Abstract
Cryptorchidism (CO) is a genital disorder of multifactorial etiology, with serious remote complications. Mutations in insulin-like 3 hormones (INSL3) G/A variant remain a matter of inquiry. We aimed to investigate the association between G178A-INSL3 polymorphism and undescended testis in a cohort of Egyptian children. In this study, a total of 160 children, including 80 cases with primary non-syndromic undescended testes and 80 healthy children with normal external genitalia as controls, both, were analyzed after detailed history, physical examination and imaging for mutations of G178A polymorphism of INSL3 gene by restriction fragment length polymorphism (RFLP) technique. We found most of the undescended testes were inside the inguinal canal mainly on the left side. Genetic analysis revealed that the mutant A allele of G178A INSL3 variant was significantly detected in the patient group with a frequency of 26.2% against 12.5% for control subjects, especially among cases with an evident family history of similar cases as shown by p value = 0.001 and odd's ratio (CI95%) of 0.13 (0.04–0.723). In conclusion, G178A—INSL3 gene polymorphism could be a susceptibility factor for testicular maldescent in Egyptian children. Also, family history of similar cases was considered as significant predictive risk for cryptorchidism, added to the shared genetic links to consanguinity in our locality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The undescended testis is considered the most common disorder of sex differentiation within boys; at birth, about 4.5% of them have an undescended testis. Because testicular descent occurs during the period of 7–8 months' gestation, 30% of premature male infants have an undescended testis, with an incidence of 3.4% at near term and an incidence decline to about 0.8% as a result of spontaneous testicles descent [1].
Testicular normal descent is thought to take place during two phases in fetal development between 8 and 15 weeks (the first phase of decent) and another second phase at 25–35 weeks gestation.[2].
The role of INSL3 on gubernaculum enlargement, anchoring the testes passively downward became more evident at early weeks' gestation. Between 25 and 35 weeks of gestational period, hormonal, neuronal and mechanical factors are incorporated to complete the anatomical descent of both testes [3].
Apart from the congenital type, acquired forms could also exist at which scarring is likely an important etiological factor [4].
A specific association of G178A-INSL3 gene polymorphism with cryptorchidism had been identified through animal and human studies in the recent years. The later polymorphism is shown to be localized to the C peptide region of the involved gene, resulting in amino acid change of an alanine to threonine. This amino acid alteration was thought to be responsible for interrupting the normal physiological sequence of testicular descent [5].
The undescended testicle may be prone to a variety of harmful consequences as trauma, torsion and inguinal hernias, and later on male infertility, atrophy, malignant transformation and psychological stress. Infertility ratios could be increased up to 40% in unilateral cryptorchidism, compared to a possibility of 70% in case of bilateral cryptorchidism.
Orchiopexy had been the mainstay line of treatment for placing the cryptorchid testicle into the scrotum in affected cases [6, 7].
In respect to the above considerations of possible remote serious complications, our study aimed to evaluate the association between G178A-INSL3 gene polymorphism and the development of undescended testis, and whether or/not it contributeed to its clinical appearance.
Patients and methods
Participants
Following the approval of the Institutional Ethical Committee of Menoufia University Hospital, and after obtaining written consents from the caregivers of all children to be included in this research, the study was carried out between April 2018 and March 2020, with all of its steps being done in Genetic Laboratory of the Genetics and Endocrinology Unit, Pediatric Department, Faculty of Medicine, Menoufia University Hospitals.
In this case–control study, a total of 160 children who were equally divided into two groups were included. Group (I) comprised 80 unrelated children with primary non-syndromic cryptorchidism; their phenotypic pattern was: 28 children with bilateral cryptorchidism, 28 children with unilateral left cryptorchidism and 24 children with unilateral right cryptorchidism, their ages ranging from 1 to 12 years with mean age of (3.89 ± 3.03) years.
Inclusion criteria included apparently normal male infants and children, as signed in the karyotype XY in the wholly analyzed lymphocytes, presented with unilateral or bilateral undescended testis.
Those with the following non-satisfactory criteria: infants less than 6 month's age, patients with abnormal syndromic features or having multiple congenital anomalies, those whose testes were retractile, or had a positive history of other surgical operation in the inguinal region were excluded from the work.
Group (II) included 80 apparently healthy non-cryptorchid male children collected from the general pediatric population who were chosen as control subjects. their ages ranged from 2 to 12 years with mean age of 4.13 ± 3.21 years.
