Abstract
Objective
Distraction enterogenesis may provide a novel therapy for short bowel syndrome (SBS). Previously described methods have relied upon isolated intestinal segments or transmural fixation. Our objective was to develop a novel, fully endoluminal device, permitting placement and removal through an enteral stoma or orifice.
Methods
A flexible device was designed consisting of two latex balloons mounted on coaxial catheters. The inner catheter allowed longitudinal force transmission from an external spring. Yorkshire pigs underwent jejunal Roux limb creation with device placement via jejunostomy. Balloons were inflated to 52 mmHg without significant reduction in bowel perfusion as measured by laser Doppler. The device was explanted after 7 days.
Results
Distracted bowel achieved an increase in length of 26.1 ± 6.1 % vs nondistracted fed bowel. As the device resided in unfed bowel, a 66.7 ± 14.5 % increase vs unfed bowel was noted. These corresponded to a gain of 6.3 ± 2.3 cm (0.9 ± 0.3 cm/day) and 12.9 ± 7.6 cm (1.8 ± 1.1 cm/day), respectively. Attachment sites demonstrated occasional epithelial sloughing with no balloon-associated perforation.
Conclusion
A novel double-balloon catheter device allows for fully endoluminal distraction enterogenesis. This approach may allow development of clinically applicable technology for the treatment of patients with SBS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Short bowel syndrome (SBS), the most common cause of pediatric intestinal failure, results from congenital or surgical loss of small bowel length, with insufficient remaining surface area to absorb nutrients required for growth and development [1]. Patient survival has been linked to the length of remaining small bowel [2], driving efforts to develop techniques of increasing intestinal length.
Surgical procedures to this end have been described [3–5], though these have been limited by surgical complications [6]. Small bowel transplantation has limited outcomes as well, with graft failure and rejection approaching 60 % at 5 years [7]. The mainstay of treatment, thus, remains supportive medical therapy with supplemental or total parenteral nutrition (TPN). TPN, or complete reliance on parenteral nutrition without feeding, is associated with complications such as metabolic derangements, catheter-related morbidity, and sepsis [1]. Thus, new treatments for SBS are needed.
Distraction enterogenesis, wherein linearly directed distractive mechanical force produces small intestinal elongation, may provide an effective option for increasing functional intestinal length in patients who face a poor prognosis of achieving enteral autonomy with medical treatment alone [8–10]. As we and others have previously shown, distraction enterogenesis produces significant, sustained intestinal lengthening with preservation of intestinal function [11–13]. This is characterized by mesenteric neovascularization, increased villus height and crypt depth, muscular hypertrophy, and increased epithelial cell proliferation [9, 14, 15].
A major limitation of prior techniques of distraction enterogenesis is the requirement of either creation of a blind-ending segment of intestine [8, 9] or the use of full-thickness sutures to allow transmission of mechanical force to the intestinal wall [16]. These techniques require an initial operation to either exclude the intestine to be lengthened or to place fixation sutures. This may introduce substantial risk in patients with SBS, who have been shown to develop a profound inflammatory response in elective intestinal surgery [17]. In addition, reoperation after distraction to restore intestinal continuity or to remove the device adds additional surgical morbidity, and may result in the loss of gained intestinal length in the creation of new anastomoses. For example, in a model requiring an isolated segment of intestine for a spring device, 39 % of gained length was lost upon restoration of intestinal continuity [18].
We aimed to create a device that could deliver longitudinal distractive force via reversible endoluminal attachments. This aim obviates the need for repeat operations for implantation and removal, and would no longer require surgical manipulation of the intestinal tract. A novel double-balloon catheter device successfully achieved endoluminal attachment and distraction. Safety of this approach and efficacy of enterogenesis were demonstrated in a well-established swine model.
