Abstract
Purpose
Port removal is usually a straightforward procedure delegated to trainees. However, some port removals are complicated by central venous catheter (CVC) fragmentation, a challenge for even experienced surgeons. This study aimed to determine the incidence of, and risk factors for, complicated port removal in children.
Methods
A single-centre study assessed the outcome of removal for all paediatric ports inserted from 1996 to 2012. Data were recorded detailing patient, insertion, device and removal characteristics. Risk factors for complicated removals were scrutinised using Chi-square tests; p < 0.05 significant.
Results
Of 628 ports inserted from 1996 to 2012, 443 were subsequently removed at the same centre. 8/443 (1.8 %) removals were complicated by CVC fragmentation, a median of 3.3 (2.4–3.9) years after insertion. Of complicated cases, 8/8 underwent formal neck dissection, 3/8 intravascular dissection, and 1/8 endovascular retrieval. 2/8 cases have retained intravascular CVC fragments. Risk factors for complication were CVC caliber <6Fr (p < 0.001) and use duration >2 years (p < 0.001).
Conclusion
Greatest care and senior supervision should be ensured when removing ports with CVC caliber <6Fr and/or >2 years since insertion. However, complications also occur with larger CVCs or after shorter durations. Therefore, the key to avoiding complicated port removal may simply be: preparation, preparation, neck preparation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vascular access port removal is usually a straightforward procedure delegated to more junior trainees. However, a minority of port removals are complicated by central venous catheter (CVC) deterioration and/or fragmentation. This complication can quickly lead to a procedure of great challenge for even experienced surgeons. Despite extensive literature addressing the acute and long-term complications of vascular access port insertion and use [1–3], relatively few studies have considered specifically the intraoperative complications of port removal [4–6]. Several related reports have focused on the implications and management of retained CVC fragments, albeit without clear indications as to the antecedents of such fragmentation [6–10]. The primary aim of this study was to determine the incidence of port removals complicated by intraoperative CVC fragmentation. Further, we aimed to inform future management by identifying risk factors for intraoperative CVC fragmentation in our paediatric population.
Methods
Study population
All paediatric (aged 0–18 years) patients undergoing vascular access port insertion at the Royal Hospital for Sick Children (Edinburgh, UK) between 1996 and 2012 were assessed for the outcome of any subsequent port removal procedure. Port removal cases between 1996 and 2014 were included. Cases were identified by retrospective analysis of two independent, prospectively maintained institutional databases: the Royal Hospital for Sick Children Lines Database and Lothian Surgical Audit Database. The Royal Hospital for Sick Children Lines Database is a dedicated database established in 1996 to provide data for various aspects of central vascular access procedures. Data are entered prospectively at insertion and removal detailing patient, insertion and device characteristics. For the purpose of this study, missing data were retrieved wherever possible by retrospective review of other contemporaneous sources, i.e. case note review and operating theatre prosthesis ledgers.
Complicated vascular access port removals
For this study, ‘complicated vascular access port removal’ was defined as that in which deterioration or fragmentation necessitated additional intervention, e.g. formal neck dissection, other second procedure or interventional radiology. Cases of complicated port removal were recorded at occurrence. Putative risk factors for complicated removal were identified by review of the relevant literature [1, 6, 7, 11, 12], together with superadded examination of index cases.
Ethical standards
This project was assessed by the South East Scotland Research Ethics Service and deemed to not need NHS ethical review under the terms of the UK Health Department’s Governance Arrangements for Research Ethics Committees (A Harmonised Edition), 2011.
Statistical analysis
Two tailed Chi-square tests were performed to assess for associations between complicated port removal and putative risk factors; p values less than 0.05 were considered significant. Risk factors included patient, insertion and device characteristics. Cases whose data for a given risk factor were missing were excluded from that particular analysis, but included in risk factor analyses if the data relevant to that factor were complete. Exclusion of cases with missing data in this fashion is a conventional statistical technique termed ‘pairwise deletion’ [13].
Results
Study population
Between 1996 and 2012, 628 vascular access ports were inserted at the Royal Hospital for Sick Children (Edinburgh, UK). 443 of these 628 ports were also removed at this same centre prior to the completion of data collection at the end of 2014. An additional 8 removals are known to have been performed at other hospitals, albeit these cases were excluded due to lack of access to outcome data. Insertion side, insertion vein, site for placement of port, device characteristics including lumen number and caliber, and duration of port use at the time of removal are shown in Table 1. Of the remaining 177 ports for which no removal procedure was recorded: 75 patients died prior to removal, 46 were documented as remaining in use, and 56 were considered lost to follow-up at the completion of the study period. This equates to 9 % of the original cohort being potentially lost to follow-up.
Incidence of complicated vascular access port removals
8 of 443 (1.8 %) vascular access port removals were complicated by intraoperative CVC fragmentation with need for additional intervention. 7 of 8 complicated port removals were performed following completion of oncology treatment, and 1 port required removal for refractory CVC colonisation. Median duration of port use at time of complicated removal was 3.3 (2.4–3.9) years. This was calculated to equate to 1 complicated removal per 33,507 catheter days for the study cohort. Further details of the 8 complicated cases are provided in Table 2.
