Abstract
Purpose
The efficacy of robot-assisted hepaticojejunostomy (RAHJ) and laparoscopic-assisted hepaticojejunostomy (LAHJ) in children with congenital choledochal dilatation has been a topic of much debate and controversy. The purpose of this study was to evaluate the role of RAHJ and LAHJ in pediatric congenital choledochal dilatation.
Method
The review program has been prospectively registered (PROSPEROID: CRD42022306868). We searched the PubMed, Embase, Cochrane, CBM, VIP, Web of Science, CNKI databases, and Wanfang databases from March 2021. The Mantel–Haenszel method and a random-effects model were used to figure out the hazard ratio (95% CI).
Results
Ten studies evaluated eight hundred and sixty-nine subjects (three hundred and thirty-two in the robotic group and five hundred and thirty-seven in the laparoscopic group), meeting all inclusion criteria. Compared with the laparoscopic group, robotic group demonstrated fewer postoperative complications [p = 0.0009; OR = 0.34 (95% CI, 0.18–0.64); I2 = 3%], shorter postoperative hospital stay [p < 00,001; MD = − 2.05 (95% CI, − 2.40–1.70); I2 = 0%], and less intraoperative bleeding [p = 0.008; MD = − 10.80 (95% CI, − 18.80–2.81); I2 = 99%]. There was no significant difference in operative time between the two groups [p = 0.10; MD = 24.53 (95% CI, − 5.11–54.17); I2 = 99%]. The same situation happened in short-term complication outcomes [p = 0.06; RR = 0.45 (95% CI, 0.19–1.04); I2 = 0%]. However, children in the RAHJ group had significantly lower levels of long-term complications [p = 0.04; OR = 0.41 (95% CI, 0.17–0.96); I2 = 0%]. Hospitalization costs were significantly higher in the RAHJ group [p < 0.00001; OR = 27,113.86 (95% CI, 26,307.24–27,920.48); I2 = 0%]. For overall complications, subgroup analysis of literature published after 2020 and of literature with high quality scores showed a significant decrease in the RAHJ group.
Conclusion
In children with congenital choledochal dilatation, RAHJ is associated with reduced intraoperative bleeding, postoperative complications, and length of stay. Robotic surgery has a bright future in the treatment of pediatric common hepatic duct cysts and deserves to be promoted and popularized.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital choledochal dilatation is a congenital malformation involving both local dilatation of the extrahepatic bile duct, including the common bile duct, and pancreaticobiliary maljunction. However, cases associated with intrahepatic bile duct dilatation can be included in this entity [1]. Congenital choledochal dilatation are uncommon congenital anomalies of bile ducts with an incidence of 1 in 100,000–150,000 live births in the western population [2,3,4], but reported to be as high as 1 in 13,500 live births in the United States and 1 in 15,000 in Australia [5]. The incidence is higher in Asian population with an incidence of 1 in 1000 [6], of which about two-third cases are reported from Japan [7]. Holistic examination of the data regarding robotic congenital choledochal dilatation excision in children makes it clear that more research is needed to examine the utility of this approach. The most recent and larger studies do show acceptable complication rates, and robotic congenital choledochal dilatation excision does not appear inferior with regard to complications if performed by experienced surgeons. On the other hand, concerns regarding the long operative times may be reinforced if forthcoming data show similar trends; additionally, cost-effective information should be reported given known expense of robotic platforms [8].
The current investigation is an updated meta-analysis of postoperative complications and postoperative length of stay for RAHJ and LAHJ for pediatric congenital choledochal dilatation. More specifically, a systematic evaluation and meta-analysis was performed to determine the impact of RAHJ and LAHJ on postoperative complications and postoperative length of stay.
Materials and methods
Search strategy
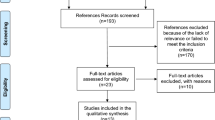
The review protocol was prospectively registered (PROSPEROID: CRD42022306868). A systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [9]. The search was conducted in the major electronic databases of PubMed, Embase, Cochrane, CBM, VIP, Web of Science, CNKI databases, and Wanfang databases.
Giving an example, we search terms such as choledochal cyst, robotic surgery, and literature types, as well as all related MeSH terms. The keyword of the search was recorded in the appendix section.
When several studies reported findings for the same patients, the most recent or most complete study was chosen.
Inclusion criteria
Studies were included according to the following criteria. Case inclusion criteria: (1) congenital choledochal dilatation diagnosed by magnetic resonance cholangiopancreatography; (2) children undergoing da Vinci robotic surgery or conventional laparoscopic surgery (including intraoperative conversion to open surgery); (3) surgery time, intraoperative bleeding, postoperative complications, and hospital stay were recorded.
