Abstract
Background
Pediatric trauma patients sustaining blunt abdominal trauma (BAT) with intra-abdominal injury (IAI) are frequently admitted to the intensive care unit (ICU). This study was performed to identify predictors for ICU admission following BAT.
Methods
Prospective study of children (< 16 years) who presented to 14 Level-One Pediatric Trauma Centers following BAT over a 1-year period. Patients were categorized as ICU or non-ICU patients. Data collected included vitals, physical exam findings, laboratory results, imaging, and traumatic injuries. A multivariable hierarchical logistic regression model was used to identify predictors of ICU admission. Predictive ability of the model was assessed via tenfold cross-validated area under the receiver operating characteristic curves (cvAUC).
Results
Included were 2,182 children with 21% (n = 463) admitted to the ICU. On univariate analysis, ICU patients were associated with abnormal age-adjusted shock index, increased injury severity scores (ISS), lower Glasgow coma scores (GCS), traumatic brain injury (TBI), and severe solid organ injury (SOI). With multivariable logistic regression, factors associated with ICU admission were severe trauma (ISS > 15), anemia (hematocrit < 30), severe TBI (GCS < 8), cervical spine injury, skull fracture, and severe solid organ injury. The cvAUC for the multivariable model was 0.91 (95% CI 0.88–0.92).
Conclusion
Severe solid organ injury and traumatic brain injury, in association with multisystem trauma, appear to drive ICU admission in pediatric patients with BAT. These results may inform the design of a trauma bay prediction rule to assist in optimizing ICU resource utilization after BAT.
Study design
Prognosis study.
Level of evidence
1.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Blunt trauma is the most common mechanism of injury in children and intraabdominal injury (IAI) occurs in 6–8% of pediatric trauma patients with common causes including motor vehicle collision (MVC), automobile versus pedestrian or bicyclist, other motorized vehicle accidents, bicycle accidents, and falls [1,2,3]. Blunt abdominal trauma (BAT) can result in a wide range of injuries with solid organ injury (SOI) being the most common [4]. Thankfully, mortality directly related to traumatic IAI is low (1–2%) [1]. Despite low mortality, children sustaining blunt abdominal trauma may require admission to the intensive care unit (ICU).
Historically, ICU admission for hemodynamically stable children with isolated liver and spleen injury was determined by grade of organ injury [5]. However, further investigations have shown that injury grade may not be the best predictor of need for ICU care [6,7,8,9,10]. Additionally, a physiologic based management strategy may improve quality of care due to notable cost savings without any detriment on outcomes [7]. In the case of patients with complex poly-trauma and BAT, the need for advanced care may be much more likely [11]. Appropriate distribution of resources is essential in high quality trauma care. In order to prioritize such resources, it is important to know what patient populations are at highest risk for intervention and need for critical care.
The purpose of our study was to (1) describe the characteristics of children who have sustained BAT and were admitted to the ICU and (2) propose predictors that could help guide appropriate ICU resource utilization in this population. We hypothesized that those admitted to the ICU would have increased hemodynamic and laboratory derangements and would have a greater number of more severe injuries.
Methods
Data collection
A multi-institutional, prospective, observational study was performed by Streck et al. [3] in association with the Pediatric Surgery Research Collaborative, to identify children at very low risk for IAI who could safely avoid computer tomography (CT). We performed a planned sub-analysis of that data in order to identify the characteristics and predictors of ICU admission in children who sustained BAT.
Fourteen level-1 trauma centers provided data for analysis. Institutional Review Board approval was obtained from each participating site prior to study enrollment and data collection. Children < 16 years of age with BAT were enrolled over a 1-year period from August 2014 to July 2015. Those included in the study were of the highest two levels of trauma activation and had either blunt torso injury or a trauma consult with abdominal pain. Those who were excluded presented more than 6 h after injury, had isolated head or extremity injury, or had CT imaging prior to arrival.
