Abstract
Purpose
Severe chordee with hypospadias may require repair by ventral corporoplasty with a free graft before urethroplasty. We report an 11 year experience with one-stage and two-stage hypospadias repair using dermal grafts.
Materials and methods
From 12/1997 to 12/2008, 47 hypospadias with severe chordee were repaired using a ventral dermal graft to correct the chordee. Forty cases were repaired in two stages; the remaining seven patients had adequate preputial skin and were repaired in one stage. In 28 cases the neourethra was covered with both tunica vaginalis and penile dartos flap while 12 were covered only with penile dartos flap. Patients ranged from 12 to 152 months of age. Follow-up ranged from 6 months to 4 years.
Results
28 patients with both tunica vaginalis and dartos flap had 7 urethral fistulas and 2 developed meatal stenosis. 12 patients with only penile dartos flap had 3 fistulas and 2 had meatal regression. The seven patients who underwent a one-stage repair had good results with a straight penis and no evidence of urethral fistula or urethral stenosis.
Conclusions
Dermal graft can be performed in one or two stage hypospadias repair. Complication rates are similar to other standard repairs for proximal hypospadias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Penile chordee is often seen in proximal hypospadias, it occurs in about 10–15 % of patients [1]. Chordee release is the first priority in hypospadias repair and must be completed before urethroplasty. In severe cases, after degloving and removing the dysplastic spongiosum tissue, if the corporal body is still bent for more than 30 degrees, corporal augmentation is the most effective procedure to make the penis straight. Several materials have been used to augment the corporal length including dermis [2–7], tunica vaginalis (TV) [8–11] or small intestinal submucosa (SIS) [12–16]. In these circumstances, the hypospadias repair is usually undertaken in stages: the corporal augmentation and rotation of preputial flaps ventrally to prepare the urethral plate is performed in the first stage, and the urethroplasty is accomplished in the second stage. Corporal augmentation associated with urethroplasty in a single stage hypospadias repair have also been described by Hendren and Keating [3], Horton et al. [4], Braga et al. [11], Kajbafzadeh et al. [10] and recently of Castellan Miguel et al. [12].
The availability of SIS is extremely limited in developing countries. We have chosen to utilize a dermal graft for corporal augmentation while preserving the TV so that it is available for coverage of our urethroplasty to prevent fistula formation. We report our 11-year experience with one-stage and two-stage hypospadias repairs using dermal grafts with the tubularized preputial island flap (TPIF) in one stage repair.
Materials and methods
We reviewed the records of all patients from 11/1997 to 12/2008 who underwent surgery for proximal hypospadias with severe chordee. Those patients who required ventral corporoplasty were included. No testosterone was used. All cripple hypospadias was excluded.
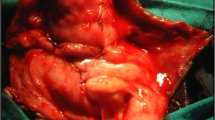
The procedure included degloving the penile skin and removing the fibrous tissue due to corpus spongiosum dysplasia. In cases with persistent angulation of the corporal body more than 30° (Fig. 1), the urethral plate was divided (Fig. 2). Following division of the urethral plate, if the chordee was still more than 15–20° [6], an incision was made along the ventral aspect on the tunica albuginea from 3 to 9 o’clock at the most angulated site. The dermal graft was harvested from an inguinal site [6]. We marked an elliptical shaped bed with a size roughly 15 × 30 mm to provide adequate dermal tissue. The bed should be colored with a marking pen so that after taking the epidermis away we could detect if there was any trace left. The dermis was then removed from the underlying tissue (Fig. 3). The graft was trimmed carefully to remove all fatty tissue and stored in saline solution. While the assistant closed the donor site, the surgeon performed again the artificial erection then incised the tunica albuginea tranversally from 3 o’clock to 9 o’clock at the maximal point of bending. Sew the graft into the defect of the tunica albuginea with 6.0 polyglactine in the quadrants and 7.0 polyglactine running suture to close the edges (Fig. 4). To check the effectiveness of the grafting, an artificial erection was performed again (Fig. 5). The tourniquet was taken down to assess for any leak in the anastomosis.
