Abstract
Purpose
To analyze the relationship between spinal cord and vertebral abnormalities from the point of view of embryology.
Methods
We analyzed the clinical and radiological data of 260 children with different types of spinal cord malformations in combination with vertebral abnormalities.
Results
Among 260 individuals, approximately 109 presented with open neural tube defects (ONTDs), 83 with split cord malformations (SCMs), and 83 with different types of spinal lipomas. Pathological spina bifida emerged as the most frequent vertebral anomaly, affecting 232 patients, with a higher prevalence in ONTD. Vertebral segmentation disorders, including unsegmented bars, butterfly vertebrae, and hemivertebrae, were present in 124 cases, with a higher prevalence in SCM. The third most common spinal anomaly group consisted of various forms of sacral agenesis (58 cases), notably associated with blunt conus medullaris, spinal lipomas, and sacral myelomeningocele. Segmental aplasia of the spinal cord had a typical association with segmental spinal absence (N = 17).
Conclusion
The association between SCM and neuroenteric cyst/canal and vertebral segmentation disorders is strong. High ONTDs often coincide with pathological spina bifida posterior. Type 1 spinal lipomas and focal spinal nondisjunction also correlate with pathologic spina bifida. Segmental spinal absence or dysgenesis involves localized spinal and spinal cord aplasia, sometimes with secondary filar lipoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neural tube defects represent one of the most prevalent malformations of the nervous system. These conditions frequently lead to walking and urination disorders in affected children. Despite significant research efforts, the pathogenesis of some spinal abnormalities remains incompletely understood, with multiple theories positing both genetic and environmental factors as potential contributors [1,2,3].
Spinal cord abnormalities are strongly linked to vertebral abnormalities, with the most well-known and perhaps overly emphasized condition being spina bifida. However, numerous other conditions exist, such as disorders of segmentation [4, 5], sacral agenesis and aplasia [6], segmental spinal dysgenesis [7], and more. It is well established that most spinal cord abnormalities occur during the initial month of pregnancy in the neurulation period [8]. During this period, another crucial process occurs: the notochord develops in very close connection with the neural tube [9].
The hypothesis of this study posits that disruptions during different stages of embryological development can potentially lead to or be associated with various anomalies of the spine and spinal cord.
Material and methods
A group of 260 patients with concomitant spinal cord abnormalities and spine anomalies were analyzed. These patients were treated at the same clinic between 2012 and 2022. The evaluation criteria primarily focused on categorizing the anomalies affecting the spine and spinal cord.
For each patient, a comprehensive assessment was conducted, involving X-ray imaging of the entire spine in two projections, as well as spinal MRI. Furthermore, a considerable proportion of patients with significant spinal pathology underwent additional CT scans. The abnormalities were initially analyzed by three specialists—a radiologist, a neurosurgeon, and an orthopedic traumatologist—each working independently. Following this individual assessment, the results were consolidated, and any areas of disagreement were thoroughly discussed until a consensus was reached.
We grouped spinal developmental anomalies as follows: (1) segmentation disorders, encompassing hemivertebrae, butterfly vertebrae, and unsegmented bar; (2) absence of lumbar vertebrae and total sacral absence; (3) partial absence of the sacrum, including hemisacrum; (4) segmental aplasia or agenesis of the spine with preserved sacrum; and (5) pathological posterior spina bifida (wide, asymmetrical). We did not include patients with spinal cord developmental anomalies and physiological spina bifida in the selection.
Statistical analyses utilized Microsoft Excel 2019, employing ANOVA analysis to assess inter-group differences.
Results
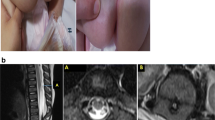
Among the 260 individuals, there were 161 girls (62%) and 99 boys (38%) spanning various age groups. Totaling 117 cases encompassed open neural tube defects (ONTDs) like myelomeningocele (MMC) or myeloschisis (MS). Among them, 109 cases were classified as “high” ONTDs, while 8 patients exhibited “low” sacral forms of MMC (Table 1). Most individuals with ONTDs exhibited an elongated dysplastic spinal cord terminating below the L1-2 level. Only 9 patients with ONTDs had a spinal cord break with or without dysplastic conus medullaris beneath the absent part of the spinal cord, usually occurring at the level of the lower thoracic region, accompanied by acute-angled kyphosis, segmental vertebral agenesis (Fig. 1), or lumbo-sacral agenesis. In 11 patients, a bony septum (split cord malformation type I) was identified below or under the ONTD (Fig. 2). The most common developmental abnormality in the group of patients with “high” ONTD was a pathological wide posterior spina bifida with flattened vertebrae (Table 1). There were also a number of patients with segmentation disorders, but it was significantly lower than, for example, in patients with split cord malformations (Table 2).