Data related to demographics, injury characteristics, trauma activation, vitals, symptoms, physical exam findings, laboratory results, imaging, and trauma bay disposition were collected prospectively for analysis. Vitals, symptoms, exam findings, and laboratory values were obtained only at initial evaluation in the trauma bay. The shock index (SI) for each patient was calculated (initial heart rate/initial systolic blood pressure). Abnormal SI was determined for different age groups (4–6 years, > 1.22; 7–12 years, > 1.0; and > 12 years, > 0.9). Glasgow coma scale (GCS) was further classified as mild traumatic brain injury (TBI) (GCS 14–15), moderate TBI (GCS 9–13), or severe TBI (GCS < 8). Kidney, liver, and spleen injuries were collectively defined as SOI. Hollow viscus injuries were defined as duodenal, jejunoileal, colon, and mesentery. Urologic injuries were defined as bladder and ureteral. Criteria for trauma activation was left to the individual institutions, and thus not standardized. Criteria for ICU admission was also not standardized and left to the discretion of the attending physician. Chart review and review of the trauma registry was used to obtain follow-up data within 30-days of discharge which included additional injury findings, procedural interventions, intraoperative findings and treatment, and hospital outcomes such as mortality and hospital length of stay (LOS). All data points were de-identified and entered into a shared REDCap (research Electronic Data Capture) database.
Statistical analysis
A cohort analysis was performed comparing ICU and non-ICU patients. A subset analysis was also performed evaluating only patients with confirmed IAI. Descriptive statistics were used to evaluate the study populations. Categorical variables were analyzed using Chi-square and Fisher’s exact test and are reported as a percentage. Continuous variables were analyzed using two-sample Student t test and are reported as, median with interquartile ranges (IQR). A multivariable hierarchical logistic regression model (clustering within hospitals) was used to evaluate the association between different exposures and ICU admission. Model covariates were selected a priori and include age, age-adjusted SI (normal/abnormal), severe trauma (Injury Severity Score (ISS) > 15), anemia (hematocrit < 30), moderate TBI, severe TBI, cervical spine injury, skull fracture, facial fracture, and high-grade SOI (grade ≥ 3). The ability of the model covariates to predict ICU admission was determined by a k-fold cross validated area under (cvAUC) the receiver operating characteristic (ROC) curve. K-fold cross validation avoids the optimistic estimates of predictive performance known to exist when the full dataset is used for both model specification and prediction assessment. In k-fold cross validation, the dataset is randomly partitioned into k approximately equal sized subsamples (or folds). For each iteration, onefold is retained as the validation data for testing the model and estimating the cvAUC, while the remaining k − 1 folds are used as training data for model estimation. This process is repeated k times, with each of the k folds used once as the validation data [12]. A k-fold of 10 was applied to our study population. The ‘cvauroc’ command in Stata was used to derive and average these tenfold cvAUCs, and estimate its associated 95% bias corrected CI [13]. The predictive ability of the model by cvAUC was evaluated using the definitions provided by Hosmer and Lemeshow (0.5 ‘no discrimination’, 0.7–0.9 ‘excellent’, and > 0.9 ‘outstanding’) [14]. Additionally, two sensitivity analyses were performed to further evaluate the primary regression model. The first evaluated patients with confirmed IAI and the second evaluated patients that proceeded to the operating room or interventional radiology suite prior to ICU admission. Adjusted odds ratio (AOR) and 95% confidence interval (CI) were calculated. A p value of < 0.05 was considered significant. All analyses were performed using Stata version 16.0 (StataCorp, College Station, TX).
Results
Demographics and trauma mechanism
A total of 2182 children were included in the study with 463 (21%) admitted to the ICU and 1719 (79%) not admitted to the ICU (non-ICU). The median patient age was 8 [IQR 4–12] years. Half of the population was Caucasian (1071 (50%)) and 36% were African American. Only 12% identified as Hispanic. The median injury severity score was 5 [IQR 1–11]. The most common mechanisms of injury were MVC (46%), auto versus pedestrian or bicyclist (20%), all-terrain vehicle (8%), fall (7%), and bicycle (4%). An additional 15% of children had other mechanisms of injury which included assault and other motorized vehicles. Children admitted to the ICU had a lower rate of MVC (ICU 174 (38%), non-ICU 839 (49%); p < 0.01), and a higher rate of assault (ICU 25 (5%), non-ICU 33 (2%); p < 0.01).
