Abstract
Purpose
Patients with biliary atresia (BA) and cytomegalovirus (CMV) infection may have poorer outcomes after Kasai portoenterostomy (KPE) than uninfected patients, suggesting a rationale for antiviral treatment (AVT). We aimed to describe the incidence of CMV infection and of AVT in BA patients, and to detect any differences between infected and uninfected patients to conclude if AVT is of use.
Methods
Data on BA patients who underwent KPE 2004–2020 were retrospectively collected, and the outcome was analyzed with regard to CMV status.
Results
Fifteen out of forty-six (33%) BA patients had signs of ongoing CMV infection. They did not differ significantly from the CMV-negative patients regarding rate of prematurity, birth weight, or biochemical markers but were slightly older at KPE. All patients received steroids postoperatively and all patients with ongoing CMV infection received AVT with very good effect on viremia and without major side effects. The AVT consisted of oral valganciclovir (10–40 (– 58) mg/kg/d) or intravenous ganciclovir (5.3–11 mg/kg/d).
Conclusion
Ongoing CMV infection is common in this group of patients. The viremia can effectively be treated with AVT without any major side effects. Larger, randomized studies are needed to clarify the possible effect on clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biliary atresia (BA) is a severe cholangiopathy in infants with an etiological heterogeneity. The first line of treatment for BA is Kasai portoenterostomy (KPE), which temporarily saves most infants but as many as 40% will need liver transplantation (LTx) in the long run. Timing of KPE is important for outcome, with improved native liver survival in those operated before 60 days of age [5,6,7]. Even though the incidence of BA varies around the world from 1:5000 in Taiwan, to 1:10 000 in Japan, 1:14 000 in Sweden, and 1:20 000 in the United States [8,9,10,11], it is the most common reason for LTx in children [12, 13].
The etiology and pathogenesis of BA are not fully known. Several studies suggest that various viral infections could be of importance for the pathogenic mechanisms, for example cytomegalovirus (CMV), reovirus and rotavirus [12, 14,15,16,17,18]. A study from the UK showed that 10% of BA patients had CMV-IgM detected in serum and that this subgroup had a different histological appearance and a worse outcome [14], the latter was also seen in a Chinese study [19] and in a recently published meta-analysis including 784 patients [20]. A study from the group in the UK suggested that CMV-IgM positive BA patients could benefit from treatment with intravenous ganciclovir or oral valganciclovir [18]. A previous study from our center showed an incidence of 38% for ongoing CMV infection among Swedish infants with BA compared to 6% of age-matched controls, but no significant difference in the long-term outcome between CMV-positive and CMV-negative patients after portoenterostomy [15, 21]. In a recently published retrospective study, we compared data on incidence, impact and treatment of CMV infection in BA patients from ours and three other European centers. The novel findings of the present study are the in-depth data on our own expanded cohort, including details on the different effects of antiviral treatment [22].
Aim
It is of importance to know if CMV infection is associated with poorer outcome and thereby increased need for liver LTx and if that could be avoided with antiviral treatment (AVT). This retrospective study aimed to evaluate if there is still a high incidence of ongoing CMV infection in the Swedish BA population and to describe the treatment and outcome of these patients. We also wanted to know if the CMV-positive patients or their mothers are inherently different from the uninfected patients or their mothers which could be useful in future diagnostics.
Methods
Patient selection
This is a retrospective observational study including all 46 patients (26 males, 20 females) with BA who were diagnosed and treated at Karolinska University Hospital, Stockholm, Sweden in 2004–2020, this included the 37 patients born 2005–2018 who were described in a less detailed manner in the previous multicentre-based paper [22]. The last data were collected in November 2021, i.e., 1 year after KPE was performed in the youngest patient. Exclusion criteria were no KPE or unknown CMV status. Out of 52 patients, 6 were excluded, 4 females and 2 males. Five patients were excluded because they did not have KPE performed, and one patient was never tested for CMV. Four of the excluded patients had a primary LTx performed because of late diagnosis (one CMV positive and three CMV negative) and one patient had no surgery at all because of severe chromosomal abnormality with congenital anomalies including major heart malformations (CMV negative).