Methods
Device design
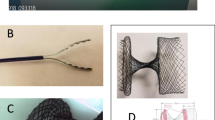
A dual-balloon catheter device was designed (MC3, Inc., Ann Arbor, MI) and manufactured (Vention Medical, South Plainfield, NJ) (Fig. 1a). An inner catheter and overtube were made of thermoplastic polyurethane. Compliant latex balloons were bonded onto the end of the overtube (proximal balloon) and the inner catheter (distal balloon). A stainless steel wire braid was incorporated into the overtube to prevent kinking. The inner catheter contained a nitinol wire (diameter 0.031 in) which, when pushed from the catheter base, advanced the inner catheter relative to the overtube. The inner catheter had a hydrogel-based hydrophilic coating (Lubricant UV, Harland Medical Systems, Eden Prairie, MN) to reduce friction. A soft silicone ball tip on the inner catheter was used to reduce perforation risk on insertion. The catheter base had three lumens: two air injection ports for balloon inflation, and one flush lumen that allowed injection of water through an orifice at the end of the overtube. This injection port allowed for the removal of pleats in the bowel during device cycling. Finally, the base of the device was mounted on a spring drive shaft that allowed for the application of continuous spring-generated push force on the inner catheter relative to the overtube (Fig. 1b).
a The catheter distraction enterogenesis device with latex balloons mounted on the outer catheter proximally (triangle) and inner catheter distally (arrow). b Diagram showing the Roux-en-Y construction and implantation of the device. An external spring applies forward force upon a nitinol wire embedded within the inner catheter, producing distraction between the distal balloon and the overtube-mounted proximal balloon. c The flexible device implanted in jejunal Roux limb, conforming to mesenteric curvature, actuated and produced longitudinal distractive force between the balloons
Animal model
The device was tested using our well-established swine model for distraction enterogenesis [16]. Female Yorkshire pigs (n = 6) weighing 30–50 kg were used for all experiments, which were approved by the University of Michigan Animal Use Committee (#PRO00005005). Although the device is designed for transgastric placement, the duodenum is 720° in pigs, and this precluded such placement for this trial. Therefore, it was elected to use a Roux-en-Y construction for this testing. Through a midline laparotomy, a Roux limb was created 90 cm distal to the ligament of Treitz. The proximal end of the distal bowel was brought out as a jejunostomy in the left lower abdomen. This stoma allowed for insertion of the catheter device. An end-to-side anastomosis was created to form a Roux-en-Y jejuno-jejunostomy, restoring intestinal continuity. The mesenteric defect was closed to prevent internal hernia. The device was inserted via the stoma into the Roux limb until the proximal balloon rested approximately 5 cm deep to the abdominal wall (Fig. 1c). The exclusion of the device from the normal enteric flow allowed for greater ease of trialing the device in the case of a pig which would not tolerate intermittent partial obstructions (i.e., pigs are intolerant of a nasogastric tube placement). Silastic markers (vessel loops) were placed along the antimesenteric border of the Roux limb at 3-cm intervals, and this served to allow for accurate measurement of gain or loss of intestinal length at harvest. A 12-cm segment was selected 10 cm distal to the jejuno-jejunostomy to serve as a fed control, and this was similarly marked at 3-cm intervals. The abdomen was then closed in standard fashion. To prevent dislodgement of the device, the external portion of the catheter device was secured to the animal’s skin with suture, and the spring drive box was mounted on the animal’s back with a custom jacket.
After a 24-h recovery period, the device was cycled twice daily. This consisted of balloon deflation, device retraction (resetting the device), flushing 30 mL of water to removal pleats in the bowel, resting for 5 min, inflation of both balloons to target pressure, and device expansion by advancing the distal balloon via the inner catheter. The inner catheter was mounted to a spring to apply the goal expansion tension on the bowel during expansion cycles. After 7 days, a repeat laparotomy was performed and intervals between antimesenteric Silastic markers were measured along the Roux limb and the control segment. In addition, attachment sites were inspected grossly for evidence of mucosal damage or perforation.
Tissue perfusion assessment
To characterize optimal filling pressure for the balloon attachments, visual and laser Doppler assessment of tissue perfusion was performed at each implant. After device insertion into the jejunal Roux limb, the latex balloons were filled with continuous balloon pressure monitoring until occlusion of vessels along the antimesenteric bowel wall was observed. This pressure was defined to be critical pressure, and target balloon pressure was set below this.
Blood flow to the antimesenteric bowel wall was measured using a Lisca PIM II Laser Doppler Perfusion Imager (Perimed AB, Stockholm, Sweden), placed 10 cm above the bowel segment of interest. Perfusion patterns were analyzed using LDPIwin 2.3 software (Perimed AB) as previously described [19]. Sequential measurements were taken at the same site during balloon inflation to 52 mmHg and deflation to quantify changes in tissue perfusion at attachment sites.