The next significant group comprised split cord malformation (SCM). Notably, 50% of cases involving SCM exhibited a lumbar bony septum, often accompanied by diplomyelia, low-lying conus medullaris, with or without fatty filum (Fig. 3). An interesting finding was the co-occurrence of SCM with other conditions, such as spinal lipoma type 3-4 in 33 cases, “high” ONTDs in 12 cases, focal spinal nondisjunction (FSN) in 5 cases (see Table 1), and epidermoid cyst in 2 cases. SCM group was primarily characterized by a combination of segmentation disorders (Table 1). Spina bifida posterior was also quite common in this group, but significantly less than in patients with ONTD (Table 2).
The final significant group consists of individuals with spinal lipomas, predominantly spinal lipoma type 4 (filum terminalis lipoma, FTL). A notable observation was the high occurrence of spinal lipoma type 3-4 in combination with SCM (Figs. 3 and 4). Notably, spinal lipoma type 1-2 never coexisted with SCM, although it is worth saying that the number of patients with such abnormalities was quite small (11 cases). Various types of spinal lipomas were often accompanied by dermoid/epidermoid cysts and FSN. In cases of spinal lipomas, the most frequent vertebral anomalies observed were sacral aplasia, spina bifida, and segmentation disorders (Table 1). Sacral aplasia in patients with spinal lipomas was more common than in other groups (Table 2).
Segmental spinal aplasia was observed in 17 patients (Table 1), and all of them exhibited segmental vertebrae aplasia at the same level. Among them, 6 patients had the classic form of segmental spinal dysgenesis with local narrowing of the spinal cord in the thoracolumbar area with the normal position of conus medullaris (Fig. 5), while 11 individuals had accompanying low-lying conus medullaris with or without FTL (Fig. 6). It should be noted that segmental aplasia of the spine itself was found not only in this group of spinal cord malformations but also in ONTD cases (Fig. 1) and FTL (Fig. 7).
Blunt conus medullaris was identified in seven patients, and in the majority of these cases, it was associated with diverse forms of sacral aplasia (Fig. 8).
Discussion
It is probable that each defect in the development of the neural tube and notochord arises at distinct stages and is linked to varying mechanisms.
Table 3 represents a hypothetical compilation of data related to different stages and types of neural tube defects, as well as their associated vertebral conditions. The table appears to have been constructed by drawing upon our own research data and existing literature. It serves as a visual representation of a working hypothesis or a theoretical framework. Below, we have given some facts from our literature review in defense of our theory.
Gastrulation: SCM, neuroenteric cysts, and segmentation disorders
On day 13 of embryo development, gastrulation starts as a primitive streak emerges on the dorsal area of the embryo’s mid-caudal region. Epiblast cells move downward through this streak, forming the endoderm, mesoderm, and ectoderm layers. The primitive streak becomes a groove, and its anterior portion folds in to create the primitive pit. This process shapes the notochordal canal, which will develop into the notochord, with cells migrating from the specialized Hensen node [10].
The notochord develops concurrently with the regression of the primitive streak. Between days 17 and 25 of gestation, a series of complex events occurs as the notochordal canal transitions into a plate and moves ventrally [9]. Afterward, the plate undergoes recanalization, creating a temporary connection between the dorsal amniotic cavity and the ventral yolk sac cavity known as the neuroenteric canal.
The neuroenteric canal plays a vital role in balancing cavity pressure and nutrient exchange. Upon completion of its function, the canal closes, prompting a gradual decrease in yolk sac size and an increase in the amniotic cavity. Developmental issues with canal closure or regression can result in neuroenteric cysts, persistent canals, and SCM [8].