We excluded articles that included in the study those who presented with choledochal cyst-related acute abdomen necessitating emergency surgery. Studies were excluded if the type of article was a case report or a review. A small number of studies were conference literature, where the original article could not be found, and were also excluded. (Fig. 1).
Definitions
In this post, we focus on patients who underwent RAHJ and LAHJ. “RAHJ” stands for robot-assisted hepatic tunnel-jejunostomy and “LAHJ” stands for laparoscopic hepatic tunnel-jejunostomy.
Data extraction
We reviewed all titles and abstracts to determine eligibility and retrieve articles. The following information was extracted according to a fixed protocol: study design, geographical location, stage, sample size, group number, and number of complications (Table 1).
Validity assessment
The quality of included studies was accessed independently by the Newcastle–Ottawa Quality Assessment Scale. The scale comprises three factors: patient selection, comparability of the study groups, and assessment of outcome. A score of 1 was awarded for each item if the standard was completely met, a score of 0.5 was awarded if the standard was partially met, and a score of 0 was awarded if it was not met or if it was unclear whether it was met. The total score for each study was then calculated, a score of > 6 indicated a high-quality study, a score of ≥ 3 and ≤ 6 indicated a median-quality study, while a score of ≥ 0 and ≤ 2 indicated a low-quality study [10].
None of the ten included studies stated that operational selection was randomized (selection bias). The type of topic of our study dictates that confidentiality of participants and personnel is not possible (performance bias). The same happens with the confidentiality of the assessment of the results (test bias). After careful assessment of reports of Koga et al. [11], Cai et al. [12], Xie et al. [13], a brief description of follow-up durations could not be observed, and it was rated as unclear of bias. In reports of Cai et al. [14], Xiao et al. [15], some postoperative complications were not introduced clearly, and it was also rated as unclear of bias (attrition bias). These cases are summarized in Fig. 2.
Statistical analysis
Statistical analysis was conducted by Review Manager version 5.4. The significance of pooled OR/MD was assessed by Z test, and a P value < 0.05 was considered significant. Statistical heterogeneity between studies was assessed by I2 and Q statistics. The I2 statistic was used to test for heterogeneity. More than 50% of I2 was considered to be highly heterogeneous and the results were aggregated using random-effects models. However, I2 < 50% is considered to be low heterogeneous, so fixed-effect models can be used, and subgroup analysis was used to explore potential causes of heterogeneity [16].To assess the risk of publication bias, funnel plots were used to assess publication bias [17]. P values < 0.05 were considered significant for heterogeneity.
Results
Ten studies evaluated eight hundred and sixty-nine subjects (five hundred and thirty-seven in the laparoscopic group and three hundred and thirty-two in the robotic group). Sample sizes ranged from 2 to 172 (Table 1). The literatures were published in 2019 or later. Validity scores could be obtained in Table 2. Six articles were of high quality, four articles were of moderate quality, and low-quality articles were not being continued research. Xie et al. [13, 18] additionally documented surgical conditions, complications, and postoperative length of stay in open surgery patients.
Results of the meta-analysis
Robotic surgery showed a trend toward reduced intraoperative bleeding and shorter postoperative hospital stay. There was no obvious distinction in operative time between the two groups. Robotic surgery group significantly improved the postoperative complication profile of patients. Children in the RAHJ group had significantly lower levels of long-term complications. However, short-term complication outcomes did not change obviously. RAHJ group was proved to be more expensive, as expected. For overall complications, subgroup analysis of literature published after 2020 and of literature with high quality scores showed a significant decrease in the RAHJ group.
Intraoperative bleeding
Six studies provided data including seven hundred and eighty-one patients with congenital choledochal dilatation (two hundred and ninety-five in the RAHJ group and four hundred and eighty-six in the LAHJ group). Heterogeneity between studies was also significant (I2 = 99%, P < 0.00001). Therefore, a random-effects model was applied. Of the six studies included in the review, five studies reported less intraoperative bleeding in the RAHJ group. There was less intraoperative bleeding in the RAHJ group [(p = 0.008; MD = − 10.80 (95% CI, − 18.80–2.81); I2 = 99%] (Fig. 3).
Time to surgery
Eight studies [12, 13, 18,19,20,21,22,23] provided data including eight hundred and sixty-two patients with congenital choledochal dilatation (three hundred and thirty in the RAHJ group and five hundred and thirty-two in the LAHJ group). Heterogeneity between studies was significant [I2 = 99%, P < 0.00001], and a random-effects model was subsequently applied. Of the included articles reviewed, five studies by Cai et al. [12], Chi et al. [19, 23], Dong et al. [20], and Lin et al. [22] reported less operative time in the LAHJ group. However, no obvious distinction happened on this indicators [p = 0.10; MD = 24.53 (95% CI, − 5.11–54.17); I2 = 99%] (Fig. 4).