Analysis
All longitudinal growth measurements were made along the experimental Roux limb relative to a fed control segment. Unfed small intestine is known to result in intestinal atrophy [20]; therefore, additional comparisons were made to an unfed control intestinal segment (a segment of the Roux limb where the device was not present). This allowed assessment of device-induced enterogenesis versus prevention of atrophy. Paired t test was used to compare results from distracted and control segments from matched animals. P < 0.05 was considered significant.
Results
Balloon attachment strength
At implant, the device was calibrated to determine maximum longitudinal force before device slippage. After device insertion and balloon inflation, the inner catheter was manually advanced relative to the overtube using the spring drive shaft. Longitudinal bowel tension was observed between the balloon attachments (Fig. 1c), with balloon slippage occurring above 375 gram force (gf) of externally applied spring force. With the balloons deflated, 291 gf was required before inner catheter slippage, representing the total system friction without balloon attachments. This indicated that the balloon attachments allowed an additional 84 gf of longitudinal distraction prior to slippage. At explant, however, balloon attachment efficacy was diminished, with balloon slippage occurring with the device expansion to the same externally applied force of 375 gf.
Tissue perfusion
Visual inspection of antimesenteric bowel wall vessels during balloon inflation with continuous pressure monitoring demonstrated vessel occlusion at 59 mmHg balloon pressure. As 42 mmHg balloon pressure was required for balloon expansion ex vivo, it was estimated that 17 mmHg of transmural pressure was applied to the bowel at this critical level of balloon inflation. Therefore, to prevent any blood flow occlusion, a pressure level of 52 mmHg was selected as the target balloon pressure for the chronic studies.
Laser Doppler measurements showed no significant decrease in tissue perfusion with balloon inflation at attachment sites at implant [0.62 ± 0.42 perfusion units (PU) vs 0.53 ± 0.39 PU with inflation vs deflation; p = 0.16; Fig. 2]. Laser Doppler measurements were repeated at explant, confirming no compromise in perfusion after chronic implant (0.09 ± 0.02 PU vs 0.05 ± 0.01 PU; p = 0.07). PU is a dimensionless unit used for laser Doppler measurement, with environment-specific calibration preventing the comparison of measurements at implant and explant.
Lengthening
After 7 days, the distracted segment (measured after removal of the device) achieved a significant increase in length relative to fed (p < 0.001) and unfed (p < 0.001) control segments (Fig. 3a). Bowel lengthening was noted from the stoma to the end of the device, with greatest relative lengthening occurring between the proximal and distal balloon attachment sites. Percent net growth of the bowel located between the balloon attachments relative to fed control was 26.1 ± 6.1, and 66.7 ± 14.5 % versus unfed bowel (Fig. 4). While this indicated that the balloons successfully applied distractive force, the additional lengthening between the distal balloon and device tip reveals that the flexible catheter itself induced growth independent of the balloon attachments.
Increase in length of the distracted segment relative to fed and unfed controls. Each marker was initially placed 3 cm apart, beginning at the stoma. The % increase in distance from the stoma to each marker is shown (relative to controls), with the locations of the proximal balloon, distal balloon, and device tip (at full stroke). Maximum % growth was calculated at marker 8, corresponding to the distal balloon. All measurements were taken with the device in place
As the device had a finite stroke length, the gain in bowel length was dependent upon the length of bowel with which the device interacted and applied distractive force. The measured length of the distracted segment at explant is shown in Fig. 5, as the cumulative distance from the stoma to each bowel marker is graphed (with markers initially placed 3 cm part). The fed and unfed control segments had markers also placed 3 cm apart at implant. Control segment marker intervals at explant are shown extrapolated over the same number of markers as the distracted segment (i.e., if a 6-cm segment increased in length by 50 %, the distance from stoma to marker#2 would be 9 cm). The gain in length of the fully distracted segment relative to fed control was 6.3 ± 2.3, and 12.9 ± 7.6 cm relative to unfed control. Over 7 days, this corresponded to an average growth rate of 0.9 ± 0.3 cm/day versus fed control and 1.8 ± 1.1 cm/day versus unfed control.