Outcome parameters
The primary outcome was 1-year survival with native liver. Other outcome parameters were clearance of jaundice and side effects from AVT. Clearance of jaundice was defined as total serum bilirubin < 20 µmol/L within 6 months after KPE. Side effects from AVT were defined as elevated creatinine, lowered hemoglobin concentration, lowered platelet or white blood cells count and elevated liver enzymes after KPE and AVT compared to before the treatment.
Compared parameters
The patients were divided into two groups according to CMV status and the groups were compared regarding birth weight, prematurity, splenomegaly, age at KPE and laboratory findings before KPE. Splenomegaly was defined by the written report from the ultrasonographist. The mothers of the patients were compared regarding age, parity, and country of birth, according to chart data.
Diagnosis, surgery, and medical treatment
The BA diagnosis was established by hepatobiliary scintigraphy with good uptake to the liver but no excretion to the gut within 24 h, needle biopsy with histological pattern suggesting extrahepatic biliary disorder and finally confirmed at laparotomy where intraoperative cholangiogram was performed, if possible.
KPE was performed by either or both of two individual pediatric surgeons, one of them (JFS) participated in 38 out of 46 operations.
All patients were given corticosteroids, fat-soluble vitamins, and ursodeoxycholic acid.
Cytomegalovirus infection
CMV status was defined during admission to the hospital for investigation of cholestasis or had already been established at the referring hospital. The patients were considered CMV positive if CMV-IgM was detected in serum and/or CMV-DNA was detected in urine or blood. The level of CMV replication in those considered to be CMV positive was analyzed by quantitative PCR detection for CMV-DNA in blood according to the current hospital routine. In patients born before 2016, CMV-DNA by PCR was analyzed in whole blood, thereafter it was analyzed in plasma. The CMV-DNA levels in these two compartments have previously been shown to be comparable [23].
Statistical analysis
Continuous data were expressed as medians and total range. The data could not be assumed to be normally distributed due to small sample size and was, therefore, compared using nonparametric Mann–Whitney U test. Categorical data were compared with cross tabulation and Chi-square test.
Ethics
The regional ethics review board in Stockholm has approved retrospective studies of medical records. Registration number 2017/1394-31.
Results
Cytomegalovirus infection
Fifteen (33%) out of forty-six patients were CMV positive in blood or urine at some point before surgery, 1 of them was negative at 2 days of age but positive 13 days after surgery and was treated with AVT and was, therefore, regarded as CMV positive for the purpose of this study. Two of the CMV-positive patients did not receive AVT, presumably because of very low CMV-DNA level in blood. Those patients are included in the CMV-positive group except when the results for AVT are reported.
None of the patients could be proven to have congenital CMV infection because all positive samples were taken after 3 weeks of age.
Out of the 15 patients defined as infected, CMV was detected by PCR in serum or urine in all 15. Twelve of these patients were also tested for CMV antibodies but only four (33%) were positive for CMV-IgM.
Survival with native liver and clearance of jaundice
The 1-year survival with native liver was 55% (n = 17) for CMV-negative patients and 47% (n = 7) for CMV-positive patients.
Clearance of jaundice within 6 months after KPE was 42% (n = 14) in the CMV-negative group and 27% (n = 4) in the CMV-positive group. This is shown in Table 1.
Maternal features
Out of 46 patients 26 had mothers who were born in Sweden, 3 in other parts of Europe, 9 in West Asia, Iran or Afghanistan, 7 in North or East Africa, and 1 in South America. A map of maternal origin is shown in Fig. 1.
World map showing maternal of origin of infants with biliary atresia included in the study. Produced with https://www.mapchart.net/
The mothers were all between 23 and 44 years of age when giving birth except for one who was 16 years. Parity was between 1 and 7 births (median 2).
Out of the 26 patients with a Swedish mother, 30% were CMV positive and out of the 20 patients whose mother was born outside of Sweden, 35% were CMV positive.
The median age for mothers in the CMV-negative group was 31 years and in the CMV-positive group 34 years (p = 0.08). There was no significant difference in the parity of the mothers in the two groups.
Prematurity and birth weight
Thirty-nine patients were born full term, seven patients were born in gestational week 33–36, i.e., late preterm. The prematurity rate was 16% for CMV-negative patients and 13% for CMV-positive patients. During 2004–2020, the average percentage for premature births was 6% in the whole Swedish population, according to Swedish Medical Birth Register [24].