One of the theories for the development of butterfly-shaped vertebrae is the persistence of the notochord, which prevents the fusion of lateral chondral centers [5]. As the notochord regresses normally, it enables the proper fusion of lateral chondral centers, forming well-shaped vertebral bodies. However, its persistence can disrupt this fusion, causing a distinctive butterfly-shaped appearance. In a significant study by Feng et al., high occurrence of SCM at lower thoracic and lumbar levels, often combined with multiple spinal segmentation anomalies (84%), was reported [11, 12]. The combination of NEC with Klippel Feil syndrome is also described, which also indicates a possible single genetic mechanism underlying the development of multiple anomalies in spinal segmentation, NEC, and SCM [13].
In our series, we noted a high incidence of SCM coupled with segmentation disorders, primarily localized in the caudal region (L2 and below), aligning with the embryonic localization of the neuroenteric canal. The consistent co-occurrence of SCM, NEC, and vertebral segmentation disorders suggests a shared mechanism involving regression abnormalities and persistent neuroenteric canal and notochord. This association hints at an underlying developmental pathway influencing their formation and regression. The presence of spinal cord lipomas alongside SCM and NEC is likely secondary. Similarly, SCM in some ONTDs indicates that severe ONTD forms may manifest during gastrulation.
Early primary neurulation: “high” ONTD and wide spina bifida with vertebral flattening
Between days 16 and 28 of gestation, notochord formation coincides with primary neurulation, where the neuroectoderm develops from the superficial middle layer of dorsal and cranial embryo cells. Primary neurulation involves two key steps: apposition and fusion of the cutaneous and neuroectoderm, followed by disjunction, facilitating proper neuroectoderm differentiation. ONTDs typically stem from primary neurulation disruptions, likely during early stages (apposition and fusion) and occasionally during gastrulation [10].
In our patient group, the majority of ONTD cases are located on the lumbar and thoracolumbar levels. Approximately 27% of “high” ONTD patients in our series had vertebral segmentation issues. However, this proportion sharply contrasted with those in SCM and NEC cases (see Table 2).
Pathological lumbar kyphosis in children with ONTD is well documented in the literature [14,15,16,17]. We also observed a significant number of such patients in our series. In all cases, there is a deformed wedge-shaped vertebra or two vertebrae at the apex of the kyphosis (Fig. 2).
The combination of ONTD and sacral agenesis is indeed a rare congenital condition characterized by abnormalities in the development of the neural tube and the sacrum during early fetal development. In a study by Balioğlu et al. [18], 19 cases of ONTD with sacral agenesis were described, with 2 cases having lower sacral agenesis and 18 cases having total agenesis of the sacrum. Emami-Naeini et al. also reported a case series of 9 patients with ONTD and caudal regression syndrome, but the type of sacral agenesis was not specified [19]. In our series, as well as in the series of Balioglu et al. and Emami-Naeini et al., patients with ONTD had different types of sacral agenesis: lumbo-sacral absence (6%) or low sacral aplasia and hemisacrum (9%).
Late primary neurulation: focal spinal nondisjunction, dermoid and epidermoid cyst, spinal lipomas type 1, and lumbo-sacral spina bifida
Congenital dermal sinus is a link that draws skin tissue toward the neural side [2]. In limited dorsal myeloschisis neural tissue, to move toward the skin side, contrary to dermal sinus, the lumen and epithelial cells inside are not detected [20]. Also, transitional forms reported in the literature [20] provide insight into a potential shared developmental mechanism. These processes may lead to the inclusion of tumors like dermoid or epidermoid cysts along this connection.
There are two opinions about the origin of FSN: a violation of primary neurulation [21, 22] or secondary [20]. Our study showed that in terms of the frequency of combination with different malformations, this group of patients is closest to MMC, myeloschisis, and spinal lipoma type 1: the frequent presence of simple spina bifida was noted, while other vertebral anomalies were rare. In our series, it is possible that congenital dermal sinuses and limited dorsal myeloschisis were observed in conjunction with both SCM and FTL. The specific location can provide insights into the precise timing of their occurrence.