Management of complicated vascular access port removals
Formal neck dissection through a second incision was undertaken in all 8 cases of complicated port removal. This dissection progressed to include, intravascular dissection in 3 of the 8 cases. A fourth case was ultimately transferred to another hospital for endovascular retrieval of a distal CVC fragment. Intravascular CVC fragments were retained in situ in 2 of the 8 cases, and to date no further complications have arisen attributed to these retained fragments. The surgical management of each of the 8 cases is summarised in Table 2.
Assessment of catheters from complicated vascular access port removal cases
All catheters from complicated removals were returned to the relevant manufacturers for assessment, but none were identified to have manufacturing faults. Histology demonstrated the catheters’ roughened surface to be due to micro-calcification, often with an associated and tightly applied fibrous sheath. It was speculated these histologic changes represented a foreign body reaction due to the catheter.
Risk factors for complicated vascular access port removals
No patient or insertion characteristics were associated with increased risk of complicated port removal; Table 1. Two device characteristics were associated with significantly increased risk of complicated removal, namely CVC caliber less than 6 French (<6Fr: 5/48 vs 6 to <9Fr: 2/239 vs ≥9Fr: 0/87; p < 0.001) and duration of use more than 2 years (≤2 years: 0/299 vs >2 years: 8/144; p < 0.001). However, neither brand (Arrow: 6/244 vs Bard: 0/73 vs pfm medical cpp: 1/27 vs other: 0/17; p = 0.46) nor lumen number (single: 7/327 vs double: 0/56; p = 0.27) was found to be a significant risk factor. See Table 1 for full details of putative risk factor analysis, including the distribution of missing data (i.e. ‘not recorded’).
Discussion
This large, single-centre study of children requiring long-term vascular access confirms complicated vascular access port removal is uncommon, but by no means rare.
We consider the 1.8 % incidence of complicated removal to be accurate in this paediatric population, and comparable with two other large series reporting a similar incidence of 2 % [5, 6]. Wilson et al. (2006), however, reported a much higher incidence of complicated port removals (32 of 200, 16 %). These authors attributed their remarkably high rate of complication port removal to use of polyurethane rather than silicon-based CVCs [4]. Polyurethane catheters are suggested to be more prone to complicated removal due to increased intravascular adherence and microfractures [4, 14]. Our study did not specifically record the catheter material used. However, retrospectively applied brand product specifications indicate the vast majority of CVCs were silicon-based, including 7 of our 8 complicated cases. Thus, although differences in CVC material may reconcile the discrepancy between reported incidences of complications, we and others show complicated port removals still occur with silicon-based CVCs [14].
Previous case series report that the incidence of mechanical port complications varies according to insertion characteristics, such as choice of vein [1, 15] or port placement [12]. In the current series, the internal jugular vein was preferred, albeit vein choice was not associated with complicated port removal. Similarly, we observed no difference in complication rate according to placement of the port on the lateral vs anterior chest wall. Our findings are in agreement with those of Fallon et al. (2011), who reported no difference in mechanical or infection complications in adult oncology patients undergoing either anterior or lateral chest wall placement [11]. Some previous studies have ascribed risk of CVC fragmentation and complicated removal to a specific brand or device design [4, 6]. Whilst 6 complicated removals described in this series involved devices produced by arrow, this was also the most frequently used brand and there was no significant association with risk of complication. We scrutinised brand, lot and serial number identifiers for any trends, but found none.
This study identified two risk factors for complicated vascular access port removal: narrow caliber of the CVC (<6 French), and duration in situ exceeding 2 years. These findings are strikingly consistent with previous studies [4, 5, 7, 14]. However, our and other paediatric series show complications may also occur when removing larger caliber CVCs [1] or after lesser periods of time in situ [5, 9, 10]. Two cases in the current series involved fragmentation of an 8.4 French CVC. These exceptions notwithstanding, we recommend greatest care if removing ports more than 2 years duration in situ, or with narrow caliber CVCs.
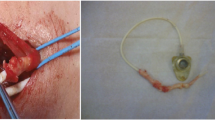
Given the limited sensitivity of such risk factors for complicated port removal, we advocate heightened surgical consideration, awareness and preparation for complicated vascular access port removal. Consideration: vascular access port removal is most often brief and uncomplicated, and so regularly delegated to more junior surgical staff with minimal supervision. However, this study highlights how children may be put at risk by failure to consider the possibility of complications when scheduling, delegating and supervising cases. We and others [5] advocate the immediate availability of senior surgical staff to assist, supervise and if appropriate assume the role of operating surgeon should CVC fragmentation occur or be considered at high risk. Awareness: Wilson et al. [4] described characteristic CVC deterioration as a precursor to fragmentation. We concur the findings of a discoloured and roughened CVC (see Fig. 1) is a ‘red flag’, which alerts the observant surgeon to the potential for complicated removal and allows action to limit the morbidity of fragmentation. Whilst such presumptive action may still take the form of neck dissection with or without intravascular dissection, these more challenging procedures may now be undertaken in controlled fashion with the appropriate assistance and resources. The option of retaining firmly adherent CVC fragments in situ is valid, and may prove prudent when compared with the potential morbidity of intravascular dissection [6–10]. Preparation: we advocate routine positioning and skin preparation of the neck in addition to the anterolateral chest to permit time-efficient transition to emergency neck dissection if required [5]. Undue delays could allow time for central migration of the proximal CVC fragment, resulting in superadded morbidity for the patient such as need for endovascular intervention.