All of the patients and normal control children were subjected to a detailed history taking, general examination, anthropometric measurements, and examination of the genitalia under the patient's authorization for complete ensured safety procedures. Size determination of the palpable testis was done in cases of unilateral UDT using a Prader Orchidometer, and data were referred to external masculinization score (EMS) for assessing the child external genetalia to provide a score out of 12 [8, 9]. Control subjects were assessed for their testicular size as well.
In addition to basic laboratory investigations and hormonal studies, pelvi-abdominal and inguino-scrotal ultrasound was done to show the site of each testis and the parenchymal structure and dimensions of the testes to calculate the testicular volume based on the following formula:
In the present study, the testicular size obtained for each case by ultrasonography was compared to the normal values reported by Lawal et al. (2016) [10]. Further radiological assessment was done accordingly whenever needed.
Molecular analysis of INSL3 gene polymorphism was applied through sequential steps as follows.
DNA was extracted from 2 ml (ml) of anti-coagulated peripheral blood collected into an EDTA tube by using a DNA extraction kit (Gene JET Whole Blood Genomic DNA Purification Mini Kit). Genomic DNA was then amplified using PCR with different forward and reverse primers (forward 5-AAA GAC TCG TTG CCC AGT GCT CCC T-3; reverse 5_-GCA TCT GCG CCT ACG TGC AC-3). The polymerase chain reaction (PCR) conditions for the amplification of exon 1 with primers F2/R1 were 95 °C for 5 min, followed by 33 cycles of 95 °C 40 s, 61 °C 35 s, 72 °C 45 s.
Restriction endoclease assay was applied for detecting non-silent gene alterations through the specifically used EagI restriction enzyme according to the manufacturer's conditions. The digested products were visualized on 2%agarose gel electrophoresis, after being stained with ethedium bromide, where the targeted enzyme recognized the wild G/G genotype certainly at the position 178(exon1) of INS3L gene.
Statistical analysis
IBM SPSS software version 20.0 (SPSS Inc., Chicago, Illinois, USA) was used for statistical analysis. The data were given as the mean ± the standard deviation and also as a range. The categorical data were analyzed by the Chi-square test. The latter was also performed for analyzing data about genotype differences and allelic distribution between patients and control groups. Continuous variables were compared using the t test. A P value < 0.05 was considered to be significant.
Results
One hundred and sixty full-term infants and children were categorized in this study with mean ages of 3.89 ± 3.03 years and 4.13 ± 3.21 years representing patients and control groups in order.
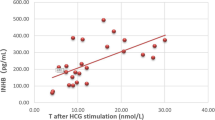
A statistically significant difference regarding history of similar cases with other group data is shown in Table 1. Most of the undescended testes were found inside the inguinal canal [47.5% on the right side and 57.5% on the left side] (Table 2). The genotype results and allele frequencies of G178A _ INSL3 gene polymorphism revealed a statistical significant difference between the patients and the apparently healthy normal control children (p = 0.003). GG genotype was more frequently observed among the control children compared with cases (80.0% versus 55.0%), respectively, while heterozygous GA and homozygous AA genotypes were more frequent in cases compared with the control group (37.5% versus 15.0% and 7.5% versus 5.0%), respectively (Table 3). The presence of mutant A allele and positive history of similar cases were significant predictive risk factors for occurrence of cryptorchidism using regression analysis as shown by odd's ratio (95% CI) 0.13 (0.04–0.723) and p value of 0.001 for A allele frequency.
The distribution of G178A_INSL3 polymorphisms (GG, GA, AA) in participant children with CO with respect to parents' ages, consanguinity and testicular site is shown in Table 4, where ten children at a percentage of 22.7% of those with GG genotype were born to a consanguineous marriage compared to eight children of GA genotype (26.6%) and three out of six affected children accounted for 50% of those children with AA genotype. The latter subgroup had a consanguinity of fourth degree.
Gel electrophoretic pattern of PCR-digest products on 2% agarose gel for G/A_INSL3 is shown in Fig. 1.
Discussion
Undescended testis is the most common urogenital problem in pediatrics. Normally intrauterine testicular descent occurs in two stages: transabdominal, then transinguinal. plenty number of intervening factors are responsible for undescended testis: genetic, hormonal and mechanical factors [7].
INSL3 gene comprised two exons in addition to one intron, contained in a single copy within the human genome. A specific association of detected mutations in the INSL3 gene in cases with bilateral cryptorchidism had been identified in human and animal studies, including the analyzed G/A SNP that leads to alanine (GCC) to the other amino acid threonine (ACC), at codon 60 of the C-peptide region [11, 12].