Length gained via distraction enterogenesis. The distance from the stoma to each marker is shown for the distracted segment (mean values). Control segments were extrapolated over the same number of markers to compare total bowel length gain. Hash = 6.3 ± 2.3 cm gain vs fed control. Asterisk = 12.9 ± 7.6 cm gain vs unfed control
Mucosal effects
No balloon-related perforation occurred. The mucosa at balloon sites demonstrated occasional sloughing with intact submucosa (Fig. 3b). No evidence of serosal or mesenteric damage occurred. One perforation with abscess occurred where the distal silicone ball tip eroded through the intestinal wall. While this did not result in clinical deterioration, it demonstrates a limitation of the current device design in that a relatively rigid device exerts radial force upon the antimesenteric bowel wall. Atraumatic device tip geometry may prevent this complication.
Other adverse events
One device failure occurred, characterized by proximal balloon rupture. A replacement device was successfully placed via the jejunostomy without requiring reoperation. One surgical adverse event occurred, in which a small bowel volvulus occurred on the second postoperative day. The volvulized segment was in the distal ileum and not associated with the device. This animal was killed early and excluded from analysis.
Discussion
This study represents the first description of fully endoluminal distraction enterogenesis. This was accomplished using a novel catheter-based device which employed compliant latex balloons. A similar approach is currently employed in double-balloon enteroscopy [21] to allow for distal exploration of the small intestine. A significant difference, however, is that the inner catheter during enteroscopy is pushed forward when the balloon is deflated, and the balloon is then used to provide enough friction to pull the bowel toward the proximal balloon. This application requires relatively low attachment strength compared to distraction enterogenesis, where the bowel is placed on tension. Establishing the strength of the compliant latex balloons was, therefore, important to establish their ability to create tension without slippage. We demonstrated that this method of attachment allowed the application of an additional 84 gf before device slippage. As effective distraction enterogenesis occurs at forces above 45 gf with an end-abutting device, these balloons delivered provided adequate attachment strength. An additional advantage of the current lengthening approach allows for repeated retraction and lengthening of a relatively short segment of the intestine. Thus, this approach could be used for patients with severely short lengths of small bowel.
Balloon attachment strength is directly proportional to both the coefficient of friction of the balloon-mucosa interaction and the radial force of the balloon upon the intestinal wall. Increasing balloon pressure thus increases attachment strength, but at the potential expense of tissue perfusion. It was, therefore, important to define safe balloon pressure parameters. We used both visual inspection of bowel wall vessel occlusion as well as laser Doppler measurements of changes in tissue perfusion along the antimesenteric bowel wall during balloon inflation and deflation. This maximum balloon inflation pressure was 59 mmHg, which was likely affected by intestinal diameter and mean arterial pressure during intraoperative pressure testing. At the target balloon inflation pressure, which was similar to that employed in double-balloon enteroscopy [21], no significant change in laser Doppler-measured tissue perfusion occurred at implant or explant.
This device achieved lengthening rates that compared favorably to STEP outcomes. As patients with <10 % expected bowel length, or those with ultra-short bowel syndrome, are the least likely to respond to medical therapy, this subgroup of patients may be ideal candidates for distraction enterogenesis [2]. With 7 days of distraction enterogenesis, this double-balloon device achieved 26.1 ± 6.1 % growth vs nondistracted fed bowel and 66.7 ± 14.5 % vs unfed bowel. In comparison, the current standard of care, a primary STEP procedure in children with SBS, has been shown to result in ~36.4 ± 13.1 % increase in bowel length [22]. It is important to note, however, that STEP lengthening is measured at a single operative setting, whereas distraction enterogenesis requires delayed measurement of bowel growth after the distraction period relative to control nondistracted bowel. In addition, while the relatively high growth relative to unfed control may be partially due to prevention of atrophy associated with enteral deprivation in the Roux segment, the significant growth relative to fed control indicates that true enterogenesis was accomplished.
A limitation of the animal model used in this study was the requirement of device implant at laparotomy. This created differences from the envisioned method of clinical use. A double-balloon catheter device has several advantages, including a narrow caliber and flexibility, which allow placement via a stoma or gastrostomy. In this model, however, a laparotomy was required at implant to place bowel markers to measure efficacy. Explant, therefore, occurred on postoperative day 7, at which time significant intra-abdominal adhesion formation had occurred. To control for generalized changes in bowel length due to the postoperative peritoneal inflammation and adhesions, lengthening outcomes were measured relative to control segments which were exposed to the same peritoneal environment. In future studies, as well as in clinical use, marker placement may be replaced with serial contrast studies to monitor distraction outcomes.
