomy was matured and later reversed after 1 year. During the past 10 months, the patient has had normal bowel movements without recurrent abscess or fistula. The second patient was a 28-month-old girl who developed a perianal abscess 3 weeks after the surgery. Intraoperatively, the colon was noted to have a significant size mismatch requiring intestinal plication along both the medial and lateral positions. She was treated operatively with a transverse colostomy, which was taken down after 8 months. The anal fistula recurred eight months later requiring a return to the operating room and the creation of another colostomy. There was one patient (0.7%) with Down syndrome and tetralogy of Fallot who was operated on at 1.5 months of age, then had multiple episodes of enterocolitis and had a rectal-vestibular fistula which developed 1 year after surgery.
Postoperative constipation was observed in 45 (32.3%) patients, including those with fewer than 3 bowel movements per week or those using laxatives. All patients diagnosed with postoperative enterocolitis or constipation had ganglion cells circumferentially at the anastomosis and no hypertrophic nerves on pathology.
Forty-four patients (33.1%) were at least 3 years of age and could be assessed for fecal and urinary continence. The average follow-up time after surgery was 32.7 ± 8.3 months. 97.7% had fecal continence, while one patient (2.2%) still had fecal soiling. This was a 38-month-old boy who underwent a pull-through of the descending colon that still had loose stools > 10 times/day at the six-month follow-up. All patients voided spontaneously with urinary control. There were no episodes of postoperative urinary retention. All male patients had spontaneous erections.
Finally, there were no deaths in the study.
Discussion
With the near-complete resection of the aganglionosis, the Swenson procedure provides the best pathologic resolution of HD. However, many surgeons may be hesitant to perform the Swenson approach due to the extensive pelvic dissection for rectal mobilization and reported high risk for postoperative complications [1]. Levitt et al. popularized the "Swenson-like" technique in transanal pull-through by demonstrating its safety and feasibility with very low complication rates [10]. As a result, many pediatric surgeons gradually became more empowered to apply this surgical technique [17, 18]. With promising results internationally, we suspected that we could also adopt this technique in Vietnam successfully, with the anticipation that our postoperative outcomes would be improved from previous techniques which were not standardized across our institution.
Regarding the early complications of the surgery, our study had 1 (0.7%) anastomotic leak, 4 (2.8%) anastomotic strictures, 2 (1.4%) perianal abscesses, no intraabdominal abscesses, and no urethral or vaginal injury, but on rectovestibular fistula. These rates are low when compared to the standard Swenson procedure [1, 5, 16]. The anastomotic leak and perianal abscesses occurred in patients with delayed diagnosis in children over the age of 2 years with a significant size mismatch noted prior to the anastomosis. In pediatric HD patients diagnosed after the age of 2 years, Rentea et al. [17] suggest that single-stage transanal-only pull-through should only be performed in pediatric patients with a low transition, specifically from below the sigmoid colon and minimally dilated colonic diameter. In our study, 9 (6.5%) cases were diagnosed after 2 years of age, however, the colon in most cases was dilated (Fig. 2). Prior to anastomosis, most patients (56.8%) required intestinal plication to reduce the size of the colon due to size mismatch. Perhaps the significant size mismatch coupled with postoperative enterocolitis led to the postoperative abscesses in these two patients.