The study focused on the essential role of insulin-like 3hormone, derived from Leydig cells, in detecting a precise molecular pathogenic mechanism involved in integral gubernaculum differentiation and testicular descent [13]. Detailed background reviews from formal studies were directed to the identification of multiple defects within that gene [14,15,16,17,18,19,20]. Furthermore, it has recently gained great attention owing to the suggested paracrine-related role of INSL3 in male germ cell survival [21, 22].
While analyzing the results of molecular study of G178A_INSL3 gene polymorphism, in the present study it was found that a group difference of statistical significance was evident regarding the frequency distribution of A allele among patients with CO as shown by an odd's ratio (95% confidence interval) of 0.13 (0.04–0.723), p value = 0.001, in comparison to the reference G allele that was frequently observed in the group of control children at a percentage of 80%.
Also, the GG genotype was significantly linked to non-cryptorchid normal children (p < 0.05).
These findings were in agreement with those of Yamazawa et al. [23], who studied the G178A_INSL3 gene polymorphisms in 62 cryporchid patients and 60 control males and reached the result that the frequency of the G178A_INSL3 gene polymorphism genotypes (GG, GA and AA) was distributed between the cryptorchid patients and the controls as follows; 40.3%, 32.2%, 27.4% in patients versus 55%, 38.3%, 6.6% in controls, respectively, with a statistically significant difference (p = 0.0094).
On the other hand, Koskimies et al. [24] in their studies conducted on 30 cryptorchid boys and 89 controls for the G178A mutation found that the A allele frequency in both the homo- and heterozygous states was slightly higher (38.3%) than in the control subjects (29.7%) with otherwise non-significant difference.
Along with the spectrum of studies that favored the significant association of INSL3 G178A variant to primary non-syndromic CO was that of Huang et al. [25]. In this study, the sequencing of PCR-amplified coding regions of INSL3 in 97 azoospermic patients with a positive history of bilateral cryptorchidism represented the patient group, which they further divided into two subgroups according to the results of testes spermatic extraction, in contrast to a comparable group of 49 obstructive azoospermic males (control individuals). They reached conclusive findings of significant association of the studied variant to CO, whereas the damaged spermatogenic process could not be directly associated with G178A of INSL3 polymorphism among males with bilateral CO.
The distribution of cases with primary CO showed significant association with positive family history as shown in our results where the patients with (GG, GA, AA) genotypes showed that four (9%), six (20%) and two (33.3%) had positive family history of similar cases, respectively, with statistically significant difference between patients with GG and AA genotypes (p = 0. 0.004). This was not agreed by Mamoulakis et al. [26], who stated that the non-wild type (178A) was found at percentages of 52.9% and 42.3% of patient alleles with documented family history and sporadic CO patients (P = 0.240), showing no significant association between that polymorphism and positivity of family history. Burgu et al. similarly agreed with clustering of CO within certain families [27], taking into account the possibility that 178 A variant polymorphism may be a marker of consanguinity, as shown by an increased frequency of mutations made obviously because of genetic links in parents of children harboring the mutant allele.
Many authors reported that the association of inguinal hernia with cryptorchidism varied in the literature. Several studies suggested that cryptorchidism was almost always associated with an indirect inguinal hernia. Among those, Al-Abbadi and Smadi [28] conducted a study on 37 children, where undescended testis associated with indirect inguinal hernia was reported in 75.68% of patients. These findings were also concordant with that of Ravikumar et al. [29]. The processus vaginalis (PV) is a conduit, extending from the peritoneum down to the scrotum, usually obliterated after the end of the testicular migration. In cases where the vaginal processus did not close, the child could develop inguinal hernias or communicating hydrocele as a result of vaginal process persistence [30]. On the other hand, Tanyel et al. [31] clarified that despite the patency of that conduit in boys with undescended testis, clinical inguinal hernia is only encountered in 10–15% of cases.
Well seen in our study participants was the distribution of 178A variant among non-cryptorchid control infants and children at percentage of 5% versus 7.5% in CO patients, the matter that was extensively viewed in related research studies that interpreted the relevance of G178A nucleotide substitution to be claimed as a common polymorphic variant of human gene; INSL3 not linked to CO [32]. Mamoulakis et al. also studied the G178A_INSL3 gene polymorphisms in 170 cryptorchid patients and 50 control males and found that the wild-type nucleotide (178G) was found in 55.9% of patient and 55.0% of control alleles. Thus, the substitution represents common polymorphism unrelated to testicular maldescent (P = 0.876) [26].