Postoperative hospital stay
In the current meta-analysis, a total of 457 cases were included in the 4 studies to study the issue of postoperative length of stay, and after sensitivity analysis, the article by Chi et al. was finally removed. A total of 3 articles were finally included, including 131 cases in the RAHJ group and 186 cases in the LAHJ group. All of which showed a significantly lower postoperative length of stay in the RAHJ group compared to the LAHJ group [I2 = 0%, P = 0.55]. RAHJ group was able to significantly reduce the postoperative hospital stay [p < 0.00001; MD = − 2.05 (95% CI, -2.40–1.70); I2 = 0%] (Fig. 5).
Postoperative complications
Total complications
A total of 818 cases were included in the final 9 papers, 308 in the RAHJ group and 510 in the LAHJ group [I2 = 3%, P = 0.40]. RAHJ was associated with a reduction in complications, possibly because of the reduced bleeding and operative time in the surgery [p = 0.0009; MD = 0.34 (95% CI, 0.18–0.64); I2 = 3%] (Fig. 6).
Short-term complications
Short-term complications were defined as those that occurred within 30 days after surgery. Short-term complications were documented in 8 of the 10 publications, with a cumulative total of 862 cases included (330 in the RAHJ group and 532 in the LAHJ group). The overall heterogeneity was low [I2 = 0%, P = 0.58]. The two surgical procedures did not produce obvious changes in this metric [p = 0.06; RR = 0.45 (95% CI, 0.19–1.04); I2 = 0%] (Fig. 7).
Long-term complications
Long-term complications were defined as those that occurred more than 30 days after surgery. Long-term complications were documented in 5 of the 10 publications, with a cumulative total of 678 cases included (274 in the RAHJ group and 404 in the LAHJ group). The overall heterogeneity was low [I2 = 0%, P = 0.95]. RAHJ group had significantly lower levels of long-term complications [p = 0.04; OR = 0.41 (95% CI, 0.17–0.96); I2 = 0%] (Fig. 8).
Hospitalization costs
The cost of robotic surgery is undoubtedly higher than that of laparoscopic surgery. To discuss the difference in the total cost of the two treatment modalities when accounting for postoperative hospitalization costs, a further analysis was performed. Among them, the cost data recorded in the Cai et al. [12] article were recorded with interquartile spacing and were skewed [RAHJ: 11,250 (10,950 ~ 12,900) $, LAHJ: 4800 (4050 ~ 5400) $], so they are only statistically described here and not included in the combined analysis. The overall heterogeneity was low [I2 = 0%, P = 0.63]. As expected, RAHJ group showed an expensive price [p < 0.00001; OR = 27,113.86 (95% CI, 26,307.24–27,920.48); I2 = 0%] (Fig. 9).
Subgroup analysis
We performed subgroup analysis of total complications, short-term complications, and long-term complications of cases according to the year of publication (< 2020, > 2020) and quality score (high or medium; Table 3). Of the literature reporting long-term complications, the number of publications before 2020 was only one and could not be included in the combined analysis. There were no significant differences in levels in each subgroup, whether for long-term or short-term complications. For overall complications, subgroup analysis of literature published after 2020 and of literature with high quality scores showed a significant decrease in the RAHJ group, while subgroup analysis of literature published before 2020 and of literature with moderate quality scores showed no obvious distinction (Fig. 10).
Publication bias
In the funnel plots comparing postoperative complications (Supplementary Fig. 1), postoperative length of stay (Supplementary Fig. 2), intraoperative bleeding (Supplementary Fig. 3), and operative time (Supplementary Fig. 4) between the RAHJ and LAHJ groups, studies grouped at the top of the plot suggest that larger studies with larger numbers of patients are more likely to be included. The lack of studies at the bottom of the graph suggests that publications with smaller sample sizes are rare.
Discussion
Robotic surgical system has been utilized in the treatment of choledochal cysts since 2006. Its advantages include three-dimensional visualization through a stereo endoscope, tremor reduction, motion scaling, and the additional degrees of freedom compared to the standard laparoscopic instruments. However, at present, it is not widely accepted yet because of the size of current robotic hardware in relation to child’s body size, the loss of hepatic feedback, special training requirement, and expensive hardware and maintenance of the robotic system. With the technical improvement, the refined robotic system will provide an optimal alternative to achieve the advanced goal of minimal invasive surgery, scarlessness, minimal surgical trauma, and steep learning curve [24]. More recent studies have shown improved outcomes compared to the early era of robotic choledochal dilatation excision [8]. The purpose of this study was to evaluate the role of robot-assisted and laparoscopic-assisted surgery in the management of children with congenital choledochal dilatation.