The rate of enterocolitis after surgery in pediatric patients outside the neonatal age in our study was 17.9%, which is comparable to current literature [10, 17, 19]. In the cohort of patients with enterocolitis, there were 4 (2.8%) anastomotic strictures, 1 (0.7%) Trisomy 21, and 4 (2.8%) other genetic abnormalities. Some reasons for the rate of postoperative enterocolitis may include that most cases had large dilated colonic diameters with significant size mismatch, delayed diagnosis beyond the neonatal period, and more than one-third (9/25) of cases had a long aganglionic segment, all of which may have been contributors to postoperative stasis. Although we instructed family members to perform routine postoperative rectal irrigation, we were unable to monitor the compliance and effectiveness of their irrigations due to the challenges of traveling to the hospital for follow-up visits and inadequate availability of facilities for our patients during the Covid-19 pandemic. Most (89.9%) patients in our study lived outside the city and far from medical centers. Finally, we also note the limitations of pathology at our institution that may have resulted in unidentified cases of transition zone pull-throughs. Although histopathological specimens of the colon at the anastomosis are reported to demonstrate circumferentially distributed ganglion cells and no hypertrophic nerve fibers, this report relies on the subjective opinion of the pathologist at our institution. Our institution does not have the ability to accurately measure the size of the nerves, and no immunohistochemical staining of the anastomotic colon is performed if the pathologist notes the presence of ganglion cells. Therefore, we preliminarily accept that the segment of the colon that has been pulled through is healthy bowel, and thus no cases of transition zone pull-throughs were histologically identified in our study. However, in patients with obstructive symptoms that persist after maximal treatment with irrigations, neo-rectal biopsies are performed, the new specimens analyzed by pathology, and decisions are made regarding the need for redo pull-through. We did not have any such cases but recognize their potential.
When compared to other studies [18, 19], both hospital stay and time to regular diet were longer in our study. Because most patients had dilated colons, we proceeded conservatively and withheld a normal diet by mouth immediately after surgery. Patients received parenteral nutrition and were given clear liquids on postoperative days two through five. Infants were given early feeding. Furthermore, most patients live far from the hospital without access to adequate surgical care locally. We are thus also very cautious to discharge patients and make sure to confirm tolerance of regular diet, adequate oral hydration, soft reassuring abdominal exam, presence of bowel movements, and absence of urinary retention prior to discharge.
When first adopting the transanal “Swenson-like” technique at our institution, we were initially concerned about the risk of intraoperative injury to adjacent structures such as the urethra or vagina. However, we carefully followed the instructions of the technical documentation [10, 20], and similar to published reports [10, 17, 18], we had no cases of urethral or vaginal injury. We found that the circumferential sutures at the rectum not only provided uniform traction on the rectum but also aided in making the first rectal mucosal incision. We found that pinching and twisting the sutures (Fig. 1B) optimized the plane to a right angle with the tip of the needle-point cautery and helps the rectum not to adhere closely to adjacent structures during dissection. We utilized monopolar electrocautery with a needle-point tip at low energy settings, which helped to cut and coagulate bleeding accurately, minimizing thermal spread to surrounding tissues during this challenging dissection close to the rectum.
There were no cases of postoperative urinary retention. All patients over 3 years of age demonstrated urinary continence. All male patients had a spontaneous erection after surgery. These findings are quite different from the articles noting these complications for the original Swenson procedure [15, 21]. There were 32.3% that had postoperative constipation, which is similar to previously published studies [10, 22]. These patients with postoperative constipation did not have anastomotic strictures. However as described above, while pathology reported the circumferential presence of ganglion cells, we were unable to definitively rule out transition zone pull-throughs. Second, while postoperative functional evaluation is critical in the management of patients who have undergone a pull-through, anorectal manometry is not available at our institution. Finally, botulinum toxin injection is not yet approved for use in the achalasia of the internal anal sphincter in children in Vietnam. Many children in Vietnam have suffered from constipation and were treated with an osmotic laxative and anal dilation.
Despite this, we still found 43 out of 44 patients over 3 years of age had voluntary bowel movements and no fecal soiling at the conclusion of the study. Compared to the standard Swenson procedure described by Liem et al. [15] which had 8% of patients had fecal incontinence and 2% had stress urinary incontinence, our study showed better results in fecal and urinary continence (2.2% < 8% and 0% < 2%, respectively).
We do not have the mid- to long-term results of HD surgery before 2019 at our institution to compare with the results when applying the new technique. Before 2019, we only applied the transanal endorectal pull-through technique. During that period, the Yancey/Soave cuff length was left at the discretion of the surgeon, anywhere from 3 to 5 cm. The matched case–control comparison of Soave and Swenson techniques by Nasr et al. with very short rectal cuff Soave (1 to 2 cm) showed no significant difference in short- and medium-term outcomes between the two different technical approaches [22].
