Abstract
The value of laryngotracheobronchoscopy (LTB) immediately prior to repair of esophageal atresia with or without tracheo-esophageal fistula is contentious. Currently, there is a wide range of opinion on the utility of this investigation which is reflected by huge variation in clinical practice. This review is a critical analysis of the arguments for and against performing routine LTB prior to esophageal atresia repair. Reserving LTB for selected cases only is potentially disadvantageous since it limits the surgeon’s and anesthetist’s familiarity with the procedure, equipment, and range of potential findings. There is sufficient evidence to suggest that routine preoperative LTB becomes the standard of care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
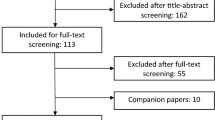
The utility of laryngotracheobronchoscopy (LTB) immediately prior to repair of esophageal atresia (EA) with or without tracheo-esophageal fistula (TEF) is contentious. Contemporary international surveys have highlighted how variably this investigation is performed in clinical practice. A recent survey of 170 IPEG members from 31 countries found that LTB was routinely undertaken by 60% of pediatric surgeons, selectively by 13%, and never by 27% [1]. Another survey of 178 delegates at the EUPSA-BAPS 2012 Congress found that 56% do not perform routine preoperative endoscopy [2]. A prospective French national registry of EA showed a preoperative LTB rate of just 22% [3] and retrospective multicenter studies from Australasia and the USA recorded figures of 41 and 66%, respectively, with huge variations in rates between individual institutions [4, 5]. Given this wide variation in clinical practice, we decided to review the arguments for and against performing routine LTB prior to repair of EA.
The case for routine preoperative laryngotracheobronchoscopy
Laryngotracheobronchoscopy preceding repair of EA ± TEF has two main functions: (1) to characterize the number and site of TEF, and (2) to identify co-existing anomalies.
-
1.
The number and site of tracheo-esophageal fistula(e)
Upper pouch fistula The common anatomical varieties of EA ± TEF and their relative frequencies derived from six published series totaling more than 2200 cases [6,7,8,9,10,11] are shown in Fig. 1. Given this distribution, some experts have argued for selective use of LTB, reserving it for cases where the incidence of an upper pouch fistula is proportionately greater [12]. Considering Fig. 1, the number needed to ‘treat’ (NNT) to identify an upper pouch fistula increases from approximately 60 when distal gas is present on a plain radiograph to 11 when there is no distal gas. This logic assumes that all upper pouch fistulae in these collected series were eventually detected but we know that an upper pouch fistula may rarely be detected for the first time in adolescence or early adulthood [13, 14]. In addition, some centers have reported a higher incidence of upper pouch fistula with EA/TEF [15]. Smaller individual institutional experiences estimate that the NNT to define an upper pouch fistula in the context of absent distal gas may be less [16], even as low as 5 [17], 3 [18] or 2 [19, 20]. In one center, the detection of an upper pouch fistula was statistically significantly improved following the introduction of routine tracheobronchoscopy [20]. However, it must be acknowledged that an upper pouch fistulae may be missed on LTB. When present, it may only be visible as a small pit just distal to the vocal cords that does not necessarily open and close with ventilation; concomitant insufflation of the esophagus whilst observing the pit can be helpful [21, 22].
Fig. 1 Major anatomical configurations of esophageal atresia and tracheo-esophageal fistula and their frequencies. According to these figures, if gas is visible on a plain abdominal radiograph in an infant with EA 98.4% will have EA + distal TEF and 1.6% will have EA + distal TEF + upper pouch fistula. If the abdomen is gasless 90.7% will have isolated EA and 9.3% EA + proximal TEF
Distal tracheo-esophageal fistula It is commonly assumed that a gasless abdomen equates to absence of a distal fistula, whereas in reality up to 15% of such patients have a distal fistula that is either very small or occluded by a mucous plug [23, 24]. In one series, 3 of 11 patients with suspected pure EA were found to have a distal TEF at tracheobronchoscopy [16].