Injury severity, vitals, laboratory assessment, and imaging
Injury severity, vitals, and SI were significantly worse in the ICU cohort (Table 1). FAST exam and chest X-ray were also more often abnormal in the ICU group. Laboratory results on arrival were significantly different between the two cohorts, with ICU patients having lower hematocrit and higher AST laboratory values.
Intra-abdominal injuries
Findings of IAI were much more common in children admitted to the ICU compared to non-ICU children (ICU 133 (29%), non-ICU 126 (7%); p < 0.001). Both patients with low- and high-grade SOI were more likely to be admitted to the ICU (Table 2). Of the patients admitted to the ICU with low-grade SOI, 28 (53%) were tachycardic, 5 (9%) were hypotensive, and 13 (25%) had an abnormal SI with 33 (62%) patients having at least one of these vital sign abnormalities (Table 3). Of the patients admitted to the ICU with high-grade SOI, 37 (60%) were tachycardic, 6 (10%) were hypotensive, and 16 (26%) had an abnormal SI with 41 (66%) patients having at least one of these vital sign abnormalities. All patients admitted to the ICU with either low- or high-grade SOI and normal vital signs had at least a mild TBI (Table 3). Similarly, hollow viscus, abdominal wall, and urologic injuries were more common in the ICU cohort. There was no difference in pancreatic or vascular injury.
Additional traumatic injuries, interventions, and outcomes
Many patients had other injuries in addition to intra-abdominal injuries. Compared to non-ICU patients, children admitted to the ICU had more intracranial, craniofacial, thoracic, and pelvic injuries (Fig. 1). ICU patients underwent more interventions including blood transfusion, intracranial pressure monitor placement, angioembolization, craniotomy, and laparotomy (Table 4). There was no difference in rate of laparoscopy. Eight percent (35/463) of patients eventually admitted to the ICU were initially taken to the operating room (n = 34) or interventional radiology suite (n = 1).
Outcomes were worse for those admitted to the ICU. Thirty-day mortality occurred in 36 (8%) ICU patients compared to 6 (< 1%) non-ICU patients (p < 0.01). Hospital length of stay was also longer for ICU patients with a median length of 5 [3–11] days compared to 2 [1–2] days (p < 0.01).
Subset analysis, confirmed intra-abdominal injuries
A subset analysis was performed to look at children with confirmed IAI after BAT. Of those children, 133 (51%) were admitted to the ICU and 126 (49%) were non-ICU. Fewer children with confirmed IAI went to the ICU after bike crash [ICU 1 (< 1%), non-ICU 8 (6%); p = 0.02]. Children with IAI admitted to the ICU were more likely to be hypotensive [ICU 14 (11%), non-ICU 3 (2%); p = 0.01], tachycardic [ICU 74 (56%), non-ICU 33 (26%); p < 0.01], and have an abnormal SI [ICU 37 (28%), non-ICU 10 (8%); p < 0.01]. The rate of abnormal FAST exams [ICU 16 (12%), non-ICU 11 (9%); p = 0.39] was comparable between the cohorts, but the ICU cohort was significantly more likely to have an abnormal chest X-ray [ICU 57 (43%), non-ICU 21 (17%); p < 0.01]. Children with confirmed IAI admitted to the ICU were more likely to have anemia [ICU 32 (42%), non-ICU 5 (4%); p < 0.01] and AST > 200 [ICU 79 (59%), non-ICU 46 (37%); p < 0.01].