Intraoperative bleeding, time to surgery, and postoperative hospital stay
The meta-analysis by Yin et al. in terms of intraoperative bleeding included 4 studies including 391 patients with choledochal dilatation (145 in the RAHJ group and 246 in the LAHJ group), where overall there was no significant difference in intraoperative bleeding between the RAHJ and LAHJ groups, subgroup analysis showed no significant difference between the two groups in pediatric patients, while adult patients showed lower bleeding [25]. Compared to the meta-analysis by Yin et al., this paper focuses on pediatric patients themselves rather than all age groups, includes a newer and more complete literature, and draws conclusions with improved reliability.
In Koga’s report, the mean operative times in the two groups were 618 and 654 min, significantly longer than in the other seven groups. Similar to the meta-analysis on intraoperative bleeding, the heterogeneity of this part of the meta-analysis was very high. The clinical value of the conclusions drawn from it was low. The meta-analysis by Yin et al. in terms of surgery time included 6 studies including 484 patients with choledochal dilatation (177 in the RAHJ group and 307 in the LAHJ group), where overall there was no significant difference in surgery time between the RAHJ and LAHJ groups, subgroup analysis showed no significant difference between the 2 groups in pediatric patients, while adult patients showed significant shorter operative time [25]. This is consistent with the conclusion reached in this paper.
It is worth noting that patients' postoperative medications differed in different studies, which to some extent affects the accuracy of the conclusions on postoperative length of stay. The meta-analysis by Yin et al. on length of stay included 6 studies including 484 patients with biliary dilatation (177 in the RAHJ group and 307 in the LAHJ group), in which overall there was no significant difference in length of stay between the RAHJ and LAHJ groups, and subgroup analysis showed no significant differences between the 2 groups in pediatric and adult patients [25]. This is inconsistent with the conclusion reached in this paper. This may be related to the small number of pediatric patient cases included in this literature.
Postoperative complications
Total complications
In the present analysis, ten reports described intraoperative and postoperative complications. Unexpectedly, Cai et al. [12, 14], Dong et al. [20], Xiao et al. [15], Xie et al. [13, 18], Chi et al. [19], Kim et al. [26], and Lin et al. [22] reported that complications were not related to the extent of resection. After sensitivity analysis, the article by lin et al. was excluded.
Short-term complications
A total of 6 (1.8%) patients in the RAHJ group were identified as having short-term complications, compared to a total of 30 (5.6%) in the LAHJ group. In the report by Cai et al. [12], there were one case of umbilical incision infection with abscess formation and one case of postoperative intra-abdominal bleeding in the RAHJ group with one case of bile leakage in the LAHJ group. In the report by Chi et al. [19], no short-term complications happened in the RAHJ group. Meanwhile, one child had anastomotic bleeding, one child had wound infection, two kids had bile leakage in the LAHJ group. In the report by Dong et al. [20], one kid who underwent RAHJ had pneumoperitoneum and number of the same indicator is three in the LAHJ group. Apart from this, there is one kid with incision infection and one kid with pancreatic fistula separately in the LAHJ group. In the report by Koga et al. [11], there were no short-term complications in the RAHJ group and anastomotic leakage complicated one LAHJ case. In the report by Lin et al. [22], there was one child who had upper respiratory infection in the RAHJ group. In the LAHJ group, one child had anastomotic bleeding accompanied by bile leakage. Three children had upper respiratory infection. Three children had wound infection. In the report by Chi et al. [23], there were two anastomotic bleeding cases, one wound infection case, and two bile leakage cases in LAHJ group while the number of cases in RAHJ group was zero. In the report by Xie et al. [18], one child with anastomotic bleeding received RAHJ while one child with anastomotic bleeding and two children with bile leakage received LAHJ. In the report by Xie et al. [13], there were one child with gallbladder bleeding in the RAHJ group and one child with gallbladder bleeding, two children with bile leakage in the LAHJ group.
The most common short-term complication in the RAHJ group was anastomotic bleeding (n = 3, 50.0%), and the most common complication in the LAHJ group was wound infection (n = 8, 26.7%). In addition, four patients in the RAHJ group had umbilical incision infection with abscess (n = 1, 16.7%), intra-abdominal bleeding (n = 1, 16.7%), upper respiratory tract infection (n = 1, 16.7%), and peritoneal effusion (n = 1, 16.7%). Twenty-two patients in the LAHJ group had biliary fistula (n = 11, 36.7%), anastomotic bleeding (n = 6, 20.0%), peritoneal effusion (n = 1, 3.3%), pancreatic fistula (n = 1, 3.3%), anastomotic fistula (n = 1, 3.3%), and upper respiratory tract infection (n = 3, 10.0%). In the report by Yin et al. [25], no significant differences in short-term complications were shown between RAHJ-treated and LAHJ-treated patients. The results of the subgroup analysis remained the same for the pediatric group as well as the adult group.