Establishing the site of entry of the fistula into the tracheobronchial tree is useful for both the anesthetist and surgeon. It may modify the positioning of the endotracheal tube and the surgical approach [25,26,27]. Awareness of the likely anatomy of the TEF prior to surgery may facilitate esophageal dissection [26] or prepare the surgeon for dealing with a potential long gap [28]; the latter is arguably even more important when selecting patients for thoracoscopic repair. Of 149 patients with EA assessed by bronchoscopy in one series, the location of the fistula was as follows: 1% bronchial, 9% carinal (Fig. 2), 23% within 1 cm proximal to the carina, 59% mid-tracheal, and 8% cervical [14]. Some surgeons consider that the area of transmitted pulsation at LTB can predict the side of the aortic arch [26] which could influence the operative approach to repair of the EA/TEF. However, the reliability of this observation has not been critically evaluated.
Fig. 2 Tracheobronchoscopy also enables the size of a distal TEF to be assessed which may assist with airway management by indicating the potential likelihood of intubating the fistula. Visualizing the TEF may also facilitate selective intubation beyond the fistula [29] or enable temporary placement of a Fogarty balloon catheter to occlude the fistula [18, 30] to control an air leak through it (especially important in infants with respiratory distress and EA/TEF) [25].
Misdiagnosis of EA/TEF There are rare reports of iatrogenic neonatal pharyngoesophageal perforation where the abnormal passage of a naso/orogastric tube causes diagnostic confusion with EA/TEF [31, 32]. There are usually clinical and radiographic clues but some infants have been subjected to needless thoracotomy for presumed EA/TEF [31, 33]. Preliminary LTB would confirm the absence of a TEF in such cases.
Multiple TEF There are rare cases of three fistulae connecting the trachea to the esophagus [34]. A detailed preliminary LTB provides no guarantee that all three fistulae would be identified at the outset of treatment but it may alert the surgeon to unusual anatomy.
-
2.
Co-existing airway pathology
Potentially important co-existing airway anomalies can be diagnosed by preliminary LTB. In one consecutive series of 88 neonates with EA ± TEF who underwent LTB, there were 2 (2.3%) with a laryngeal cleft, one of which was significant [16]. In series where preliminary LTB was not routinely undertaken, laryngeal clefts have been subsequently detected in 0.5–1.4% of cases [8, 35, 36]. While it can be argued that type 1 clefts are often not clinically significant and failure to make the diagnosis is not harmful, some patients with EA have a more severe laryngeal cleft and are at risk of repeated pulmonary aspiration [8, 35,36,37].
Other rare congenital airway problems diagnosed by LTB include congenital subglottic stenosis [16, 17], vallecular cyst [16], and tracheal and/or bronchial stenosis [14, 17, 18, 26, 38,39,40].
Tracheomalacia is a clinically significant comorbidity in 5–20% of children with EA/TEF, although it is present to a variable degree in most affected children because of a developmental deficiency in the tracheal cartilaginous rings [41]. Tracheomalacia is usually diagnosed on tracheobronchoscopy by observing anteroposterior narrowing or collapse of the tracheal lumen associated with anterior ballooning of the widened posterior membranous tracheal wall on expiration during spontaneous ventilation [42]. Tracheomalacia tends to worsen during the first few months of life and findings on preoperative LTB at the time of EA/TEF repair correlate poorly with later development of clinically significant tracheomalacia [43]. Consequently, preoperative LTB adds little to the evaluation of this particular airway problem.
Unilateral or bilateral symptomatic vocal cord paresis or paralysis is reported in 3–5% of infants after EA ± TEF repair [4, 44, 45]. The true prevalence of vocal cord palsy may well be higher because symptoms can be mistakenly attributed to laryngotracheomalacia or gastroesophageal reflux [45]. Vocal cord palsy contributes to respiratory morbidity through impaired airway protection, aspiration pneumonia, and failed extubation. It is not yet clear whether vocal cord palsy associated with EA is predominantly congenital or iatrogenic but the latter is more likely since it appears to be more common after extensive upper pouch mobilization [45] and possibly after thoracoscopic EA/TEF repair [46]. However, abnormal development of the vagus nerve and recurrent laryngeal nerve branching pattern have been demonstrated in an experimental animal model of EA/TEF [47]. Prospective evaluation of vocal cord function prior to EA ± TEF repair should help determine the relative contributions of congenital and acquired pathology.