Another limitation of the current surgical model was the deployment of the device into an unfed jejunal Roux segment. While the patients who would benefit from this would likely be PN-dependent, it will be important to demonstrate that the device can be placed in non-diverted bowel to ensure efficacy and lack of obstruction if placed via a gastrostomy or end enterostomy. This may be demonstrated in the porcine model by creating the Roux-en-Y jejunostomy followed by a delayed non-operative device implant via the stoma. The feasibility of this was demonstrated by the one device failure we encountered, in which a replacement device was successfully placed via the jejunostomy.
Two limitations of the current device were recognized in this study. First, the geometry of the device tip produced a small perforation with abscess in a single animal. This occurred in spite of a soft silicone ball to distribute tip pressure on the bowel wall. An atraumatic device tip will be required in future prototypes. Second, the balloon attachments were noted to lose effectiveness over time. Initial attachment strength of 84 gf was attributable to the balloons. By increasing the efficacy of the catheter device’s attachments, future devices may produce more efficient enterogenesis, especially over longer implant periods.
Concluding remarks
We described the first fully endoluminal distraction enterogenesis device. Successful enterogenesis was achieved with lengthening outcomes comparable to surgical lengthening. Improvements for inclusion in future prototypes were identified. This represents an important step towards the production of a device for clinical use in treating patients with medically refractory SBS.
References
Squires RH, Duggan C, Teitelbaum DH, Wales PW, Balint J, Venick R, Rhee S, Sudan D, Mercer D, Martinez JA, Carter BA, Soden J, Horslen S, Rudolph JA, Kocoshis S, Superina R, Lawlor S, Haller T, Kurs-Lasky M, Belle SH, Pediatric Intestinal Failure C (2012) Natural history of pediatric intestinal failure: initial report from the Pediatric Intestinal Failure Consortium. J Pediatr 161(4):723–728. doi:10.1016/j.jpeds.2012.03.062
Spencer AU, Neaga A, West B, Safran J, Brown P, Btaiche I, Kuzma-O’Reilly B, Teitelbaum DH (2005) Pediatric short bowel syndrome: redefining predictors of success. Ann Surg 242(3):403–409 (discussion 409–412)
Bianchi A (1980) Intestinal loop lengthening–a technique for increasing small intestinal length. J Pediatr Surg 15(2):145–151
Kimura K, Soper RT (1990) Isolated bowel segment (model 1): creation by myoenteropexy. J Pediatr Surg 25(5):512–513
Kim HB, Lee PW, Garza J, Duggan C, Fauza D, Jaksic T (2003) Serial transverse enteroplasty for short bowel syndrome: a case report. J Pediatr Surg 38(6):881–885
Sudan D, Thompson J, Botha J, Grant W, Antonson D, Raynor S, Langnas A (2007) Comparison of intestinal lengthening procedures for patients with short bowel syndrome. Ann Surg 246(4):593–601. doi:10.1097/SLA.0b013e318155aa0c (discussion 601–594)
Lao OB, Healey PJ, Perkins JD, Horslen S, Reyes JD, Goldin AB (2010) Outcomes in children after intestinal transplant. Pediatrics 125(3):e550–e558. doi:10.1542/peds.2009-1713
Park J, Puapong DP, Wu BM, Atkinson JB, Dunn JC (2004) Enterogenesis by mechanical lengthening: morphology and function of the lengthened small intestine. J Pediatr Surg 39(12):1823–1827
Safford SD, Freemerman AJ, Safford KM, Bentley R, Skinner MA (2005) Longitudinal mechanical tension induces growth in the small bowel of juvenile rats. Gut 54(8):1085–1090. doi:10.1136/gut.2004.061481