Of the 39 patients with available data on both gestational age and birth weight, only 1 was small for gestational age and 2 were large for gestational age.
Splenomegaly
Splenomegaly was detected in 33% (n = 10) of the CMV-negative group and in 60% (n = 9) in the CMV-positive group (p = 0.09).
Laboratory findings in CMV-positive and CMV-negative patients
There was no significant difference between CMV-positive and CMV-negative patients regarding laboratory tests at the time of KPE: total bilirubin, conjugated bilirubin, AST, ALT, prothrombin time measured as international normalized ratio (INR), creatinine, hemoglobin, leukocyte count, thrombocyte count. These laboratory results are shown in Table 1.
Age at the time of surgery
The overall median age at the time of KPE was 71 days. It was 74 days (range 46–132) for CMV-positive and 68 days (range 32–130) for CMV-negative patients (p = 0.10). The median age at KPE was 70 days for patients with a Swedish mother and 74 days for patients with a non-Swedish mother (p = 0.42).
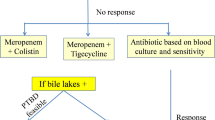
Antiviral treatment
Thirteen CMV-positive patients were given AVT at the discretion of the physician. There were some differences in treatment strategy regarding timing, duration, and dosage. Details about AVT are described in Table 2. The treatment was initiated before KPE in four patients and within 2–22 days after KPE in nine patients. The duration of AVT was 21–74 days (median 42 days); in one patient, it was prolonged because of LTx.
Six patients received only oral valganciclovir, four patients received only intravenous (IV) ganciclovir, and in three patients where treatment was initiated before KPE, they received first oral, then IV and then oral treatment again. The intravenous dosage varied between 5 and 11 mg/kg/d. Oral dosage varied between 10 and 40 mg/kg/day, one patient received as much as 58 mg/kg/day. Most patients had their dosage altered after one or a few weeks, either decreased or increased at the discretion of the physician but antiviral effect was seen before altered dosage in all patients. The highest reported trough levels varied between 0 and 4.7 µmol/L.
All treated patients had lowered CMV levels at the first testing after initiating AVT, as shown in Table 2. The timing of the test varied between 5 and 24 days after initiating AVT. CMV levels after completed treatment was 0 IU/mL or 0–500 IU/mL for all 12 patients where it was measured.
There were some improvements in liver specific laboratory findings for the 13 patients who received AVT when comparing before and after the surgery and AVT. There was no anemia, leukopenia, or elevated creatinine. Laboratory findings before and after AVT are shown in Table 3.
Nine out of ten CMV-positive patients who subsequently, at some point before November 2021, underwent LTx had CMV reactivation within1 year after transplantation. Six of these were successfully treated with AVT during 1–2.5 months. Three patients were treated two or three times for reactivation during the first year after transplantation. One of the two patients who was CMV positive but did not receive AVT at the time of KPE was liver transplanted about 1 year after KPE and had reactivated CMV infection 6 weeks after LTx. The reactivation started shortly after treatment for transplant rejection and was successfully treated with oral valganciclovir for 4 weeks.
Corticosteroids
All 46 patients in the present study were treated with prednisolone after KPE, starting 7 days after surgery. There was no difference in dosage or duration of the prednisolone treatment between CMV-positive and CMV-negative patients. The target-dose and the median-dose prednisolone both were 2 mg/kg for 14 days followed by 1 mg/kg for 7 days. The dose and the duration of corticosteroid treatment varied slightly between patients at the discretion of the physician.
Discussion
This study confirms that the incidence of ongoing CMV infection in Swedish patients with BA remains around 30%. This is true regardless of whether the mother is born in Sweden or not. The cause of the different incidence compared to the study from the UK [14] is not known; however, in the latter study, only CMV-IgM positivity was used to define infected patients. For comparison, studies from China, Brazil, South Africa, USA, India, and Norway show an incidence of 24–78% for CMV in patients with BA [17, 25,26,27,28,29,30].
