Abstract
Purpose
Retrospective analysis of clinical and epidemiological characteristics of central nervous system (CNS)tumors in Uyghur children from a single center in Xinjiang.
Methods
Between January 2013 and December 2021, 243 children (0–17 years old) with a clear pathological type of CNS tumor are collected and analyzed for tumor size, grade, and category, as well as their relationship with the child’s gender, age, and region of origin according to the 2021 edition of the new WHO CNS tumor classification.
Outcome
The 243 cases of CNS tumors in Uyghur children are predominantly from rural areas, with 144 cases (59.26%) of supratentorial tumors and 129 cases (53.09%) of low-grade tumors. With an overall male-to-female ratio of 1.43:1, a peak age of incidence of 6 to 8 years.
Concluding
The present study is based on a 9-year analysis of pediatric CNS data from a single center, and the center is the largest tertiary hospital in Xinjiang with large numbers of admitted patients, which may reflect some extent the clinical characteristics and epidemiological features characteristics of pediatric CNS tumors in Uyghur in Xinjiang.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
CNS tumors are the second most common cancers in pediatric populations, and among pediatric solid tumors, CNS tumors are the most common and have the highest mortality rate of all pediatric tumors, with incidence rates as high as 20% [1,2,3,4]. As the diagnosis and treatment of CNS tumors in pediatric patients continue to develop and improve, improvements have also been made in the detection rate of CNS tumors in pediatric patients [5]. The Uyghurs can be traced back to the third century B.C. and are part of the Turkic language family of the Altaic language family, mostly congregated in the north and northwest of China and south of Lake Baikal and between the Irtysh River and Lake Balkhash. The ancestors of the Uyghurs are thought by some to be related to the Hungarians, and Xinjiang, the main gathering place of the Uyghurs in China, is the home to 11,774,500 Uyghurs, representing more than half of the Uyghurs people in the world. However, there have been few analyses of pediatric CNS tumors in Uyghurs. For this reason, the present study is based on the most recent version of the WHO Classification of Tumors of the Central Nervous System (2021 edition), and the clinical data of Uyghur pediatric patients admitted to our neurosurgery department in the past 9 years are analyzed to supplement the clinical and epidemiological gaps of CNS tumors in Uyghur children.
Materials and methods
Date from 243 pediatric Uyghur (0–17 years old) with a confirmed diagnosis of CNS tumor admitted to the Department of Neurosurgery at the First Affiliated Hospital of Xinjiang Medical University between January 2013 and December 2021 are counted, including the hospitalization number, name, gender, age, date of admission, location of residence, clinical symptoms, primary diagnosis, pathological diagnosis, and imaging diagnosis. Pediatric patients are strictly checked for information to avoid duplication, and all receive treatment for tumor removal, the diagnosis of tumor tissue obtained is made by histopathology at the First Affiliated Hospital of Xinjiang Medical University, and all are confirmed to be CNS tumors by either light microscopic observation or (and) immunohistochemistry staining.
Clinical manifestations
In 6 cases, there are no overt CNS tumor symptoms or tumors due to head trauma or physical exam. A total of 237 cases are diagnosed as CNS tumors with clinical symptoms. Including 142 cases of headache, 113 cases of nausea and vomiting, 49 cases of loss of appetite, 44 cases of abnormal vision, 43 cases of disorders of limb movement disorder, 37 cases of balance dysfunction, 36 cases of seizure, 22 cases of dizziness, 21 cases of developmental abnormalities, 13 cases of polydipsia and polyuria, 13 cases of fever, 8 cases of limb pain, 8 cases of somnolence, 8 cases of cognitive dysfunction, 3 cases of abnormal crying, 2 cases of coma, 2 cases of difficulty in micturition, and respiratory difficulty in 1 case.
Classification and gradation
The pathological diagnosis of 243 pediatric cases is classified and graded in conjunction with the latest version of whom neurological classification criteria (2021 version), the age distribution, sex distribution, gender characteristics, clinical manifestations, tumor sites, and pathological types of the pediatric patients are statistically analyzed. The tumor sites are divided into the supratentorial, infratentorial, and spinal canals. Supratentorial tumors are divided into the cerebral hemisphere, the sella region, three ventricles, the lateral ventricles, and others, the infratentorial tumors are divided into the cerebellum, the brainstem, the fourth ventricle, and others. The tumor grade is divided into low-grade and high-grade, with WHO grades I and II classified as low-grade tumors and grades III and IV classified as high-grade tumors.
Statistical methods
Data are processed and analyzed using descriptive statistics and count data are expressed as frequency and rate (%).