For the two-stage approach, a preputial flap was rotated ventrally to create the new urethral plate for the next stage. The second stage urethroplasty was performed at least 6 months later in either Thiersch–Duplay or Snodgrass technique. An artificial erection was performed at the beginning of the procedure to be sure that the chordee was completely corrected. Coverage of the urethroplasty with vascularized tissue was performed in all cases to prevent fistula formation. Only penile dartos tissue was used if there was a flap of adequate residual dartos large enough to cover the entire urethroplasty. If the dartos flap appeared to have poor vascularization or was too small a tunica vaginalis flap was used for primary coverage of the urethroplasty and any residual dartos tissue was laid on top of this. A drain was placed in the scrotum on the side where the tunica vaginalis was taken. We used either a penrose drain or a drain was fashioned from the cuff of a surgical glove. 7.0 polyglactine was used for urethroplasties. Urinary diversion was done with 8Fr or 10 Fr feeding tube from 10 to 14 days. Cefotaxime was used for all cases during urinary diversion.
A one-stage approach, performed only by senior surgeons (LTS, LCT, LTH), was utilized only after the surgeon ensured that the preputial flap had a robust blood supply and the TPIF was long enough to create a neourethra. This was then tubularized in a standard fashion over a feeding tube. The proximal end of the tube was anastomosed with interrupted suture to the native urethral meatus which was spatulated midline ventrally, creating an oval shape to prevent the stenosis afterwards. The vascular pedicle to the flap was advanced laterally over the neourethra to provide a barrier layer. The distal end of the preputial tube was sewn to the tip of the glans.
Results
Forty-seven patients with proximal hypospadias and severe congenital ventral curvature, composed of 5 perineal, 20 scrotal and 22 penoscrotal hypospadias, underwent treatment were included in our series. Patients ranged from 12 to 152 months of age, mean 74.2 months. Follow-up ranged from 6 months to 4 years with a mean of 12.2 months. Forty cases were repaired in two stages and the other seven in one stage. In the two-stage group, the artificial erection showed all chordee was corrected before the urethroplasty. The neourethra was covered with both tunica vaginalis and penile dartos flap in 28 patients. In the other 12, a dartos flap alone was felt to be adequate at the time of surgery. In the 28 patients with tunica vaginalis flap, 5 were drained with cuffs of surgical gloves, 23 others with penroses. All 5 cases drained with cuffs of surgical gloves had purulent infections that resulted in urethral fistulas, the 23 others with penroses had 2 fistulas without infection and 2 meatal stenosis. Among the 12 repairs that were covered only with penile dartos flap, 3 developed fistulas and 2 were found to have meatal regression. The fistulas and meatal regression were repaired 6 months to 1 year after. The two patients with meatal stenosis were treated with meatotomy. The seven patients with one stage repair had good results, no residual chordee, no urethral fistula or evidence of meatal stenosis. Surgical times took 3.5–4 h for a one-stage repair and about 3 h for the first stage of a two-stage repair.
All patients had a straight penis on erection postoperatively, but only 10 patients were followed up after puberty. The final assessment of erection was based on observation of parents or by patients at the follow up time at least 6 months after the urethroplasty.
Discussion
The systematic process of hypospadias repair is correcting chordee, then urethroplasty, creating the meatus at the tip of the penile glans and finally resurfacing the penis. This process is no different in a staged repair. In case of mild chordee, the dorsal plication or Nesbitt procedure may be used. If the chordee is more than 30°, the urethral plate is divided. If the curvature persists lesser than 30°, dorsal plication is usually indicated. If the curvature is still more than 30°, the best way to correct the chordee is to augment the ventral side of the corporal body with a free graft such as dermis, TV or SIS. The dorsal plication may shorten the penis, may be more prone to recurrent ventral curvature [17] or cause penile deformity in future [18]. Therefore, many surgeons will choose to lengthen the short side rather than shorten the long side, especially when the penis is short. Pope et al. [6] decided to use the graft at the ventral side even when the curvature was only from 15 to 20°. We support vigorously this point of view and apply this indication in our practice.
The use of a dermal graft for ventral lengthening was used first by Devine and Horton [2] and to date no complication related to the use of this graft has been reported [2–7, 18]. Two other free grafts are TV and SIS. Some authors who used the TV [7] and SIS [12, 13] recognized the efficacy and durability of the dermal graft and even consider the DG as the gold standard to recreate the corpus cavernosum [14]. Although one ply SIS is also a graft of choice [14, 16], SIS is not always available, especially in developing countries.
Caesar and Caldamone [7] had 60 % recurrence of chordee due to the shrinkage of the TV graft. Vandersteen [8] had the same in 3 cases. Kajbafzadeh et al. [10] had good result with 18 cases of TV graft. Richey and Ribbeck [9] who used 25 TV grafts had only one recurrence of chordee. Braga et al. [11] had 95 % success rate with TV flap alone in 23 cases.