It is not established to what degree CMV influences the development of BA and the outcome after KPE and whether the infection should be treated with antiviral drugs. However, in a retrospective report from the UK, AVT significantly improved outcome for CMV-positive patients when compared to untreated [18]. In accordance with that, we found in our study that CMV infection effectively could be treated with AVT regarding the viremia level and that this coincided with biochemical improvement. However, no untreated CMV-positive control was available. In the study from the UK, most of the CMV-positive patients were not treated with steroids which may explain why those patients had better outcomes both regarding clearance of jaundice within 6 months (75%) and 1-year survival with native liver (75%). Quite importantly, the patients in the UK had KPE performed around 10 days earlier than the patients in our study which may clearly contribute to the better overall outcome.
CMV testing in all patients with neonatal cholestasis is of possible importance. However, its detection clearly does not rule out a BA diagnosis. The only finding in our CMV-positive BA patients that differed from the CMV-negative patients during the investigation of cholestasis was a trend toward a higher incidence of splenomegaly. In other aspects, the two groups were similar, i.e., no difference in gestational week, birth weight or laboratory findings; hence, it is important to test all BA patients to find the CMV-positive ones. However, screening for CMV in all newborns would not be of benefit for the BA patients because these patients seem to seldom have congenital CMV infection [31].
There were no obvious differences between the mothers of CMV-positive and CMV-negative patients. Neither country of origin, number of siblings nor the mothers’ age did differ significantly. Therefore, for example, overcrowding or multiparity could not be confirmed as risk factors for CMV infection in this cohort. The incidence of prematurity in our whole BA cohort is higher than in the rest of the Swedish population. This is consistent with studies from Taiwan and the Netherlands where the incidence of BA was higher in preterm infants than in term infants [32, 33]. However, the prematurity rate did not differ when comparing CMV-positive and CMV-negative patients.
The limitation of this study is the small sample size and because, it is a retrospective study, there is heterogeneity in, for example, type of AVT. On the other hand, while several centers have reported the use of AVT in patients with biliary atresia and ongoing CMV infection [34], data on dosage, safety, and effect, as ours, are very scarcely found. Overall, the AVT used in this setting seemed safe. Data are lacking regarding the optimal trough levels to avoid side effects. In our center, we have used an empirically suggested level from experiences in children after solid organ transplantation. We found that if the trough levels were kept below 4 µmol/L, there were no negative effects from AVT such as bone marrow depression or impaired kidney function. Even though 9 out of the 13 highest ganciclovir trough levels in this cohort were below 2 µmol/L, the AVT was effective in reducing viremia. After LTx, the virus will commonly be reactivated at some point. We could not find that AVT after KPE was associated with difficult-to-treat CMV reactivation post LTx.
This study did not aim for and had no possibility to explain why there might be a difference in outcome for BA patients with CMV infection than for those without. If indeed CMV-positive patients had been older at KPE, this could have indicated that the onset of the CMV-associated BA starts later in life, suggesting this subgroup to be a different entity. Alternatively, later diagnosis could be due to late referral as pointed out previously [27].
Conclusion