Investigations into whether type 1 spinal cord lipomas stem from primary neurulation disruption continue. Unlike ONTDs, there is no outer integument defect, and nerve elements are not directly connected to the skin (successful disjunction). Yet type 1 lipomas are associated with subcutaneous fat, indicating improper neural tube closure and significant neurological deficits, akin to ONTDs. Another theory suggests that pathological neuro-mesenchymal adhesions may contribute to this anomaly, positing abnormal tissue connections as potential factors [2].
Junctional neurulation: segmental spinal dysgenesis, spinal lipoma 2, blunt conus medullaris, segmental lumbar, and sacral agenesis
Junctional neurulation is a distinct process that occurs during gestation week 4 of embryonic development. It involves the transformation of specific regions of Hensen’s node and the primitive streak (node-streak border) into the neural tube. Unlike the rostral neuroectoderm, which forms the rest of the neural tube, this region follows a different process to close and form the neural tube [2, 23, 24].
In this region, two cell groups exist: dorsolateral and ventromedial. Dorsolateral cells contribute to primary neurulation, forming the neural tube, while ventromedial cells engage in secondary neurulation, adding to the neural tube. Junctional neurulation, occurring around gestational week 4, shapes the thoracolumbar spine junction, a pivotal area in embryo development. Understanding this process is crucial for grasping the origins of certain congenital malformations and neural tube defects in this region, like local spinal aplasia, spinal lipomas (type 2), and blunt-ended conus medullaris [25]. The main theory for the occurrence of segmental spinal dysgenesis involves an embryonic insult, likely during the critical period when junctional neurulation takes place.
Blunt conus medullaris often coincides with lumbo-sacral and full sacral agenesis in our series and may involve a disruption in junctional neurulation. This condition shares similarities with segmental spinal dysgenesis, presenting as spinal cord aplasia in the junctional zone alongside spinal segment or sacrum aplasia. These defects, distinct from other neural tube issues, typically occur independently, less frequently with spina bifida, and often involve segmental spine and sacrum aplasia. Possible causes include local blood supply disorders or segmental vessel anomalies.
Type 2 spinal lipomas, occurring during the junctional period, likely result from mesenchymal tissue ectopia or regression disorders in embryonic structures. They share similarities with type 1 and type 3 spinal lipomas, suggesting a unified developmental mechanism.
Early secondary neurulation: spinal lipomas 3, sacral MMC, low sacral aplasia, and hemisacrum
Between days 27 and 31 of embryonic development, significant caudal neural growth occurs through secondary neurulation, originating from the caudal cell mass—a cluster of cells from the regressed primitive streak. This mass forms the caudal segment of the spinal cord and spine. While the notochord directs primary neurulation, the neural tube reciprocally influences spine formation. However, the regulatory factors for secondary neurulation are unknown. It is theorized that those disruptions in secondary neurulation led to most cases of caudally located closed spinal dysraphism [2].
An alternative theory posits that certain cases of ONTDs, specifically “low” sacral forms, may emerge due to secondary neurulation disruption. This theory hinges on the observation that hydrocephalus and Chiari anomaly are less prevalent in “low” ONTDs. Two potential mechanisms are postulated: unsuccessful ingression of the primitive streak into the caudal cell mass leading to the formation of dorsal-limited myeloschisis in the sacral or lower lumbar region or the rupture of an anomalous “terminal balloon” at the lowest spine portion (around the future sacral hiatus), resulting in caudal skin defect formation. This notion is supported by our findings on patients with “low” ONTDs, who exhibited no Chiari anomalies, hydrocephalus, or vertebral splitting.
The recurrence of low forms of sacral aplasia in this cohort, albeit not affecting treatment outcomes, could possibly be attributed to disrupted sacral formation from the caudal cell mass. This disruption may result from mechanical damage during terminal balloon rupture or the violation of local regulatory mechanisms.
Disorders of late secondary neurulation: FTL and sacral spina bifida
In situations where a focal neuro-mesenchymal connection occurs in the lower dorsal region of the medullary cord—similar to a minor variation of the transitional type—and the involution of the distal medullary cord follows its normal course, it could potentially lead to the development of focal fatty tissue within the filum. Another possible mechanism may be, again, a violation of the regression of the secondary neural tube.
In general, when considering all anomalies of spinal cord development, they can be conditionally divided into several categories:
-
1.