Spencer AU, Sun X, El-Sawaf M, Haxhija EQ, Brei D, Luntz J, Yang H, Teitelbaum DH (2006) Enterogenesis in a clinically feasible model of mechanical small-bowel lengthening. Surgery 140(2):212–220. doi:10.1016/j.surg.2006.03.005
Miyasaka EA, Okawada M, Utter B, Mustafa-Maria H, Luntz J, Brei D, Teitelbaum DH (2010) Application of distractive forces to the small intestine: defining safe limits. J Surg Res 163(2):169–175. doi:10.1016/j.jss.2010.03.060
Koga H, Sun X, Yang H, Nose K, Somara S, Bitar KN, Owyang C, Okawada M, Teitelbaum DH (2012) Distraction-induced intestinal enterogenesis: preservation of intestinal function and lengthening after reimplantation into normal jejunum. Ann Surg 255(2):302–310. doi:10.1097/SLA.0b013e318233097c
Sullins VF, Wagner JP, Walthers CM, Chiang EK, Lee SL, Wu BM, Dunn JC (2014) Function of mechanically lengthened jejunum after restoration into continuity. J Pediatr Surg 49(6):971–974. doi:10.1016/j.jpedsurg.2014.01.033 (discussion 974–975)
Okawada M, Maria HM, Teitelbaum DH (2011) Distraction induced enterogenesis: a unique mouse model using polyethylene glycol. J Surg Res 170(1):41–47. doi:10.1016/j.jss.2011.03.041
Ralls MW, Sueyoshi R, Herman RS, Utter B, Czarnocki I, Si N, Luntz J, Brei D, Teitelbaum DH (2013) Mesenteric neovascularization with distraction-induced intestinal growth: enterogenesis. Pediatr Surg Int 29(1):33–39. doi:10.1007/s00383-012-3204-5
Ralls MW, Sueyoshi R, Herman R, Utter B, Czarnocki I, Luntz J, Brei D, Teitelbaum DH (2013) Development of a novel approach to safely couple the intestine to a distraction-induced device for intestinal growth: use of reconstructive tissue matrix. Pediatr Surg Int 29(2):151–156. doi:10.1007/s00383-012-3198-z
Chawla BK, Teitelbaum DH (2013) Profound systemic inflammatory response syndrome following non-emergent intestinal surgery in children. J Pediatr Surg 48(9):1936–1940. doi:10.1016/j.jpedsurg.2013.05.065
Stark R, Zupekan T, Bondada S, Dunn JC (2011) Restoration of mechanically lengthened jejunum into intestinal continuity in rats. J Pediatr Surg 46(12):2321–2326. doi:10.1016/j.jpedsurg.2011.09.019
Riordan CL, McDonough M, Davidson JM, Corley R, Perlov C, Barton R, Guy J, Nanney LB (2003) Noncontact laser Doppler imaging in burn depth analysis of the extremities. J Burn Care Rehabil 24(4):177–186. doi:10.1097/01.BCR.0000075966.50533.B0
Goldstein RM, Hebiguchi T, Luk GD, Taqi F, Guilarte TR, Franklin FA Jr, Niemiec PW, Dudgeon DL (1985) The effects of total parenteral nutrition on gastrointestinal growth and development. J Pediatr Surg 20(6):785–791
May A, Nachbar L, Wardak A, Yamamoto H, Ell C (2003) Double-balloon enteroscopy: preliminary experience in patients with obscure gastrointestinal bleeding or chronic abdominal pain. Endoscopy 35(12):985–991. doi:10.1055/s-2003-44582
Wales PW, Jancelewicz T, Romao RL, Piper HG, de Silva NT, Avitzur Y (2013) Delayed primary serial transverse enteroplasty as a novel management strategy for infants with congenital ultra-short bowel syndrome. J Pediatr Surg 48(5):993–999. doi:10.1016/j.jpedsurg.2013.02.015
Acknowledgments
Gail Rising, DVM, Amber Yanovich, LVT, and Janet Wolforth, LVT provided veterinary care and their contributions are appreciated. This research was supported by NIH 2R44DK085765-02, FDA P50 Pediatric Device Consortia Grant 2-P50-FD-003787-03, and a Hartwell Biomedical Research Award.
Conflict of interest
The authors declare no conflicts of interest relevant to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Demehri, F.R., Wong, P.M., Freeman, J.J. et al. A novel double-balloon catheter device for fully endoluminal intestinal lengthening. Pediatr Surg Int 30, 1223–1229 (2014). https://doi.org/10.1007/s00383-014-3612-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3612-9