The case against routine preoperative laryngotracheobronchoscopy
-
1.
Logistics
Although it has been stated that the additional procedural time of performing LTB is “minimal”[18] or “a few minutes”[48], this depends in part on the familiarity of the pediatric surgeon and anesthetist with the procedure. Laryngotracheobronchoscopy can be performed using a variety of techniques and equipment which must be tailored to the size and stability of the infant. A rigid ventilating neonatal bronchoscope is most often used since this allows positive pressure ventilation and, if required, can be used to pass a Fogarty catheter into the fistula. Alternatively, flexible fiberoptic bronchoscopy can be used; this is usually performed while maintaining spontaneous ventilation [18] and each endoscopic assessment is limited to about 30–45 s [49]. There are numerous techniques including passing a 2.2-mm fibreoptic bronchoscope down a 3-mm ETT whilst maintaining continuous positive pressure ventilation [48] or using a small rod lens without the outer ventilating sheath [50]. The choice of equipment is dictated by tracheal size, the aims of the procedure (diagnostic or therapeutic), anesthetic expertise, availability of equipment, and surgeon preference. Traditionally, fiberoptic scopes of 2.2 mm [51] (or 2.5 mm with a working channel) or even smaller diameter [52] have been used, but 2.8 mm and 3.7 mm videoscopes (the latter with a working channel) with improved image resolution are now available. LTB has been performed in neonates with EA ± TEF as small as 1.3 kg [18, 48].
It is beyond the scope of this article to discuss the relative merits and limitations of other methods used to characterize the anatomy of EA ± TEF preoperatively including contrast studies, ultrasound scans, cross-sectional imaging, and esophagoscopy. These have been reviewed elsewhere [49] and currently do not provide the diagnostic accuracy [19, 20] or versatility afforded by LTB, although they may be complementary investigations.
-
2.
Risks
Complications of neonatal bronchoscopy are uncommon but include moderate/transient desaturation, laryngospasm, apnoea, bradycardia, inadvertent extubation, and airway trauma [51, 53, 54].
-
3.
Other arguments
Various arguments against routine preoperative LTB have been put forward: when distal gas is present on a plain radiograph in an infant with EA up to 60 such infants need to be examined to identify an upper pouch fistula, raising questions of validity and cost-effectiveness; in the presence of a gasless abdomen and apparently isolated EA, if a distal TEF is present it will still be found at operation; prompt surgical control of the fistula rather than attempted endoscopic occlusion is the best option in infants with respiratory distress and EA/TEF [55]; an upper pouch fistula can still be missed despite careful LTB and a negative examination might provide false reassurance [21, 22]; most laryngeal clefts associated with EA are type 1 and clinically insignificant while more severe varieties will be identified because of symptoms (as will other rare major airway anomalies); tracheomalacia is an evolving condition that cannot be adequately assessed by early LTB; and vocal cord paresis is predominantly iatrogenic and therefore documenting vocal cord function preoperatively is not particularly helpful.
Conclusions
Robust arguments can be developed for and against routine preoperative LTB prior to repair of EA ± TEF. Despite numerous publications supporting the value of this investigation, pediatric surgeons remain divided about its role in clinical practice. Reserving LTB for selected cases only is potentially disadvantageous since it limits both the surgeon’s and anesthetist’s familiarity with the procedure, equipment, and range of potential findings. Perhaps it is time to recommend that routine preoperative LTB becomes the standard of care.