Soergel et al. [13] had 4/12 cases of 4 ply SIS that resulted in shrinkage of grafts and they concluded that 4 ply SIS may not be an appropriate graft on the corporal body. Miguel Castellan et al. [12] had good results on 58 cases using 1 ply SIS. Among these, 43 were performed in two-stage repair and 15 in one stage. In the one-stage group with the TPIF for the urethroplasty, the neourethral meatus was left in the lower part of the glans in 8 and at the coronal sulcus in 7. Complications associated with the urethroplasty of the two-stage repair group were 11/43 including 3 urethrocutaneous fistulas, 3 urethral diverticulum, 2 meatal stenosis, 1 partial urethral dehiscence, 1 epidermal retention cyst and complications of the one-stage repair were 3 urethrocutaneous fistulas, 2 urethral diverticulum. In the series of Weiser with 1 ply SIS [14], he had one meatal stenosis and one subcoronal fistula in eight cases of two stages and one glans breakdown in one case of the one stage repair. Elmore et al. [16], using 4 ply SIS in 21 and 1 ply SIS in 7 patients, had 5 complications in 26 patients after stage 2 repair including epidermal retention cyst in 2 patients, partial urethral dehiscence in 2, urethral diverticulum in 1.
Corporal grafting with dermis to lengthen the ventral side of the penis associated with the urethroplasty using TPIF in a one-stage repair was first described by Horton et al. [4] in 3 cases without complication associated. In this report, the authors had also 20 cases of two-stage repair with 3 urethrocutaneous fistulas and 1 meatal stenosis. Hendren and Keating [3] corrected the chordee with dermal graft and performed the urethroplasty with bladder mucosa free graft in one stage in 10 patients. Kajbafzadeh performed the repair on his 16 patients in one stage with 1 urethrocutaneous fistula and 2 others in two stage with 1 meatal stenosis [10]. Hendren and Keating [3] said that the correction of chordee with DG and urethroplasty could be performed simultaneously, presumably because the DG obtained blood supply from the corpora cavernosa. They decided to repair in one stage on the basis of the quality of the penile skin. If, after degloving, the skin had enough dartos to cover the neourethra, they applied the two grafts simultaneously. Based on this, we performed the severe chordee hypospadias repair in one stage if the penile skin had a robust blood supply and was long enough for the neourethra.
In the treatment of proximal hypospadias, although a one-stage repair is preferable to avoid a second operation, a two-stage repair is still used. However, in the second stage, fistula is a frequent problem in a long urethroplasty without good vascular tissue to cover the urethroplasty. To reduce the fistula rate, we used the TV flap to cover the neourethra in 28 cases during their planned second stage urethroplasty. In our initial cases, we had 5 purulent infections in the scrotum due to ineffective drainage with the cuff of surgical glove, all leading to urethral fistulas. Following this experience, we began leaving a penrose drain in place for 5 days [19] to avoid this complication. With regards to meatal stenosis, we have found that we must incise the entire the glandular urethra after recognizing that the urethral dilatation alone failed and left the meatus at the coronal sulcus. We had a patient who did not belong to this study (proximal hypospadias repair without dermal graft) had the same complication with TV flap and we also performed the meatotomy. Since that time when we used the TV flap to wrap the neourethra, we covered the neourethra to coronal sulcus only.
Due to the high complication rate in the TPIF repair [20], a two-stage repair combined with corporal augmentation was performed on a majority of patients in recent reports, except in the papers by Kajbafzadeh [10] and Braga [11]. As described above in the methods, the patients who underwent a one-stage repair were selected carefully during the surgery based on the length of the neourethra and the vascularisation of the preputial flap. Thanks to the strict selection, complications were avoided in these patients. This good result is likely due to the fact that this is a different patient population from those who we felt required a two-stage repair. With experience, we feel that the complication rate of the two-stage repair may be further reduced, especially in using the TV flap to wrap the neourethra and the penrose to drain the scrotum instead of the cuffs of surgical gloves, while maintaining the strict selection criteria for patients who are candidates for a one-stage repair.
The disadvantage of the DG is that it is time consuming [12, 16]. We have found that this is not a real hindrance. We feel that the duration of time needed to perform the DG is not sufficient reason to avoid doing this procedure and the effort is worthwhile.
The limitation of this study is that the follow-up time is not long enough. Although in a recent study Badawy and Morsi [21] showed the good long term outcomes of DG, our results should be evaluated after puberty for all patients.
Conclusions
Dermal graft has demonstrated long-term efficacy for lengthening of the ventral corporal body for repair of severe chordee with hypospadias. Besides the staged repairs, in selected cases, a ventral dermal graft can be performed in one-stage hypospadias repair along with a tubularized preputial island flap. Complications of the repair are similar to those of other proximal hypospadias repairs.