Disruptions on migration and reduction of embryonic structure: SCM, spinal lipomas, NEC, FSN, dermoids, and epidermoids. In this case, the skin, muscles, bones, and spinal cord membranes remain intact, but there are derivatives of embryonic structures that typically require removal.
-
2.
Failure of closure of the skin, muscles, bones, and membranes: ONTD and FSN. These anomalies require urgent closure due to the potential pathological communication of cerebrospinal fluid with the surrounding environment and the potential risk of infection and meningitis. Also, they may lead to a retained spinal cord, which in some cases requires untethering as the individual grows.
-
3.
The absence of anatomical structures, like aplasia or agenesis, can present as segmental spinal absence (referred to as junctional neurulation disorder) or a blunt conus medullaris. Generally, in cases of isolated spinal cord anomaly, active surgical intervention is unnecessary. However, concurrent spinal anomalies sometimes necessitate spine stabilization to avert complications such as spinal dislocation and instability. Examples of such anomalies include segmental spinal dysgenesis with congenital spinal dislocation, spino-pelvic disconnection resulting from severe sacral aplasia or one-sided sacro-pelvic dislocation due to hemisacrum.
Approaches to the treatment of spinal pathology are straightforward: if there is progressive deformation and instability of the spine, the patient requires surgical intervention.
Conclusions
The relationship between SCM, NEC, and vertebral segmentation disorders is notably strong. These conditions may be linked to disruptions in the regression and apoptosis processes of specific embryonic structures, particularly the neuroenteric canal and notochord. In cases of “high” ONTDs, there appears to be a significant association with extensive pathological spina bifida posterior. Additionally, both type 1 spinal lipomas and FSN also exhibit a distinct correlation with pathologic spina bifida.
Segmental spinal absence or segmental spinal dysgenesis represents a cohesive category of anomalies marked by localized spinal and spinal cord aplasia, sometimes accompanied by secondary FTL. Blunted conus medullaris frequently presents alongside sacral aplasia.
Data availability
In compliance with privacy regulations and ethical standards, access to the patient database used in this study cannot be granted. The database contains personally identifiable information, such as names and surnames, making it unsuitable for sharing.
References
Kancherla V (2023) Neural tube defects: a review of global prevalence, causes, and primary prevention. Childs Nerv Syst 39(7):1703–1710
Yang J, Lee JY, Kim KH, Wang KC (2021) Disorders of secondary neurulation : mainly focused on pathoembryogenesis. J Korean Neurosurg Soc 64(3):386–405
Ravi KS (2021) Divasha, Hassan SB, Pasi R, Mittra S, Kumar R: Neural tube defects: different types and brief review of neurulation process and its clinical implication. J Family Med Prim Care 10(12):4383–4390
Mackel CE, Jada A, Samdani AF, Stephen JH, Bennett JT, Baaj AA, Hwang SW (2018) A comprehensive review of the diagnosis and management of congenital scoliosis. Childs Nerv Syst 34(11):2155–2171
Katsuura Y, Kim HJ (2019) Butterfly vertebrae: a systematic review of the literature and analysis. Global Spine J 9(6):666–679
Warner T, Scullen TA, Iwanaga J, Loukas M, Bui CJ, Dumont AS, Tubbs RS (2020) Caudal regression syndrome-a review focusing on genetic associations. World neurosurgery 138:461–467
Kim KH, Lee JY (2021) Junctional neurulation : a junction between primary and secondary neural tubes. J Korean Neurosurg Soc 64(3):374–379
Morota N, Sakamoto H (2023) Surgery for spina bifida occulta: spinal lipoma and tethered spinal cord. Childs Nerv Syst 39(10):2847–2864
de Bree K, de Bakker BS, Oostra RJ (2018) The development of the human notochord. PLoS ONE 13(10):e0205752
Dias MS, Partington M (2004) Embryology of myelomeningocele and anencephaly. Neurosurg Focus 16(2):E1
Milić I, Milić M, Djorić I, Marinković I, Boljanović J, Marinković S (2019) Spondylocostal dysostosis associated with split spinal cord and other malformations. Pediatr Neurosurg 54(6):367–374