Long-term complications
A total of 7 (2.6%) patients in the RAHJ group were identified as having short-term complications, compared to a total of 25 (6.2%) in the LAHJ group. In the report by Chi et al. [19], one child had cholangitis in the RAHJ group and the number of hepaticojejunostomy stricture, residual cyst, distal lithiasis was one separately in the LAHJ group. The median values of the follow-up time in the RAHJ group and the LAHJ group were 24 and 31.5 months. In the report by Lin et al. [22], one child developed stenosis of hepatoenteric anastomosis and two children developed cholangitis in LAHJ group while there were no long-term complications cases in the RAHJ group. In the RAHJ group, the average following time was 13.38 ± 2.02 months. In the LAHJ group, the average following time was 14.04 ± 3.18 months. In the report by Chi et al. [23], there were one child with stenosis of hepatoenteric anastomosis, two children with cholangitis, and one child with distal lithiasis in the RAHJ group. Meanwhile, two children had stenosis of hepatoenteric anastomosis, one child developed cholangitis, one child developed residual cyst, and three children developed distal lithiasis in the LAHJ group. The median values of the follow-up time in the RAHJ group and the LAHJ group were 34 and 36 months. In the report by Xie et al. [18], one child developed intestinal obstruction in the RAHJ group. In the LAHJ group, there were one child with intestinal obstruction, one child with biliary stones, one child with residual cyst, and three children with stricture of hepaticojejunostomy. The median follow-up time in the RAHJ group and the LAHJ group were, respectively, 20 months and 36 months. In the report by Xie et al. [13], there was one child with intestinal obstruction in the RAHJ group. However, there were three children with stricture of hepaticojejunostomy, one child with intestinal obstruction, one child with biliary stones, and one child with residual cyst in the LAHJ group. The follow-up time was not mentioned.
The most common complication in the RAHJ group was cholangitis (n = 3, 42.9%), and the most common complication in the LAHJ group was anastomotic stricture (n = 10, 40.0%). Other long-term complications in the RAHJ group included anastomotic strictures (n = 1, 14.3%), distal stones (n = 1, 14.3%), and intestinal obstruction (n = 2, 28.6%). Other long-term complications in the LAHJ group included residual abscesses (n = 4, 16.0%), distal stones (n = 4, 16.0%), cholangitis (n = 3, 12.0%), gallstones (n = 2, 8.0%), and intestinal obstruction (n = 2, 8.0%).In the report by Yin et al. [25], there was no significant difference in the long term between the RAHJ and LAHJ groups in terms of the level of complications, and the same was true for the results of the pediatric and adult groups in the subgroup analysis.
Secondary surgery and hospitalization costs and follow-up time
Among the ten publications, only the report of Xie et al. [18] clearly documented the secondary surgery, one case in the RAHJ group and five cases in the LAHJ group. In RAHJ group, one patient with bleeding at the hepaticojejunostomy received a reoperation with laparotomy. In LAHJ group, one patient with bleeding at the hepaticojejunostomy received an exploratory laparotomy, one patient with biliary stone received choledochojejunostomy and lithotomy, three patients with stricture of the hepaticojejunostomy received a reoperation of choledochojejunostomy.
The analysis result of hospitalization costs is also in line with expectations. However, only two Chinese studies were included in this price comparison. Koga et al. [11] reported that the Japanese national health insurance system does not cover the use of robotic surgery, resulting in an average procedure cost of approximately $15,000. There are few statistical studies related to congenital choledochal dilatation abroad, and the cost issue lacks supporting literature. Therefore, the conclusions are limited for foreign children.
Seven articles mentioned the issue of follow-up time. Among them, the mean of the follow-up time exceeded 24 months in both the RAHJ and LAHJ groups as reported by S. Q. Chi et al. [23], Chi et al. [19], and Lin et al. [22].
Subgroup analysis
We believe the outcome is due to the increasing popularity of the surgical da Vinci robot over time, as well as the increasing experience and proficiency of robotic surgical operators through continuous practice and training, which undoubtedly contributes to the improvement of robotic surgical outcomes. At the same time, articles with high quality scores imply less bias and higher reliability of the conclusions drawn. The relevant information is summarized in Fig. 10.