References
John W. Duckett (2002) Operative pediatric urology. In: Frank JD, Gearhart JP, Snyder III HM (eds), 2nd edn. Harcourt Publishers Limited, pp 151–160
Devine CJ Jr, Horton CE (1975) Use of dermal graft to correct chordee. J Urol 113:56
Hendren Hardy, Keating Michael (1988) Use of dermal graft and free urethral graft in penile reconstruction. J Urol 140:1265–1269
Horton CE, Gearhart JP, Jeffs RD (1993) Dermal grafts for correction of severe chordee associated with hypospadias. J Urol 150:452–455
Lindgren BW, Reda EF, Levitt SB, Brock WA, Franco I (1998) Single and multiple dermal grafts for the management of severe penile curvature. J Urol 160:1128
Pope JC IV, Kropp BP, Mclauglin KP, Adams MC, Rink RC, Keating MA, Brock JW III (1996) Penile orthoplasty using dermal grafts in the outpatient setting. Urology 48:124–127
Caesar RE, Caldamone Anthony A (2000) The use of free grafts for correcting penile chordee. J Urol 146:1691–1693
Vandersteen DR, Husmann DA (1998) Late onset recurrent penile chordee after successful correction at hypospadias repair. J Urol 160:1131–1133
Michael L, Richey, Michaelene Ribbeck (2003) Successful use of tunica vaginalis grafts for treatment of severe chordee in children. J Urol 170:1574–1576
Kajbafzadeh AM, Hamid Arshadi, Payabvash S, Salmasi AH, Tousi VN, Sahebpor ARA (2007) Proximal hypospadias with severe chordee: single stage repair using corporeal tunica vaginalis free graft. J Urol 178:1036–1042
Braga LH, Pippi Salle JL, Dave S, Bagli DJ, Lorenzo AJ, Khoury AE (2007) Outcome analysis of severe chordee correction using tunica vaginalis as a flap in boys with proximal hypospadias. J Urol 178:1693
Miguel Castellan, Rafael Gosalbez, Joshi Devendra, Yuval Bar-Yosef, Andrew Labbie (2011) Ventral corporal body grafting for correcting severe penile curvature associated with single or two-stage hypospadias repair. J. Pediat Urol 7:289–293
Soergel TM, Cain MP, Kaffer M, Gitlin J, Casale AJ, Davis MM, Rink RC (2003) Complication of small intestinal submucosa for corporal body grafting for proximal hypospadias. J Urol 170:1577–1579
Weiser AC, Franco I, Herz DB, Silver RI, Reda EF (2003) Single layer small intestinal submucosa in the repair of severe chordee and complicated hypospadias. J Urol 170:1593–1595
Hayn MH, Bellinger MF, Schneck FX (2009) Small intestine submucosa as a corporal body graft in the repair of severe chordee. Urology 73(2):277–279
Elmore JM, Kirsch AJ, Scherz HC, Smith EA (2007) Small intestinal submucosa for corporal body grafting in severe hypospadias requiring division of the urethral plate. J Urol 178:1698–1701
Luis HP, Braga Armando J, Lorenzo Darius J, Bägli Sumit Dave, Eeg Kurt, Farhat Walid A, Pippi Salle João L, Khoury Antoine E (2008) Ventral penile lengthening versus dorsal plication for severe ventral curvature in children with proximal hypospadias. J Urol 180:1743–1748
Wilcox DT, Mouriquand PDE (2008) Hypospadias in essentials of pediatric urology. In: Thomas DFM, Duffy PG, Rickwood AMK (eds), 2nd edn. Informa Healthcare, pp 213–231
Chatterjee US, Mandal MK, Basu S, Das R, Majhi T (2004) Comparative study of dartos fascia and tunica vaginalis pedicle wrap for the tubularized incised plate in primary hypospadias repair. BJU Int 94:1102–1104
Wilcox DT, Snodgrass W (2006) Long-term outcome following hypospadias repair. World J Urol 24:240
Badawy H, Morsi H (2008) Long-term followup of dermal grafts for repair of severe penile curvature. J Urol 180(4 Suppl):1842–1845
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Son, L.T., Hung, L.T., Thang, L.C. et al. The use of dermal graft in severe chordee hypospadias repair: experience from Vietnam. Pediatr Surg Int 31, 291–295 (2015). https://doi.org/10.1007/s00383-015-3656-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3656-5