Outcome
Histopathological types and subtypes of tumors with the size distribution
Of the 243 tumors in this group, 144 are supratentorial, comprising 59.26%, 86 are infratentorial tumors, comprising 35.39%, and 13 are spinal canal tumors, comprising 5.35%. Gliomas, glial neuronal tumors, and neuronal tumors account for the largest number with 107 cases (44.03%) in the type classification of pathologic tumor histology, followed by embryonal tumors in 49 cases (20.16%), tumors of the sellar tumors in 40 cases (16.46%), and mesenchymal non-membranous epithelial tumors in 13 cases (5.35%). In 42 cases (17.28%) medulloblastoma is one of the top 5 tumor subtypes, ependymal tumors in 34 cases (14.00%), craniopharyngioma in 30 cases (12.35%), pilocytic astrocytoma in 28 cases (11.52%), and pituitary tumors in 10 cases (4.12%) (Fig. 1, Table 1).
Gender and tumor age distribution
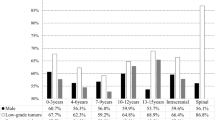
In our group, 142 (58.44%) of 243 CNS tumor cases are male and 101 (41.56%) are female. The sex ratio is 1.41:1. All patients are between 0 and 17 years old with a mean age of 8.81 years old. The age groups are divided into 0 to 2 years group, 3 to 5 years group, 6–8 years group, 9 to 11 years group, 12 to 14 years group, and 15 to 17 years group in 3-year intervals. Sex and age distribution statistics of the pediatric population have shown that the tumors are predominantly found in pediatrics aged 6–8 years. Among them, male pediatrics are mainly distributed among 6–8 years old and female pediatrics are mainly distributed among 12–14 years old (Fig. 2).
The Grade and age distribution of the tumors
Of the 243 CNS tumors in our group, low-grade is predominant, with 129 cases (53.09%), and high-grade has 114 cases (46.91%). With a ratio of 1.31:1 between the two groups. Based on statistics of tumor grade and the affected children's age show that the most affected patients are 6 to 8 years old and 15 to 17 years old in the lower grades and 3 to 5 years old in the upper grades (Fig. 3).
The region of origin and the year distribution of children with tumors
Our group of 243 CNS tumors includes 167 children of rural origin, constituting 68.72%, and 76 children of urban origin, constituting 31.28% of the population. With the exception of 2019, there are more children from rural sources than from urban sources for the period from 2013 to 2021 (Table 2).
Discussion
35.9 cases per million children aged 0–15 years in Sweden, 36.1 cases in Kumamoto Prefecture, Japan, 32.7 cases in Yorkshire, UK, 29.9 cases in 59 European cancer registries, and 47.1 cases in the US [6, 7], while according to CBTRUS statistics reporting Whites (6.36 per 100,000), Blacks (4.83 per 100,000), Asians (3.22 per 100,000), and Asian Pacific Islanders (API) (3.48 per 100,000) [8]. We can see that there are some differences between different regions and different ethnicities of pediatric tumors worldwide, despite the lower incidence of CNS tumors in Asian pediatrics, there are some studies that show little difference between the West and the East. The Uyghur people are ethnically close to Central Asia and the Middle East, and a study from Syria showed that the incidence of CNS tumors in Syrian pediatric does differ somewhat from that in Western and Far Eastern countries [7, 9]. This is a single-center study, and accurate incidence of CNS tumors in Uyghur pediatric patients is difficult to obtain, despite a large number of pediatric admission.
In this study, the ratio of male to female CNS tumors in pediatric patients in this study is 1.41:1, compared with 1.31:1 in Kumamoto Prefecture, Japan, 1.49:1 in Uganda, 1.4:1 in Pakistan, and 0.98:1 in the USA, which is close to that of Pakistan, a country located in Central Asia, with a higher number of male children than female children, but a higher proportion of female children than male children in the USA [7,8,9,10]. This may be due to some differences in the incidence of certain types of tumors between different ethnic groups, for example, germ cell tumors are more prevalent in the East than in the West, and there are significant differences between men and women in the incidence of ependymal tumors, embryonal tumors, germ cell tumors, and pituitary tumors, which are more prevalent in pediatric patients [7, 8]. Research has shown that CNS tumors in pediatric patients can present at any age, with a peak incidence in the late preschool years, but some tumor subtypes, such as medulloblastoma, have a bimodal incidence [11,12,13,14], in this group of cases, male pediatric patients are predominantly distributed in the age group of 6 to 8 year age range, with a high incidence of the school-aged patient, while female pediatric patients are predominantly distributed in the age group of 12 to 14 years, with high age. Based on whom tumor grading criteria, the number of low-grade tumors is greater than the number of high-grade tumors in the 243 Uyghur pediatric cases collected, the number of pediatric patients in each age group is also variable, with a ratio of 1.31:1, and there is no clear pattern, among which the most affected children are 6–8 years old and 15–17 years old in the lower level, and the most affected pediatric patients are aged 3 to 5 years old in the upper tier, which may reflect characteristics of the age distribution of Uyghur children to some degree, this may be due to the polymorphism of tumor genes in children and prefer to entail site of tumors [4, 6, 15, 16]. In contrast, as the Chinese government pays greater attention to pediatric medicine, they tend to conduct annual routine medical examinations for school children, which greatly assists in the early detection and diagnosis of illnesses this also prevents some low-grade tumors in children from progressing to high-grade tumors.