There was no difference between the cohorts for hollow viscus injury [ICU 20 (15%), non-ICU 29 (23%); p = 0.10], pancreatic injury [ICU 5 (4%), non-ICU 7 (6%); p = 0.56], urologic injury [ICU 7 (5%), non-ICU 3 (2%); p = 0.33], or low-grade SOI [ICU 53 (40%), non-ICU 45 (36%); p = 0.49]. However, high-grade SOI was significantly more likely to be admitted to the ICU [ICU 62 (47%), non-ICU 36 (29%); p < 0.01]. ICU patients were more likely to have severe TBI [ICU 43 (32%), non-ICU 1 (< 1%); p < 0.01], skull fractures [ICU 30 (23%), non-ICU 5 (4%); p < 0.01], cervical spine injuries [ICU 13 (10%), non-ICU 1 (< 1%); p < 0.01], facial fractures [ICU 27 (20%), non-ICU 8 (6%); p < 0.01], and thoracic injuries [ICU 74 (56%), non-ICU 28 (22%); p < 0.01]. In contrast non-ICU patients were more likely to have mild TBI [ICU 74 (56%), non-ICU 116 (92%); p < 0.01].
Transfusion [ICU 26 (20%), non-ICU 0 (0%); p < 0.01], intracranial pressure monitor placement [ICU 13 (10%), non-ICU 0 (0%); p < 0.01], and angioembolization [ICU 7 (5%), non-ICU 0 (0%); p < 0.01] were more frequently performed in the ICU cohort. However, the rate of laparoscopy [ICU 6 (5%), non-ICU 11 (9%); p = 0.17], craniotomy [ICU 5 (4%), non-ICU 0 (0%); p = 0.06], and laparotomy [ICU 18 (14%), non-ICU 14 (11%); p = 0.55] was comparable between the groups.
Multivariate analysis, cvAUC, and sensitivity analyses
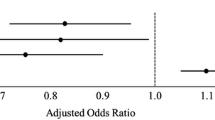
For the entire study population, ICU admission was significantly associated with abnormal SI, severe trauma, anemia, moderate TBI, severe TBI, cervical spine injury, skull fracture, and high-grade SOI (Table 5). Figure 2 depicts the tenfold ROC curves derived from the multivariable model. The averaged cvAUC was 0.91 (95% CI 0.88–0.92).
Tenfold cross-validation ROC curves for ICU admission following pediatric blunt abdominal trauma derived from multivariable hierarchical logistic regression. Mean cvAUC (solid red curve) and k-fold ROC curves (dashed curves --). ROC receiver operating characteristic curve, cvAUC cross-validation area under the curve
When limiting the model only to children with confirmed IAI, ICU admission was only associated with abnormal SI, severe trauma, severe TBI, and high-grade SOI. And when evaluating children that were taken to the operating room or interventional radiology suite prior to ICU admission, intensive care was only associated with abnormal SI, severe trauma, and skull fracture.
Discussion
Several studies have utilized trauma scores (i.e. Abbreviated Injury Scale, ISS, Pediatric Trauma Score, and trauma related ISS), physiologic parameters, and laboratory abnormalities to predict in-hospital morbidity and/or the need for ICU admission [11, 15]. Additionally, clinical decision-making tools have been created to help clinicians triage patients and utilize trauma resources appropriately [3, 7, 16]. Our results highlight several important findings for future prediction tools to ensure appropriate resource utilization in the trauma setting. First, ICU admissions in our study cohort were associated with significantly more abnormalities in vital signs (including SI), laboratory values, and imaging results. Second, all categories of IAI were associated with ICU admission, except pancreatic and vascular injuries. When limiting the analysis to children with confirmed IAI, the only abdominal injury associated with admission to the ICU was high-grade SOI. When controlling for potential confounding variables (e.g. moderate and severe TBI) in our multivariate analysis, severe SOI was still associated with ICU admission for the entire study population and children with confirmed IAI. And finally, ICU admissions were associated with significantly more non-abdominal injuries, most notably central nervous system (CNS) injuries (i.e. TBI, skull fractures, cervical spine injury).