It is possible that the G178A_INSL3 gene polymorphism represented one of the genetic factors associated with the existence of cryptorchidism, so that it can be detected in some patient populations, but not in others, depending on the attribution of other genetic, environmental and ethnic factors.
It is of great importance to discuss the clinical aspects and the diagnostic approaches with the family through counseling sessions, for implementing adequate intervention strategies, to avoid the possible complications or adverse proven testicular atrophy: an issue that was in accordance with Zvizdic et al., who reported that reduction of testicular size correlated with increasing the distance of maldescended testes away from the scrotum [33, 34].
Conclusion
The findings of this study indicated significant relevance of INSL3 178A allele to constitute a risk for susceptibility to cryptorchidism development with consideration to cases with positive family history along with worth continuation of molecular advances, thus, implying a new evidence for relation to testicular maldescent among Egyptian children.
Change history
21 September 2020
In the original publication,
References
Elder JS (2016) Disorders and anomalies of the scrotal contents. Nelson Textbook of Pediatrics. 20th ed. Elsevier, Philadelphia 2592
Gurney JK, McGlynn KA, Stanley J, Merriman T, Signal V, Shaw C, Edwards R, Richiardi L, Hutson J, Sarfati D (2017) Risk factors for cryptorchidism. Nature Rev Urol 14(9):534
Hutson JM, Terada M, Zhou B, Williams MP (2012) Normal testicular descent and the aetiology of cryptorchidism. Springer Science & Business Media, Berlin
Hutson JM, Thorup JM, Beasley SW (2016) The postnatal effects of cryptorchidism. InDescent of the Testis Springer, Cham, pp 81–103
Chedane C, Puissant H, Weil D, Rouleau S, Coutant R (2014) Association between altered placental human chorionic gonadotrophin (hCG) production and the occurrence of cryptorchidism: a retrospective study. BMC Pediatr 14(1):191
Kurz D, Tasian G (2016) Current management of undescended testes. Curr Treat Opt Pediatr 2(1):43–51
Hutson JM, Thorup J (2015) Evaluation and management of the infant with cryptorchidism. Curr Opin Pediatr 27(4):520–524
Dagli P, Jethava V, Sheth J (2014) Orchidometer-Useful office practice tool for assessment of male puberty. NHL J Med Sci 3(2):58–64
Su R, Adam MP, Ramsdell L, Fechner PY, Shnorhavorian M (2015) Can the external masculinisation score predict the success of genetic testing in 46, XY DSD. AIMS Genet 2(2):163
Lawal S, Idris HW, Ibinaiye P, Hamidu AU, Tabari MA, Usman B, Lawal AT (2016) Normative ultrasonographic values for testicular volumes in Nigerian boys aged 0–15 years. Sub-Saharan African J Med 3(2):71
Fenichel P, Lahlou N, Coquillard P, Panaia-Ferrari P, Wagner- Mahler K, Brucker-Davis F (2015) Cord blood insulin-like peptide 3 (INSL3) but not testosterone is reduced in idiopathic cryptorchidism. Clin Endocrinol (Oxf) 82:242–247
Ferlin A, Bogatcheva NV, Gianesello L, Pepe A, Vinanzi C, Agoulnik AI (2006) Foresta C (2006) Insulin-like factor 3 gene mutations in testicular dysgenesis syndrome: clinical and functional characterization. Mol Hum Reprod 12:401–406
Ivell R, Wade JD, Anand-Ivell R (2013) INSL3 as a biomarkerof Leydig cell functionality. Biol Reprod 88:147
Marin P, Ferlin A, Moro E, Rossi A, Bartoloni L, Rossato M, Foresta C (2001) Novel insulin-like 3 (INSL3) gene mutation associated with human cryptorchidism. Am J Med Genet 103:348–349
Tomboc M, Lee PA, Mitwally MF, Schneck FX, Bellinger M, Witchel SF (2000) Insulin-like 3/relaxin-like factor gene mutations are associated with cryptorchidism. J Clin Endocrinol Metab 85:4013–4018
Ferlin A, Zuccarello D, Zuccarello B, Chirico MR, Zanon GF, Foresta C (2008) Genetic alterations associated with cryptorchidism. JAMA 300:2271–2276
Foresta C, Ferlin A (2004) Role of INSL3 and LGR8 in cryptorchidism and testicular functions. Reprod Biomed Online 9:294–298