Limitations
This meta-analysis has some limitations. First, a more precise analysis would have been possible if data from individual patients had been available and could have been adjusted for age, sex, race, and geographic location. Second, the included literature does not meticulously describe the patient's preoperative infection and preoperative bile drainage. Third, different study sites use different perioperative therapeutic agents for patients; there is no uniformity in the evaluation of surgical tolerance, and biological heterogeneity affects clinical outcomes. Fourth, congenital choledochal dilation has a distinct presentation in the Eastern population yet shares some commonality with Western patients. However, some reported differences in presentation, malignancy risk, and patient demographics between Western and Eastern populations should spur further investigation into congenital choledochal dilation in Western patients to understand this disease and tailor management guidelines to Western populations [27]. Most of the literature data included in this meta-analysis were from Asian countries, and their reference value for children with choledochal cysts in Western countries is questionable. Lastly, the annual surgical volume of units published in the literature also influenced the results of our subgroup analysis. If the annual surgical volumes of the corresponding hospitals included in the study were comparable, it would be easier to compare the advantages and disadvantages of the two surgical approaches in different years.
Prospect
The advantages of robotic surgery include the following: (1) robotic surgery has more technical advantages [28], including three-dimensional imaging, tremor filters, and articulated instruments [29], three-dimensional vision can be magnified 10–15 times; (2) greater rotation angle of the robotic arm; (3) reduced hand tremors on the surgery; (4) no need to hold the mirror, optimizing the experience of the surgical operator.
However, robotic surgery also has some disadvantages: (1) the surgery is expensive; (2) the system lacks haptic feedback, so the operator cannot perceive force feedback when performing separations, sutures, and knots; however, as the learning curve increases, the visual feedback of hand–eye coordination can compensate for the mechanical sensation of tactile feedback; (3) the installation time is long; (4) it is not possible to change the position of instruments and operators during the procedure as needed; (5) the esthetics of the surgical incision is not as good as that of laparoscopic surgery.
Robotic surgery has a bright future in the treatment of congenital choledochal dilatation and deserves to be promoted and popularized. The robot, which has larger diameter operating instruments, shows its operational limitations in younger children, but its advantage is that the operating arm is flexible and can be operated at various angles. As robotic surgical systems continue to improve, it is likely that in the future their design direction will tend to accommodate smaller volume surgical objects. The effectiveness of different types of cysts for different surgical procedures is also an issue that needs to be taken into account. This requires more cases and classification by cyst type for comparative studies.
Data availability
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
References
Ishibashi H, Shimada M, Kamisawa T et al (2017) Japanese clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci 24:1–16. https://doi.org/10.1002/jhbp.415
Babbitt DP (1969) Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb. Ann Radiol (Paris) 12:231–240
Lee HK, Park SJ, Yi BH et al (2009) Imaging features of adult choledochal cysts: a pictorial review. Korean J Radiol 10:71–80. https://doi.org/10.3348/kjr.2009.10.1.71
Sato M, Ishida H, Konno K et al (2001) Choledochal cyst due to anomalous pancreatobiliary junction in the adult: sonographic findings. Abdom Imaging 26:395–400. https://doi.org/10.1007/s002610000184
Gigot JF, Nagorney DM, Farnell MB et al (1996) Bile duct cysts: a changing spectrum of presentation. J Hepatobiliary Pancreat Surg 3:405–411. https://doi.org/10.1007/BF02349784