BAT requiring ICU admission is associated with significantly more physiologic and lab derangements. Of those patients admitted to the ICU, approximately 40% had tachycardia, 16% had abnormal SI, and less than 10% were hypotensive. These are obvious indications for ICU admission; however, an important realization is the majority of patients eventually admitted did not have significant physiologic derangements. This is likely secondary to the pediatric patient’s physiologic reserve and lack of vital sign changes until decompensation is imminent. Additionally, certain injuries that are associated with ICU admission (e.g. TBI) do not always lead to physiologic abnormalities. This observation highlights the need for laboratory and imaging studies to provide additional information to triage trauma patients. All laboratory values evaluated were significantly different between the two cohorts with multivariate analysis further identifying anemia (i.e. hematocrit < 30) was associated with a fourfold increase in the odds of ICU admission. A positive FAST (6%) and abnormal chest X-ray (27%) was identified in less than a third ICU admissions, suggesting the limited ability of these specific imaging adjuncts to determine ICU admission. These findings highlight the importance of utilizing several different variables at the time of initial assessment when considering ICU admission.
Approximately 30% of the ICU admissions had IAI with severe SOI identified as the most common injury. American Pediatric Surgical Association guidelines previously recommended grade of organ injury should determine ICU admission in hemodynamically stable children [5]. However, several studies have since shown that isolated SOI is safely managed in the wards, unless there is significant hemodynamic instability requiring an intervention [6,7,8,9]. Our multivariate model identified severe SOI was associated with ICU admission for the entire study population and when limited to children with confirmed IAI. Hemodynamic instability (identified as hypotension, tachycardia, or abnormal SI) was identified in approximately 65% of patients admitted to the ICU with any SOI. Importantly, all children admitted to the ICU with normal vitals and a SOI had some degree of TBI. These results highlight that the combination of CNS and IAI injuries were potentially driving the admission in hemodynamically stable patients with SOI. Therefore, at the time of the study, physicians appeared to be following current guidelines to avoid ICU admission for SOI without hemodynamic instability.
Complex poly-trauma involving multiple organ systems is most likely to require admission to the pediatric ICU. TBI, skull fracture, facial fracture, and thoracic injuries each occurred in > 20% of patients admitted to ICU following BAT with TBI (moderate or severe) the highest at almost 60%. Thus, at least half of the ICU patients had traumatic injuries to ≥ 2 organ systems. Also, moderate TBI, severe TBI, cervical spine injury, and skull fractures were associated with ICU admission based on multivariate analysis of the entire study population. The combination of any of these injuries, especially severe TBI, with abdominal injury is reflective of high mechanism blunt trauma. Furthermore, the cvAUC for our multivariate model was 0.91, which is a recognized indicator of ‘outstanding’ generalizable performance in predicting the outcome of interest. Therefore, our results highlight that multi-organ injury is a strong predictor of ICU admission. Ultimately, our results emphasize that future models created to guide trauma and critical care resource utilization should incorporate the severity and number of organs injured.
There are several limitations to our study. First, our study does not contain real-time hemodynamic data from the trauma bay with associated trends. The evaluation of a trauma patient is a dynamic assessment with clinical decisions made as new data becomes available. The variables we evaluated are snapshots during the initial assessment of the trauma patient. A normotensive patient that becomes hypotensive and is unresponsive to fluids is significantly different than an initially hypotensive patient that responds following resuscitation. A second limitation is the lack of relevant initial laboratory values besides hematocrit, such as base deficit and international normalized ratio. A third limitation is the inability to determine the indication for the provider’s decision to admit to the ICU. Similarly, there were no protocols or criteria in place for ICU admission. Therefore, the nature of our study only allows us to retrospectively evaluate certain factors that possibly influenced the clinician’s decision-making process. A fourth limitation is the study was performed across 14 different level-1 pediatric trauma centers with different trauma protocols and practice patterns in place. At the time of the study, different trauma centers likely had different thresholds based on physiologic parameters, lab values, and imaging studies that led admission to the ICU. To account for local practices within a hospital, we performed a multivariable hierarchical logistic regression to account for clustering within hospitals.
Conclusion
There has always been a need to assess and triage patients in the trauma bay. This need has influenced studies for the past 30 years to identify prediction rules to guide management and trauma resource utilization, which includes ICU resource utilization [11, 15, 17, 18]. With multivariate analysis, several factors were identified with a significant association with ICU admission: ISS > 15, hematocrit < 30, severe TBI, moderate TBI, cervical spine injury, skull fracture, and severe SOI. The combination of these variables in a multivariate model had an ‘outstanding’ predictive capability (> 0.90 cvAUC) for ICU admission. These results lay the foundation for future studies designed to generate a trauma bay prediction rule to assist in guiding and optimizing ICU admission following BAT.