References
Lal D, Miyano G, Juang D, Sharp NE, St. Peter SD (2013) Current patterns of practice and technique in the repair of esophageal atresia and tracheoesophageal fistua: an IPEG survey. J Laparoendosc Adv Surg Tech 23(7):635–638
Zani A, Eaton S, Hoellwarth ME, Puri P, Tovar J, Fasching G, Bagolan P, Lukac M, Wijnen R, Kuebler JF (2014) International survey on the management of esophageal atresia. Eur J Pediatr Surg 24(01):003–008
Sfeir R, Bonnard A, Khen-Dunlop N, Auber F, Gelas T, Michaud L, Podevin G, Breton A, Fouquet V, Piolat C (2013) Esophageal atresia: data from a national cohort. J Pediatr Surg 48(8):1664–1669
Lal DR, Gadepalli SK, Downard CD, Ostlie DJ, Minneci PC, Swedler RM, Chelius T, Cassidy L, Rapp CT, Deans KJ (2017) Perioperative management and outcomes of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 52(8):1245–1251
Knottenbelt G, Costi D, Stephens P, Beringer R, Davidson A (2012) An audit of anesthetic management and complications of tracheo-esophageal fistula and esophageal atresia repair. Pediatric Anesthesia 22(3):268–274
Beasley S, Shann F, Myers N, Auldist A (1989) Developments in the management of oesophageal atresia and tracheo-oesophageal fistulas. Med J Aust 150(9):501–503
Engum SA, Grosfeld JL, West KW, Rescorla FJ, Scherer LT (1995) Analysis of morbidity and mortality in 227 cases of esophageal atresia and/or tracheoesophageal fistula over two decades. Arch Surg 130(5):502–508
Louhimo I, Lindahl H (1983) Esophageal atresia: primary results of 500 consecutively treated patients. J Pediatr Surg 18(3):217–229
Manning PB, Morgan RA, Coran AG, Wesley JR, Polley TZ Jr, Behrendt DM, Kirsh MM, Sloan HE (1986) Fifty years’ experience with esophageal atresia and tracheoesophageal fistula. Beginning with Cameron Haight’s first operation in 1935. Ann Surg 204(4):446
Randolph JG (1986) Esophageal atresia and congenital stenosis - Esophageal atresia and associated malformations, including laryngotracheoesophageal cleft. In: Welch, Mea (eds) Pediatric surgery, vol 1, 4th edn. Year Book Medical, Chicago, pp 682–684
Spitz L, Kiely E, Morecroft J, Drake D (1994) Oesophageal atresia: at-risk groups for the 1990s. J Pediatr Surg 29(6):723–725
Spitz L (2006) Esophageal atresia: lessons I have learned in a 40-year experience. J Pediatr Surg 41(10):1635–1640
Chiou E, Ongkasuwan J (2014) Delayed identification of proximal tracheoesophageal fistula. J Pediatr Gastroenterol Nutr 58(5):e45
Holzki J (1992) Bronchoscopic findings and treatment in congenital tracheo-oesophageal fistula. Paediatr Anaesth 2(4):297–303
Dudgeon DL, Morrison CW, Woolley MM (1972) Congenital proximal tracheoesophageal fistula. J Pediatr Surg 7(5):614–619
Sharma N, Srinivas M (2014) Laryngotracheobronchoscopy prior to esophageal atresia and tracheoesophageal fistula repair—its use and importance. J Pediatr Surg 49(2):367–369
Pigna A, Gentili A, Landuzzi V, Lima M, Baroncini S (2001) Bronchoscopy in newborns with esophageal atresia. Pediatr Med Chir 24(4):297–301
Atzori P, Iacobelli BD, Bottero S, Spirydakis J, Laviani R, Trucchi A, Braguglia A, Bagolan P (2006) Preoperative tracheobronchoscopy in newborns with esophageal atresia: does it matter? J Pediatr Surg 41(6):1054–1057
Bax KNM, Roskott AMC, van der Zee DC (2008) Esophageal atresia without distal tracheoesophageal fistula: high incidence of proximal fistula. J Pediatr Surg 43(3):522–525