Dawrant MJ, Najmaldin AS, Alizai NK (2010) Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children less than 10 kg. J Pediatr Surg 45:2364–2368. https://doi.org/10.1016/j.jpedsurg.2010.08.031
O’Neill JA Jr (1992) Choledochal cyst. Curr Probl Surg 29:361–410. https://doi.org/10.1016/0011-3840(92)90025-x
Jones RE, Zagory JA, Clark RA et al (2021) A narrative review of the modern surgical management of pediatric choledochal cysts. Transl Gastroenterology Hepatol 6:37. https://doi.org/10.21037/tgh-20-235
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Koga H, Murakami H, Ochi T et al (2019) Comparison of robotic versus laparoscopic hepaticojejunostomy for choledochal cyst in children: a first report. Pediatr Surg Int 35:1421–1425. https://doi.org/10.1007/s00383-019-04565-3
Cai DT, Chen QJ, Zhang LF et al (2022) Comparative study of Da Vinci technique versus traditional laparoscopic technique in the treatment of choledochal cyst[J]. J Clin Ped Sur 21:51–57. https://doi.org/10.3760/cma.j.cn.101785-202012066-010
Xie XL, Li KW, Chuan W et al (2021) Clinical efficacy of Da Vinci (SI) robot-assisted choledochal cyst excision in pediatrics. Chin J Pediatr Surg 42:610–616
Cai DT, Gao ZG, Chen QJ et al (2021) Experience of mini-invasive treatment for Todani type II choledochal cyst in children. Chin J Pediatr Surg 42:622–628
Xiao YH, Zhang X, Zhao GD et al (2019) Pathologic features and minimal invasive procedures for Caroli disease in children. Acad J Chin PLA Med Sch 40:140–144. https://doi.org/10.3969/j.issn.2095-5227.2019.02.009
Egger M, Smith GD (1998) Bias in location and selection of studies. BMJ 316:61–66. https://doi.org/10.1136/bmj.316.7124.61
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Xie X, Li K, Wang J et al (2020) Comparison of pediatric choledochal cyst excisions with open procedures, laparoscopic procedures and robot-assisted procedures: a retrospective study. Surg Endosc 34:3223–3231. https://doi.org/10.1007/s00464-020-07560-1
Chi SQ, Cao GQ, Li S et al (2021) Outcomes in robotic versus laparoscopic-assisted choledochal cyst excision and hepaticojejunostomy in children. Surg Endosc 35:5009–5014. https://doi.org/10.1007/s00464-020-07981-y
Dong LL, Chu ZH, Cui XC et al (2021) A comparative study of da Vinci robot versus traditonal laproscopy for congenital choledochal cyst in children. Chin J Pediatr Surg 42:17–22. https://doi.org/10.3760/cma.j.cn421158-20191022-00603
Chan EKW, Lee KH, Wong VHY, Tsui BSY, Wong SYS, Pang KKY et al (2018) Laparoscopic management of choledochal cysts in infants and children: a review of current practice. Surg Pract 22:131–137. https://doi.org/10.1111/1744-1633.12310
Lin S, Chen J, Tang K et al (2022) Trans-umbilical single-site plus one robotic assisted surgery for choledochal cyst in children, a comparing to laparoscope-assisted procedure. Front Pediatr 10:806919. https://doi.org/10.3389/fped.2022.806919
Chi SQ, Xu YH, Tang ST et al (2021) Comparison between robot-assisted and traditional laparoscopic surgery on choledochal cyst excision and hepaticojejunostomy in children [J]. Chinese Journal of Robotic Surgery. 2:248–254. https://doi.org/10.12180/j.issn.2096-7721.2021.04.002
Diao M, Li L, Cheng W (2013) Role of laparoscopy in treatment of choledochal cysts in children. Pediatr Surg Int 29:317–326. https://doi.org/10.1007/s00383-013-3266-z
Yin T, Chen S, Li Q et al (2022) Comparison of outcomes and safety of laparoscopic and robotic-assisted cyst excision and hepaticojejunostomy for choledochal cysts: a systematic review and meta-analysis. Ann Med Sur 75:103412. https://doi.org/10.1016/j.amsu.2022.103412
Kim NY, Chang EY, Hong YJ et al (2015) Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J 56:737–743. https://doi.org/10.3349/ymj.2015.56.3.737
Baison GN, Bonds MM, Helton WS et al (2019) Choledochal cysts: similarities and differences between Asian and western countries. World J Gastroenterol 25:3334–3343. https://doi.org/10.3748/wjg.v25.i26.3334
Giulianotti PC, Coratti A, Angelini M et al (2003) Robotics in general surgery: personal experience in a large community hospital. Arch Surg 138:777–784. https://doi.org/10.1001/archsurg.138.7.777
Sodergren MH, Darzi A (2013) Robotic cancer surgery. Br J Surg 100:3–4. https://doi.org/10.1002/bjs.8972
Funding
This study was funded by the Natural Science Foundation of Xinjiang Uygur Autonomous Region (Grant number: 2021D01A38).