Ongoing CMV infection is common in BA patients and the viremia can effectively be treated without any major side effects. We would, therefore, suggest that a positive effect of AVT on outcome might still be postulated but that further studies in randomized multicenter settings are needed to clarify the possible effect of the treatment on clinical outcome.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Davenport M, Kerkar N, Mieli-Vergani G, Mowat AP, Howard ER (1997) Biliary atresia: the King’s College Hospital Experience (1974–1995). J Pediatr Surg 32:479–485. https://doi.org/10.1016/S0022-3468(97)90611-4
Nio M, Sano N, Ishii T, Sasaki H, Hayashi Y, Ohi R (2006) Long-term outcome in type I biliary atresia. J Pediatr Surg 41:1973–1975. https://doi.org/10.1016/j.jpedsurg.2006.08.019
Chardot C, Buet C, Serinet M-O, Golmard J-L, Lachaux A, Roquelaure B et al (2013) Improving outcomes of biliary atresia: French national series 1986–2009. J Hepatol 58:1209–1217. https://doi.org/10.1016/j.jhep.2013.01.040
Nio M, Ohi R, Miyano T, Saeki M, Shiraki K, Tanaka K (2003) Five- and 10-year survival rates after surgery for biliary atresia: a report from the Japanese biliary atresia registry. J Pediatr Surg 38:997–1000. https://doi.org/10.1016/S0022-3468(03)00178-7
Ohi R (2001) Surgery for biliary atresia: surgery for biliary atresia. Liver 21:175–182. https://doi.org/10.1034/j.1600-0676.2001.021003175.x
Chen S-M (2006) Screening for biliary atresia by infant stool color card in Taiwan. Pediatrics 117:1147–1154. https://doi.org/10.1542/peds.2005-1267
Song Z, Dong R, Shen Z, Chen G, Yang Y, Zheng S (2017) Surgical outcome and etiologic heterogeneity of infants with biliary atresia who received Kasai operation less than 60 days after birth: a retrospective study. Medicine (Baltimore) 96:e7267. https://doi.org/10.1097/MD.0000000000007267
Tiao M-M, Tsai S-S, Kuo H-W, Chen C-L, Yang C-Y (2007) Epidemiological features of biliary atresia in Taiwan, a national study 1996–2003. J Gastroenterol Hepatol. https://doi.org/10.1111/j.1440-1746.2007.05114.x
Wada H, Muraji T, Yokoi A, Okamoto T, Sato S, Takamizawa S et al (2007) Insignificant seasonal and geographical variation in incidence of biliary atresia in Japan: a regional survey of over 20 years. J Pediatr Surg 42:2090–2092. https://doi.org/10.1016/j.jpedsurg.2007.08.035
Fischler B, Haglund B, Hjern A (2002) A population-based study on the incidence and possible pre- and perinatal etiologic risk factors of biliary atresia. J Pediatr 141:217–222. https://doi.org/10.1067/mpd.2002.126001
Hopkins PC, Yazigi N, Nylund CM (2017) Incidence of biliary atresia and timing of hepatoportoenterostomy in the United States. J Pediatr 187:253–257. https://doi.org/10.1016/j.jpeds.2017.05.006
Perlmutter DH, Shepherd RW (2002) Extrahepatic biliary atresia: A disease or a phenotype? Extrahepatic biliary atresia: a disease or a phenotype? Hepatology 35:1297–1304. https://doi.org/10.1053/jhep.2002.34170
McDiarmid SV, Anand R, Lindblad AS, The SPLIT Research Group (2004) Studies of pediatric liver transplantation: 2002 update. An overview of demographics, indications, timing, and immunosuppressive practices in pediatric liver transplantation in the United States and Canada. Pediatr Transplant 8:284–294. https://doi.org/10.1111/j.1399-3046.2004.00153.x
Zani A, Quaglia A, Hadzić N, Zuckerman M, Davenport M (2015) Cytomegalovirus-associated biliary atresia: an aetiological and prognostic subgroup. J Pediatr Surg 50:1739–1745. https://doi.org/10.1016/j.jpedsurg.2015.03.001
Fischler B, Ehrnst A, Forsgren M, Örvell C, Nemeth A (1998) The Viral Association of neonatal cholestasis in Sweden: a possible link between cytomegalovirus infection and extrahepatic biliary atresia. J Pediatr Gastroenterol Nutr 27:57–64. https://doi.org/10.1097/00005176-199807000-00010
Fischler B, Woxenius S, Nemeth A, Papadogiannakis N (2005) Immunoglobulin deposits in liver tissue from infants with biliary atresia and the correlation to cytomegalovirus infection. J Pediatr Surg 40:541–546. https://doi.org/10.1016/j.jpedsurg.2004.11.035
Xu Y, Yu J, Zhang R, Yin Y, Ye J, Tan L et al (2012) The perinatal infection of cytomegalovirus is an important etiology for biliary atresia in China. Clin Pediatr (Phila) 51:109–113. https://doi.org/10.1177/0009922811406264