Conclusion
The results demonstrate that the "Swenson-like" technique in transanal pull-through in the surgical treatment of HD is a safe technique that has been adopted by our institution. While we may lack the facilities, equipment, and experience in diagnosing and treating obstructive problems post pull-through of HD, optimization in surgical technique to effectively eliminate the aganglionic segment should be considered. Of course, there are other factors that can affect the obstructive problems post pull-through of HD, such as early diagnosis; nursing treatment such as instructing proficient rectal irrigation before surgery to avoid dilated colon and preoperative enterocolitis; the view of leveling ostomy for cases have large dilated colon; meticulous postoperative care, etc., but while optimizing the approaches, the changing the surgical approach is also very helpful in excluding mechanical and functional causes of obstruction due to residual seromuscular cuff or Duhamel pouch. However, we recognize the limitations of a retrospective single-institution study. More long-term investigations and randomized controlled studies are needed to weigh the advantages and disadvantages of this technique compared to other pull-through techniques.
Data availability
Due to regulatory privacy and ethical concerns, neither the data nor its source code in this study can be made available to the public. Future information about the data you may contact to corresponding author. Submission for data sharing will be reviewed by the Institutional Review Board of Children's Hospital 1, Ho Chi Minh City, Vietnam.
References
Madonna MB, Luck SR, Reynolds M et al (1998) Swenson procedure for the treatment of Hirschsprung’s disease. Semin Pediatr Surg 7:85–88. https://doi.org/10.1016/S1055-8586(98)70018-6
Soave F (1964) Hirschsprung’s disease: a new surgical technique. Arch Dis Child 39:116–124. https://doi.org/10.1136/adc.39.204.116
Duhamel B (1960) A New operation for the treatment of hirschsprung’s disease. Arch Dis Child 35:38–39. https://doi.org/10.1136/adc.35.179.38
Swenson O, Bill AH (1948) Resection of rectum and rectosigmoid with preservation of the sphincter for benign spastic lesions producing megacolon; an experimental study. Surgery 24:212–220
Sherman JO, Snyder ME, Weitzman JJ et al (1989) A 40-year multinational retrospective study of 880 swenson procedures. J Pediatr Surg 24:833–838. https://doi.org/10.1016/S0022-3468(89)80548-2
Weidner BC, Waldhausen JHT (2003) Swenson revisited: a one-stage, transanal pull-through procedure for Hirschsprung’s disease. J Pediatr Surg 38:1208–1211. https://doi.org/10.1016/S0022-3468(03)00269-0
Mahajan JK, Rathod KK, Bawa M, Narasimhan KL (2011) Transanal Swenson’s operation for Recto-sigmoid Hirschsprung’s disease. Afr J Paediatr Surg 8:301. https://doi.org/10.4103/0189-6725.91678
Sookpotarom P, Vejchapipat P (2009) Primary transanal Swenson pull-through operation for Hirschsprung’s disease. Pediatr Surg Int 25:767–773. https://doi.org/10.1007/s00383-009-2428-5
Xu Z, Zhao Z, Wang L et al (2008) A new modification of transanal Swenson pull-through procedure for Hirschsprung’s disease. Chin Med J 121:2420–2423
Levitt MA, Hamrick MC, Eradi B et al (2013) Transanal, full-thickness, Swenson-like approach for Hirschsprung disease. J Pediatr Surg 48:2289–2295. https://doi.org/10.1016/j.jpedsurg.2013.03.002
De La Torre L, Langer JC (2010) Transanal endorectal pull-through for Hirschsprung disease: technique, controversies, pearls, pitfalls, and an organized approach to the management of postoperative obstructive symptoms. Semin Pediatr Surg 19:96–106. https://doi.org/10.1053/j.sempedsurg.2009.11.016