Author information
Authors and Affiliations
Contributions
RZ, SL, and TL contributed to the conception, design of the study, and drafting of the article. JZ contributed to revising the article critically for important intellectual content and contributed to the final approval of the version to be submitted. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The keyword of the search was (((((((((((((((((((((((((((((((((((((((((Choledochal Cyst[Title/Abstract]) OR (Choledochal Cysts[Title/Abstract])) OR (Cyst, Choledochal[Title/Abstract])) OR (Congenital Choledochal Cyst[Title/Abstract])) OR (Choledochal Cyst, Congenital[Title/Abstract])) OR (Congenital Choledochal Cysts[Title/Abstract])) OR (Cyst, Congenital Choledochal[Title/Abstract])) OR (Bile Duct Cysts[Title/Abstract])) OR (Bile Duct Cyst[Title/Abstract])) OR (Cyst, Bile Duct[Title/Abstract])) OR (Duct Cyst, Bile[Title/Abstract])) OR (Choledochocele[Title/Abstract])) OR (Choledochoceles[Title/Abstract])) OR (Choledochal Cyst, Type II[Title/Abstract])) OR (Choledochal Diverticulum[Title/Abstract])) OR (Choledochal Diverticulums[Title/Abstract])) OR (Diverticulum, Choledochal[Title/Abstract])) OR (Choledochal Cyst, Diverticulum[Title/Abstract])) OR (Choledochal Cysts, Diverticulum[Title/Abstract])) OR (Diverticulum Choledochal Cyst[Title/Abstract])) OR (Diverticulum Choledochal Cysts[Title/Abstract])) OR (Congenital Biliary Dilatation[Title/Abstract])) OR (Biliary Dilatation, Congenital[Title/Abstract])) OR (Congenital Biliary Dilatations[Title/Abstract])) OR (Dilatation, Congenital Biliary[Title/Abstract])) OR (Choledochal Cyst, Type IV[Title/Abstract])) OR (Multiple Choledochal Cysts[Title/Abstract])) OR (Choledochal Cyst, Multiple[Title/Abstract])) OR (Cyst, Multiple Choledochal[Title/Abstract])) OR (Multiple Choledochal Cyst[Title/Abstract])) OR (Choledochal Cyst, Type V[Title/Abstract])) OR (Intrahepatic Choledochal Cyst[Title/Abstract])) OR (Choledochal Cyst, Intrahepatic[Title/Abstract])) OR (Cyst, Intrahepatic Choledochal[Title/Abstract])) OR (Intrahepatic Choledochal Cysts[Title/Abstract])) OR (Choledochal Cyst, Type I[Title/Abstract])) OR (Common Bile Duct Cyst[Title/Abstract])) OR (Cyst, Common Bile Duct[Title/Abstract])) OR (Cysts, Common Bile Duct[Title/Abstract])) OR (Choledochal Cyst, Type III[Title/Abstract])) AND ((((((((((((((((((((((((((Robotic Surgical Procedures[Title/Abstract]) OR (Procedure, Robotic Surgical[Title/Abstract])) OR (Procedures, Robotic Surgical[Title/Abstract])) OR (Robotic Surgical Procedure[Title/Abstract])) OR (Surgical Procedure, Robotic[Title/Abstract])) OR (Robot Surgery[Title/Abstract])) OR (Robot Surgeries[Title/Abstract])) OR (Surgery, Robot[Title/Abstract])) OR (Robot-Assisted Surgery[Title/Abstract])) OR (Robot Assisted Surgery[Title/Abstract])) OR (Robot-Assisted Surgeries[Title/Abstract])) OR (Surgery, Robot-Assisted[Title/Abstract])) OR (Robot-Enhanced Procedures[Title/Abstract])) OR (Procedure, Robot-Enhanced[Title/Abstract])) OR (Robot Enhanced Procedures[Title/Abstract])) OR (Robot-Enhanced Procedure[Title/Abstract])) OR (Surgical Procedures, Robotic[Title/Abstract])) OR (Robotic-Assisted Surgery[Title/Abstract])) OR (Robotic Assisted Surgery[Title/Abstract])) OR (Robotic-Assisted Surgeries[Title/Abstract])) OR (Surgery, Robotic-Assisted[Title/Abstract])) OR (Robot-Enhanced Surgery[Title/Abstract])) OR (Robot Enhanced Surgery[Title/Abstract])) OR (Robot-Enhanced Surgeries[Title/Abstract])) OR (Surgery, Robot-Enhanced[Title/Abstract])) OR (Robotic[Title/Abstract]))) AND (((((((((((((Research Support, U.S. Government [Publication Type]) OR (Research Support, American Recovery and Reinvestment Act [Publication Type])) OR (Research Support, N.I.H., Extramural [Publication Type])) OR (Research Support, N.I.H., Intramural [Publication Type])) OR (Research Support, U.S. Gov't, P.H.S. [Publication Type])) OR (Research Support, U.S. Gov't, Non-P.H.S. [Publication Type])) OR (Research Support, Non-U.S. Gov't [Publication Type])) OR (Support, Non-U.S. Gov't[Publication Type])) OR (Support, Non-U.S. Govt[Publication Type])) OR (Support, Non U.S. Gov't[Publication Type])) OR (Support, Non U.S. Govt[Publication Type])) OR (Comparative Study[Publication Type])) OR (Comparative Studies[Publication Type])).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, R., Liu, S., Li, T. et al. Efficacy of robot-assisted hepaticojejunostomy and laparoscopic-assisted hepaticojejunostomy in pediatric congenital choledochal dilatation: a system review and meta-analysis. Pediatr Surg Int 39, 46 (2023). https://doi.org/10.1007/s00383-022-05286-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-022-05286-w