Parolini F, Hadzic N, Davenport M (2019) Adjuvant therapy of cytomegalovirus IgM + ve associated biliary atresia: prima facie evidence of effect. J Pediatr Surg 54:1941–1945. https://doi.org/10.1016/j.jpedsurg.2018.12.014
Shen C, Zheng S, Wang W, Xiao X-M (2008) Relationship between prognosis of biliary atresia and infection of cytomegalovirus. World J Pediatr 4:123–126. https://doi.org/10.1007/s12519-008-0024-8
Zhao Y, Xu X, Liu G, Yang F, Zhan J (2021) Prognosis of biliary atresia associated with cytomegalovirus: a meta-analysis. Front Pediatr 9:710450. https://doi.org/10.3389/fped.2021.710450
Fischler B, Svensson JF, Nemeth A (2009) Early cytomegalovirus infection and the long-term outcome of biliary atresia. Acta Paediatr 98:1600–1602. https://doi.org/10.1111/j.1651-2227.2009.01416.x
Fischler B, Czubkowski P, Dezsofi A, Liliemark U, Socha P, Sokol RJ et al (2022) Incidence, impact and treatment of ongoing CMV infection in patients with biliary atresia in four European centres. J Clin Med 11:945. https://doi.org/10.3390/jcm11040945
Kullberg-Lindh C, Olofsson S, Brune M, Lindh M (2008) Comparison of serum and whole blood levels of cytomegalovirus and Epstein-Barr virus DNA. Transpl Infect Dis 10:308–315. https://doi.org/10.1111/j.1399-3062.2008.00313.x
Swedish Medical Birth Register [database online]. Socialstyrelsen n.d. https://www.socialstyrelsen.se/statistik-och-data/register/alla-register/medicinska-fodelseregistret/. Accessed 7 Jan 2021
De Tommaso AM, Andrade PD, Costa SC, Escanhoela CA, Hessel G (2005) High frequency of human cytomegalovirus DNA in the liver of infants with extrahepatic neonatal cholestasis. BMC Infect Dis 5:108. https://doi.org/10.1186/1471-2334-5-108
Moore SW, Zabiegaj-Zwick C, Nel E (2012) Problems related to CMV infection and biliary atresia. S Afr Med J 102:890. https://doi.org/10.7196/SAMJ.6163
Tarr PI, Haas JE, Christie DL (1996) Biliary atresia, cytomegalovirus, and age at referral. Pediatrics 97:828–831
Fjaer RB, Bruu A-L, Nordbø SA (2005) Extrahepatic bile duct atresia and viral involvement. Pediatr Transplant 9:68–73. https://doi.org/10.1111/j.1399-3046.2005.00257.x
Zhao D, Gong X, Li Y, Sun X, Chen Y, Deng Z et al (2021) Effects of cytomegalovirus infection on the differential diagnosis between biliary atresia and intrahepatic cholestasis in a Chinese large cohort study. Ann Hepatol 23:100286. https://doi.org/10.1016/j.aohep.2020.100286
Goel A, Chaudhari S, Sutar J, Bhonde G, Bhatnagar S, Patel V et al (2018) Detection of cytomegalovirus in liver tissue by polymerase chain reaction in infants with neonatal cholestasis. Pediatr Infect Dis J 37:632–636. https://doi.org/10.1097/INF.0000000000001889
Fischler B, Rodensjo P, Nemeth A, Forsgren M, Lewensohn-Fuchs I (1999) Cytomegalovirus DNA detection on Guthrie cards in patients with neonatal cholestasis. Arch Dis Child - Fetal Neonatal Ed 80:F130–F134. https://doi.org/10.1136/fn.80.2.F130
Chiu C-Y, Chen P-H, Chan C-F, Chang M-H, Wu T-C (2013) Biliary atresia in preterm infants in Taiwan: a nationwide survey. J Pediatr 163:100-103.e1. https://doi.org/10.1016/j.jpeds.2012.12.085
van Wessel DBE, Boere T, Hulzebos CV, de Kleine RHJ, Verkade HJ, Hulscher JBF (2017) Preterm infants with biliary atresia: a nationwide cohort analysis from The Netherlands. J Pediatr Gastroenterol Nutr 65:370–374. https://doi.org/10.1097/MPG.0000000000001692
Wong Z, Davenport M (2019) What happens after Kasai for biliary atresia? A European multicenter survey. Eur J Pediatr Surg 29:001–006. https://doi.org/10.1055/s-0038-1668146
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by UL. The first draft of the manuscript was written by UL and all authors contributed to previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liliemark, U., Svensson, J.F. & Fischler, B. Incidence and antiviral treatment of cytomegalovirus infection in infants with biliary atresia. Pediatr Surg Int 39, 117 (2023). https://doi.org/10.1007/s00383-023-05394-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05394-1