Parolini F, Morandi A, Macchini F, Canazza L, Torricelli M, Zanini A, Leva E (2013) Esophageal atresia with proximal tracheoesophageal fistula: a missed diagnosis. J Pediatr Surg 48(6):e13–e17
Shoshany G, Vatzian A, Ilivitzki A, Smolkin T, Hakim F, Makhoul IR (2009) Near-missed upper tracheoesophageal fistula in esophageal atresia. Eur J Pediatr 168(10):1281–1284
Summerour V, Stevens PS, Lander AD, Singh M, Soccorso G, Arul GS (2017) Characterization of the upper pouch tracheo–oesophageal fistula in oesophageal atresia. J Pediatr Surg 52(2):231–234
Goh D, Brereton R, Spitz L (1991) Esophageal atresia with obstructed tracheoesophageal fistula and gasless abdomen. J Pediatr Surg 26(2):160–162
Kluth D (1976) Atlas of esophageal atresia. J Pediatr Surg 11(6):901–919
Filston H, Rankin J, Grimm J (1984) Prognostic factors and contribution of preoperative telescopic endoscopy. Esophageal atresia. Ann Surg 199:532–536
Kosloske AM, Jewell PF, Cartwright KC (1988) Crucial bronchoscopic findings in esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 23(5):466–470
Alabbad SI, Shaw K, Puligandla PS, Carranza R, Bernard C, Laberge J-M (2009) The pitfalls of endotracheal intubation beyond the fistula in babies with type C esophageal atresia. Semin Pediatr Surg 18(2):116–118
Holcomb GW (2017) Thoracoscopic surgery for esophageal atresia. Pediatr Surg Int 33(4):475–481
Broemling N, Campbell F (2011) Anesthetic management of congenital tracheoesophageal fistula. Pediatr Anesthesia 21(11):1092–1099
Andropoulos D, Rowe R, Betts J (1998) Anaesthetic and surgical airway management during tracheo-oesophageal fistula repair. Pediatr Anesthesia 8(4):313–319
Krasna IH, Rosenfeld D, Benjamin BG, Klein G, Hiatt M, Hegyi T (1987) Esophageal perforation in the neonate: an emerging problem in the newborn nursery. J Pediatr Surg 22(8):784–790
Blair G, Filler R, Theodorescu D (1987) Neonatal pharyngoesophageal perforation mimicking esophageal atresia: clues to diagnosis. J Pediatr Surg 22(8):770–774
Kassner E, Baumstark A, Balsam D, Haller J (1977) Passage of feeding catheters into the pleural space: a radiographic sign of trauma to the pharynx and esophagus in the newborn. Am J Roentgenol 128(1):19–22
Kane TD, Atri P, Potoka DA (2007) Triple fistula: management of a double tracheoesophageal fistula with a third H-type proximal fistula. J Pediatr Surg 42(6):e1-e3
Spitz L, Kiely E, Brereton R (1987) Esophageal atresia: five year experience with 148 cases. J Pediatr Surg 22(2):103–108
Hseu A, Recko T, Jennings R, Nuss R (2015) Upper airway anomalies in congenital tracheoesophageal fistula and esophageal atresia patients. Ann Otol Rhinol Laryngol 124(10):808–813
Fraga JC, Adil EA, Kacprowicz A, Skinner ML, Jennings R, Lillehei C, Rahbar R (2015) The association between laryngeal cleft and tracheoesophageal fistula: myth or reality? Laryngoscope 125(2):469–474
Alfery DD, Ward C, Plumer MH, Lynch F (1980) Management of tracheal atresia with tracheoesophageal fistula. J Am Soc Anesthesiol 53(3):242–243
Bray R, Lamb W (1988) Tracheal stenosis or agenesis in association with tracheo-oesophageal fistula and oesophageal atresia. Anaesthesia 43(8):654–658