Liem NT, Hau BD (2006) Primary laparoscopic endorectal colon pull-through for Hirschsprung’s disease: early results of 61 cases. Asian J Surg 29:173–175. https://doi.org/10.1016/S1015-9584(09)60081-6
Hau BD, Quynh TA, Anh VH, Liem NT Early and Late Outcomes of Primary Laparoscopic Endorectal Colon Pull-Through Leaving a Short Rectal Seromuscular Sleeve for Hirschsprung Disease. 4
Vũ PA, Thien HH, Hiep PN (2010) Transanal one-stage endorectal pull-through for Hirschsprung disease: experiences with 51 newborn patients. Pediatr Surg Int 26:589–592. https://doi.org/10.1007/s00383-010-2599-0
Liem NT, Hau BD, Thu NX (1995) The long-term follow-up result of Swenson’s operation in the treatment of Hirschsprung’s disease in Vietnamese children. Eur J Pediatr Surg 5:110–112. https://doi.org/10.1055/s-2008-1066180
Clausen EG, Davies OG (1963) Early and late complications of the Swenson pull-through operation for Hirschsprung’s disease. The American Journal of Surgery 106:372–380. https://doi.org/10.1016/0002-9610(63)90026-6
Rentea RM, Halleran DR, Ahmad H et al (2019) Transanal-only Swenson-like pull-through for late diagnosed Hirschsprung disease. J Surg Case Rep 2019:341
Mohamed W, Elsawaf MI, Shalaby AI et al (2021) Optimism for the Single-stage Transanal Swenson in Neonates. J Indian Assoc Pediatr Surg 26:16–22. https://doi.org/10.4103/jiaps.JIAPS_187_19
Singh R, Cameron BH, Walton JM et al (2007) Postoperative Hirschsprung’s enterocolitis after minimally invasive Swenson’s procedure. J Pediatr Surg 42:885–889. https://doi.org/10.1016/j.jpedsurg.2006.12.055
Levitt MA, Vilanova-Sanchez A (2020) Pediatric colorectal and pelvic reconstructive surgery. CRC Press, Boca Raton
Moore SW, Albertyn R, Cywes S (1996) Clinical outcome and long-term quality of life after surgical correction of Hirschsprung’s disease. J Pediatr Surg 31:1496–1502. https://doi.org/10.1016/s0022-3468(96)90164-5
Nasr A, Haricharan RN, Gamarnik J, Langer JC (2014) Transanal pullthrough for Hirschsprung disease: Matched case–control comparison of Soave and Swenson techniques. J Pediatr Surg 49:774–776. https://doi.org/10.1016/j.jpedsurg.2014.02.073
Acknowledgements
The authors wish to thank Dr. Marc Levitt and the Colorectal Team Overseas (www.ctoverseas.org) for performing the transanal Swenson-like pull-through for the first time for Vietnamese Hirschsprung patients. We also thank Dr. Levitt (Children's National Hospital, the George Washington School of Medicine, Washington D.C) for his help with editing the manuscript.
Author information
Authors and Affiliations
Contributions
CRediT authorship contribution statement: Bich-Uyen Nguyen: Conceptualization, Methodology, Data curation, Formal analysis, Visualization, Writing - original draft, Writing - review & editing, Project administration. Megan Vu: Visualization, Writing - original draft, Writing - review & editing. Quoc-Tung Pham: Data curation, Formal analysis. Viet-Hung Nguyen Phung: Data curation, Formal analysis. Quynh-Nhu Nguyen Dang, Thin Thai, Duc-Trong Le Vo, Thanh Thi Tran, Man Minh Huynh, Quynh Kim Huynh: Investigation. Thoi Kim Ngo: Supervision. Hieu Trung Dao: Supervision and Review. The authors wish to thank Dr. Marc Levitt and the Colorectal Team Overseas (www.ctoverseas.org) for performing the transanal Swenson-like pull-through for the first time for Vietnamese Hirschsprung patients. We also thank Dr. Levitt (Children's National Hospital, the George Washington School of Medicine, Washington D.C) for his help with editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nguyen, BU., Vu, M.T., Pham, QT. et al. Adopting the Swenson-like technique for patients with Hirschsprung disease in Vietnam. Pediatr Surg Int 39, 124 (2023). https://doi.org/10.1007/s00383-023-05415-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05415-z