Our study is subject to biases, most notably that of missing data. ‘Pairwise deletion’ has been used to limit the impact of this bias. Importantly, pairwise deletion is not considered prone to Type 1 errors [13]. In this study, a type 1 error would result in a variable being wrongly considered a risk factor, which is not associated with an increased risk of complicated vascular access port removal. Another limitation pertains to variables, which were not measured but may influence the outcome of port removal, e.g. skin preparation used at port insertion, indication for central venous access and the nature of solutions instilled per device [3, 4, 7, 10, 15].
Our recommendations echo those of other authors, who equate a lack of awareness of, and preparedness for, the challenges of complicated port removal with a failure of professional duty, including that of fully informed parental consent [5, 10]. Ours is, however, also a simple and achievable message, which will resonate with many: preparation, preparation, and neck preparation.
References
Dillon PA, Foglia RP (2006) Complications associated with an implantable vascular access device. J Pediatr Surg 41(9):1582–1587
Goossens GA, Stas M, Jerome M, Moons P (2011) Systematic review: malfunction of totally implantable venous access devices in cancer patients. Support Care Cancer 19(7):883–898
Kock HJ, Pietsch M, Krause U, Wilke H, Eigler FW (1998) Implantable vascular access systems: experience in 1500 patients with totally implanted central venous port systems. World J Surg 22(1):12–16
Wilson GJ, van Noesel MM, Hop WC, van de Ven C (2006) The catheter is stuck: complications experienced during removal of a totally implantable venous access device. A single-center study in 200 children. J Pediatr Surg 41 (10):1694–1698
Maizlin I, Carpentier H, Bliss D (2010) Difficult extraction of long-term central venous catheters in children—case report. J Pediatr Surg 45(8):1720–1723
Lin CH, Wu HS, Chan DC, Hsieh CB, Huang MH, Yu JC (2010) The mechanisms of failure of totally implantable central venous access system: analysis of 73 cases with fracture of catheter. Eur J Surg Oncol 36(1):100–103
Milbrandt K, Beaudry P, Anderson R, Jones S, Giacomantonio M, Sigalet D (2009) A multiinstitutional review of central venous line complications: retained intravascular fragments. J Pediatr Surg 44(5):972–976
Teeple EA, Shiels WE, Nwomeh BC, Rocourt DV, Caniano DA (2011) Difficult central venous access removal: case reports of the use of endovascular snare shearing of endothelialized tetherings. J Pediatr Surg 46(5):e13–e15
Lesher AP, Kratz JM, Smith CD (2008) Removal of embedded central venous catheters. J Pediatr Surg 43(6):1030–1034
Chan BK, Rupasinghe SN, Hennessey I, Peart I, Baillie CT (2013) Retained central venous lines (CVLs) after attempted removal: an 11-year series and literature review. J Pediatr Surg 48(9):1887–1891
Pardo I, Rager EL, Bowling MW, Fajardo A, Clare S, Goulet R Jr (2011) Central venous port placement: a comparison of axillary versus anterior chest wall placement. Ann Surg Oncol 18(2):468–471
Fallon SC, Larimer EL, Gwilliam NR, Nuchtern JG, Rodriguez JR, Lee TC, Lopez ME, Kim ES (2013) Increased complication rates associated with Port-a-Cath placement in pediatric patients: location matters. J Pediatr Surg 48(6):1263–1268
Allison PD (2001) Missing data. Sage, Thousand Oaks, Calif, London
Jones SA, Giacomantonio M (2003) A complication associated with central line removal in the pediatric population: retained fixed catheter fragments. J Pediatr Surg 38(4):594–596
Fratino G, Molinari AC, Parodi S, Longo S, Saracco P, Castagnola E, Haupt R (2005) Central venous catheter-related complications in children with oncological/hematological diseases: an observational study of 418 devices. Ann Oncol 16(4):648–654
Acknowledgments
The authors wish to acknowledge the children, families and surgeons whose cases are represented in this series.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This study was not supported by any grant bodies, scholarships or other financial support.
Ethical standards
As stated in the manuscript, this project was assessed by the South East Scotland Research Ethics Service and deemed to not need NHS ethical review under the terms of the UK Health Department’s Governance Arrangements for Research Ethics Committees (A Harmonised Edition), 2011.
Rights and permissions
About this article
Cite this article
Teague, W.J., Fouad, D., Munro, F.D. et al. Complicated vascular access port removals: incidence, antecedents and avoidance. Pediatr Surg Int 31, 859–864 (2015). https://doi.org/10.1007/s00383-015-3754-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3754-4