Loeff D, Filler R, Vinograd I, Ein S, Williams W, Smith C, Bahoric A (1988) Congenital tracheal stenosis: a review of 22 patients from 1965 to 1987. J Pediatr Surg 23(8):744–748
Wailoo M, Emery J (1979) The trachea in children with tracheo-oesophageal fistula. Histopathology 3(4):329–338
Benjamin B (1981) Endoscopy in esophageal atresia and tracheoesophageal fistula. Annals of Otology. Rhinol Laryngol 90(4):376–382
Dodge-Khatami A, Deanovic D, Sacher P, Weiss M, Gerber A (2006) Clinically relevant tracheomalacia after repair of esophageal atresia: the role of minimal intra-operative dissection and timing for aortopexy. Thorac Cardiovasc Surg 54(03):178–181
Mortellaro V, Pettiford J, St Peter S, Fraser J, Ho B, Wei J (2011) Incidence, diagnosis, and outcomes of vocal fold immobility after esophageal atresia (EA) and/or tracheoesophageal fistula (TEF) repair. Eur J Pediatr Surg 21(06):386–388
Morini F, Iacobelli BD, Crocoli A, Bottero S, Trozzi M, Conforti A, Bagolan P (2011) Symptomatic vocal cord paresis/paralysis in infants operated on for esophageal atresia and/or tracheo-esophageal fistula. J Pediatr 158(6):973–976
Woo S, Lau S, Yoo E, Shaul D, Sydorak R (2015) Thoracoscopic versus open repair of tracheoesophageal fistulas and rates of vocal cord paresis. J Pediatr Surg 50(12):2016–2018
Qi BQ, Merei J, Farmer P, Hasthorpe S, Myers NA, Beasley SW, Hutson JM (1997) The vagus and recurrent laryngeal nerves in the rodent experimental model of esophageal atresia. J Pediatr Surg 32(11):1580–1586
De Gabriele L, Cooper M, Singh S, Pitkin J (2001) Intraoperative fibreoptic bronchoscopy during neonatal tracheo-oesophageal fistula ligation and oesophageal atresia repair. Anaesth Intensive Care 29(3):284
Parolini F, Boroni G, Stefini S, Agapiti C, Bazzana T, Alberti D (2014) Role of preoperative tracheobronchoscopy in newborns with esophageal atresia: A review. World J Gastrointest Endosc 6(10):482
Veyckemans F, Hamoir M, Rombaux P, Van Obbergh LJ, Reding R (2002) Preoperative tracheoscopy in neonates with esophageal atresia. Anesthesia Analgesia 95(6):1827–1828
Midulla F, De Blic J, Barbato A, Bush A, Eber E, Kotecha S, Haxby E, Moretti C, Pohunek P, Ratjen F (2003) Flexible endoscopy of paediatric airways. Eur Respir J 22(4):698–708
Nussbaum E (2002) Pediatric fiberoptic bronchoscopy: clinical experience with 2,836 bronchoscopies. Pediatr Crit Care Med 3(2):171–176
Deanovic D, Gerber AC, Dodge-Khatami A, Dillier CM, Meuli M, Weiss M (2007) Tracheoscopy assisted repair of tracheo-esophageal fistula (TARTEF): a 10-year experience. Pediatr Anesthesia 17(6):557–562
De Blic J, Marchac V, Scheinmann P (2002) Complications of flexible bronchoscopy in children: prospective study of 1,328 procedures. Eur Respir J 20(5):1271–1276
Templeton JM, Templeton JJ, Schnaufer L, Bishop HC, Ziegler MM, O’Neill JA (1985) Management of esophageal atresia and tracheoesophageal fistula in the neonate with severe respiratory distress syndrome. J Pediatr Surg 20(4):394–397
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no competing interest.
Rights and permissions
About this article
Cite this article
Taghavi, K., Stringer, M.D. Preoperative laryngotracheobronchoscopy in infants with esophageal atresia: why is it not routine?. Pediatr Surg Int 34, 3–7 (2018). https://doi.org/10.1007/s00383-017-4194-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-017-4194-0