Feng S, Ferlin A, Truong A, Bathgate R, Wade JD, Corbett S, Han S, Tannour-Louet M, Lamb DJ, Foresta C, Agoulnik AI (2009) INSL3/RXFP2 signaling in testicular descent. Ann NY Acad Sci 1160:197–204
El Houate B, Rouba H, Sibai H, Barakat A, Chafik A, el Chadli B, Imken L, Bogatcheva NV, Feng S, Agoulnik AI, McElreavey K (2007) Novel mutations involving the INSL3 gene associated with cryptorchidism. J Urol 177:1947–1951
Canto P, Escudero I, Soderlund D, Nishimura E, Carranza- Lira S, Gutierrez J, Nava A, Mendez JP (2003) A novel mutation of the insulin-like 3 gene in patients with cryptorchidism. J Hum Genet 48:86–90
Assis LH, Crespo D, Morais RD, Franca LR, Bogerd J, Schulz RW (2015) INSL3 stimulates spermatogonial differentiation in testis of adult zebrafish (Danio rerio). Cell Tissue Res. https://doi.org/10.1007/s00441-015-2213-9
Sagata D, Minagawa I, Kohriki H, Pitia AM, Uera N, Katakura Y, Sukigara H, Terada K, Shibata M, Park EY, Hasegawa Y, Sasada H (2015) Kohsaka T (2015) The insulin-like factor 3 (INSL3)-receptor (RXFP2) network functions as a germ cell survival/anti-apoptotic factor in boar testes. Endocrinology 156:1523–1539
Yamazawa K, Wada Y, Sasagawa I, Aoki K, Ueoka K, Ogata T (2007) Mutation and polymorphism analyses of INSL3 and LGR8/GREAT in 62 Japanese patients with cryptorchidism. Hormone Res Paediatr 67(2):73–76
Koskimies P, Virtanen H, Lindström M, Kaleva M, Poutanen M, Huhtaniemi I, Toppari J (2000) A common polymorphism in the human relaxin-like factor (RLF) gene: no relationship with cryptorchidism. Pediatr Res 47(4):538
Huang X, Jia J, Sun M, Li M, Liu N (2016) Mutational screening of the INSL 3 gene in azoospermic males with a history of cryptorchidism. Andrologia 48(7):835–839
Mamoulakis C, Georgiou I, Dimitriadis F, Tsounapi P, Giannakis I, Chatzikyriakidou A, Antypas S, Sofras F, Takenaka A, Sofikitis N (2014) Genetic analysis of the human I nsulin-like 3 gene: absence of mutations in a G reek paediatric cohort with testicular maldescent. Andrologia 46(9):986–996
Burgu B, Baker LA, Docimo SG (2010) Ch. 43 Cryptorchidism. In: Pediatric Urology, Publisher, Elsevier Inc. 2nd edn. Philadelphia, W. B., pp 563–576
Al Abbadi K, Smadi SA (2000) Genital abnormalities and groin hernias in elementary-school children in Aqaba: an epidemiological study. EMHJ Eastern Mediterranean Health J 18(2):119–126
Ravikumar V, Rajshankar S, Kumar HR, MR NG, (2013) A clinical study on the management of inguinal hernias in children on the general surgical practice. JCDR 7(1):144
Lao OB, Fitzgibbons RJ, Cusick RA (2012) Pediatric inguinal hernias, hydroceles, and undescended testicles. Surg Clin North Am 92(3):487
Tanyel FC, Öcal T, Karaağaoğlu E, Büyükpamukçu N (2000) Individual and associated effects of length of inguinal canal and caliber of the sac on clinical outcome in children. J Pediatr Surg 35(8):1165–1169
Krausz C, Quintana-Murci L, Fellous M, Siffroi JP, McElreavey K (2000) Absence of mutations involving the INSL3 gene in human idiopathic cryptorchidism. Mol Hum Reprod 6(4):298–302
Zvizdic Z, Milisic E, Halimic A, Zvizdic D, Zubovic SV (2014) Testicular volume and testicular atrophy index as predictors of functionality of unilaterally cryptorchid testis. Med Arch 68(2):79
Niedzielski J, Pisarska K, Przeratil P (2003) The usefulness of testicular atrophy index in the assessment of undescended testicle–preliminary report. Rocz Akad Med Bialymst 48(112):4
Funding
There were no grants or fellowships supporting the writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abou EL-Ella, S.S., Tawfik, M.A., Abd El-Aziz, T.F. et al. The G178A polymorphic variant of INSL3 may be linked to cryptorchidism among Egyptian pediatric cohort. Pediatr Surg Int 36, 1387–1393 (2020). https://doi.org/10.1007/s00383-020-04735-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04735-8