Abbreviations
- IAI:
-
Intra-abdominal injury
- MVC:
-
Motor vehicle collision
- BAT:
-
Blunt abdominal trauma
- SOI:
-
Solid organ injury
- ICU:
-
Intensive care unit
- CT:
-
Computed tomography
- SI:
-
Shock index
- GCS:
-
Glascow coma scale
- TBI:
-
Traumatic brain injury
- LOS:
-
Length of stay
- IQR:
-
Interquartile range
- ISS:
-
Injury severity score
- cvAUC:
-
Cross-validated area under the curve
- ROC:
-
Receiver operating characteristic curve
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
References
Cooper A et al (1994) Mortality and truncal injury: the pediatric perspective. J Pediatr Surg 29(1):33–38
Holmes JF et al (2013) Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med 62(2):107–116 (e2)
Streck CJ et al (2017) Identifying children at very low risk for blunt intra-abdominal injury in whom CT of the abdomen can be avoided safely. J Am Coll Surg 224(4):449–458 (e3)
Wisner DH et al (2015) Management of children with solid organ injuries after blunt torso trauma. J Trauma Acute Care Surg 79(2):206–214 (quiz 332)
Leinwand MJ, Atkinson CC, Mooney DP (2004) Application of the APSA evidence-based guidelines for isolated liver or spleen injuries: a single institution experience. J Pediatr Surg 39(3):487–490 (discussion 487-90)
Fremgen HE et al (2014) Pediatric liver lacerations and intensive care: evaluation of ICU triage strategies. Pediatr Crit Care Med 15(4):e183–e191
Krieger AR et al (2012) Efficacy of anatomic and physiologic indicators versus mechanism of injury criteria for trauma activation in pediatric emergencies. J Trauma Acute Care Surg 73(6):1471–1477 (discussion 1477)
McVay MR et al (2008) Throwing out the “grade” book: management of isolated spleen and liver injury based on hemodynamic status. J Pediatr Surg 43(6):1072–1076
Mehall JR et al (2001) Prospective results of a standardized algorithm based on hemodynamic status for managing pediatric solid organ injury. J Am Coll Surg 193(4):347–353
Plumblee L et al (2020) Isolated low-grade solid organ injuries in children following blunt abdominal trauma: is it time to consider discharge from the emergency department? J Trauma Acute Care Surg 89(5):887–893
Narci A et al (2009) The prognostic importance of trauma scoring systems in pediatric patients. Pediatr Surg Int 25(1):25–30
Namasivayam A et al (2020) Predictors of modern contraceptive use among women and men in Uganda: a population-level analysis. BMJ Open 10(2):e034675
Luque-Fernandez MA, Redondo-Sánchez D, Maringe C (2019) cvauroc: Command to compute cross-validated area under the curve for ROC analysis after predictive modeling for binary outcomes. Stata J Promot Commun Stat Stata 19(3):615–625
Hosmer DW (2000) Applied logistic regression, 2nd edn. Wiley, New York
Hannan EL et al (2000) Predicting inpatient mortality for pediatric trauma patients with blunt injuries: a better alternative. J Pediatr Surg 35(2):155–159
Kong G et al (2015) Current state of trauma care in China, tools to predict death and ICU admission after arrival to hospital. Injury 46(9):1784–1789
Burd RS, Jang TS, Nair SS (2007) Evaluation of the relationship between mechanism of injury and outcome in pediatric trauma. J Trauma 62(4):1004–1014
Tepas JJ et al (1987) The pediatric trauma score as a predictor of injury severity in the injured child. J Pediatr Surg 22(1):14–18
Funding
No funding was used to conduct this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standard of the institutional research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mehl, S.C., Cunningham, M.E., Streck, C.J. et al. Characteristics and predictors of intensive care unit admission in pediatric blunt abdominal trauma. Pediatr Surg Int 38, 589–597 (2022). https://doi.org/10.1007/s00383-022-05067-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05067-5