Feng F, Tan H, Li X, Chen C, Li Z, Zhang J, Shen J (2017) Radiographic characteristics in congenital scoliosis associated with split cord malformation: a retrospective study of 266 surgical cases. BMC Musculoskelet Disord 18(1):420
Can A, Dos Santos Rubio EJ, Jasperse B, Verdijk RM, Harhangi BS (2015) Spinal neurenteric cyst in association with Klippel-Feil syndrome: case report and literature review. World Neurosurg 84(2):592.e599–514
Özdemir N, Özdemir SA, Özer EA (2019) Kyphectomy in neonates with meningomyelocele. Childs Nerv Syst 35(4):673–681
Ryabykh SO, Pavlova OM, Savin DM, Burtsev AV, Gubin AV (2018) Surgical management of myelomeningocele-related spinal deformities. World Neurosurg 112:e431–e441
Wui SH, Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2019) Kyphectomy and interbody fixation using lag screws in a child with myelomeningocele kyphosis: a technical case report. Childs Nerv Syst 35(8):1407–1410
Alshaalan KS, Howard JJ, Alshangiti AK, Alkhalife YI, Aleissa S, Al Sayegh SO (2019) Kyphectomy in myelomeningocele for severe early-onset kyphosis using distal intravertebral fixation and thoracic growing rods. J Am Acad Orthop Surg Glob Res Rev 3(9):e006
Balioğlu MB, Akman YE, Ucpunar H, Albayrak A, Kargın D, Atıcı Y, Büyük AF (2016) Sacral agenesis: evaluation of accompanying pathologies in 38 cases, with analysis of long-term outcomes. Childs Nerv Syst 32(9):1693–1702
Emami-Naeini P, Rahbar Z, Nejat F, Kajbafzadeh A, El Khashab M (2010) Neurological presentations, imaging, and associated anomalies in 50 patients with sacral agenesis. Neurosurgery 67(4):894–900 discussion 900.
Kim JW, Wang KC, Chong S, Kim SK, Lee JY (2020) Limited dorsal myeloschisis: reconsideration of its embryological origin. Neurosurgery 86(1):93–100
Wong ST, Pang D (2021) Focal spinal nondisjunction in primary neurulation : limited dorsal myeloschisis and congenital spinal dermal sinus tract. J Korean Neurosurg Soc 64(2):151–188
Pang D, Zovickian J, Wong ST, Hou YJ, Moes GS (2013) Limited dorsal myeloschisis: a not-so-rare form of primary neurulation defect. Childs Nerv Syst 29(9):1459–1484
Eibach S, Pang D (2020) Junctional neural tube defect. J Korean Neurosurg Soc 63(3):327–337
Ali M, McNeely PD (2018) Junctional neural tube defect: a supporting case report. Childs Nerv Syst 34(8):1447–1448
Wang KC, Lee JS, Kim K, Im YJ, Park K, Kim KH, Phi JH, Kim SK, Lee JY (2020) Do junctional neural tube defect and segmental spinal dysgenesis have the same pathoembryological background? Childs Nerv Syst 36(2):241–250
Author information
Authors and Affiliations
Contributions
O.M.S. and D.M.S. conceived and designed the study. O.M.S., D.M.S., and K.A.D. collected and analyzed the clinical and radiological data. O.M.S., D.M.S., and K.A.D. interpreted the results and contributed to the drafting of the manuscript. O.M.S. and D.M.S. contributed equally to writing the main manuscript text. All authors critically reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were approved by the Institutional Review Board and were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
This retrospective study solely involved the analysis of clinical images and did not influence the standard algorithm for examination and treatment. As such, specific informed consent for participation in the study was not obtained. Instead, the standard consent for examination and treatment was administered during the course of diagnosis and treatment. In accordance with ethical guidelines, it is important to note that this study was exempt from obtaining distinct informed consent for retrospective analysis. The study adheres to applicable regulations, and the exemption has been approved by Ilizarov Center IRB.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sergeenko, O.M., Savin, D.M. & Diachkov, K.A. Association of spinal cord abnormalities with vertebral anomalies: an embryological perspective. Childs Nerv Syst 40, 1415–1425 (2024). https://doi.org/10.1007/s00381-024-06336-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-024-06336-5