In our group, the top 5 tumor subtypes are medulloblastoma in 42 cases (17.28%), ependymal tumors in 34 cases (14.00%), craniopharyngioma in 30 cases (12.35%), pilocytic astrocytoma in 28 cases (11.52%), and pituitary tumor in 10 cases (4.12%). Gliomas, medulloblastomas, ependymal tumors, germ cell tumors, and craniopharyngiomas are prevalent in Western countries, and astrocytoma, germ cell tumors, craniopharyngiomas, medulloblastomas, ependymal tumors are prevalent in Kumamoto Prefecture, Japan, gliomas, and embryonal tumors are prevalent in Pakistan [6, 7, 11, 17, 18]. This founding differs somewhat from data reported in Western countries and some Far Eastern nations. Specifically, pituitary tumors replaced germ cell tumors as one of the top 5 tumors with the highest prevalence, this may be because our hospital is located earlier in Xinjiang to perform endoscopic resection of pituitary tumors, which tends to be mature in terms of technology, and patients do not have to choose better medical units in mainland China, and patients from other cities in Xinjiang are more willing to visit our hospital, and therefore patients are more enriched as a result. Thus, geographic differences, ethnic differences, and local levels of medical technology levels may be the primary factors influencing the incidence of tumor types of CNS in pediatric patients.
According to recent reports, the predominant site of CNS tumors in pediatric patients is supratentorial, with the brain hemispheres and the saddle region being the most common sites [1, 10, 12], but some reports suggest that tumors in pediatric patients are more likely to be found inferiorly, with the fourth ventricle being the most common [8, 19]. There are 144 cases of supratentorial tumors in this group, of which 59 cases occur in the sella, 50 in the cerebral hemispheres, 18 cases in the lateral ventricles and the third ventricle, and 17 cases in the remainder. 86 cases of infratentorial tumors, including 63 cases in the fourth ventricle, 17 cases in the cerebellar hemispheres, 3 cases in the brainstem, 3 cases in the others, and 13 cases of tumors in the spinal canal, in this group of cases, supratentorial tumors are more common than infratentorial tumors than vertebral canal: 11.08:6.62:1, with supratentorial tumors being more common. It is possible that differences in the region of origin, ethnicity, age group, and local medical resources of the included children may result in different sites of predilection of CNS tumors in pediatric patients [20].
Several studies have reported that headache, nausea and vomiting, seizures, and abnormal vision are the most common presenting symptoms of CNS tumors in children, which may be related to the fact that pediatric painful CNS tumors tend to arise in midline structures and cause symptoms of obstructive hydrocephalus as the tumor grows in size, whereas clinical symptoms in children often tend to begin with the headache. In general, patients with headaches lasting less than 6 months, unresponsive to medication, increasingly severe headaches, personality changes, or associated with abnormal neurological examinations are considered to be at high risk for structural diseases [6, 8, 18, 21]. Most of our patients are from rural areas, so there are 167 (68.72%) cases of rural background and 76 (31.28%) from an urban background, parents of rural patients often have low levels of education and economic hardship, parents of our children and local medical clinics should therefore have sufficient knowledge of patients’ clinical manifestations to make accurate judgments and select the treatment needed to avoid diagnostic errors and waste of medical resources that increase the burden on patients’ parents. Although the overall incidence of brain and other CNS tumors is 11.7% higher in urban areas compared with rural areas in the USA [8], there are more cases in rural areas than in urban cases in this group. However, as of 2019, the urban population is beginning to increase significantly, which may be related to the development of urbanization in China and the decrease in population in rural areas, on the other hand, the rapid development of pediatric neurosurgery in our hospital has resulted in more affluent urban families opting to visit our hospital instead of other medical facilities in mainland China. Due to the new coronavirus outbreak in 2020, our hospital is primarily responsible for treating children in rural areas, and as a result, there are significantly fewer cases of children in urban areas.
Concluding
Despite the fact that our center is the largest comprehensive tertiary care hospital in Xinjiang, we are looking forward to multi-center, multi-disciplinary, and collaborative research with the greatest number of patients. Combining the geographical characteristics of Xinjiang and the demographic features of Uyghurs, to establish a reasonable diagnostic and treatment system and assessment criteria for tumors evaluation in Uyghur pediatric patients, and the improvement of epidemiological follow-up system is of great importance for improving the prognosis of pediatric CNS tumors in Uyghurs in China.
Data availability
A submission to the journal implies that materials described in the manuscript, including all relevant raw data, will be freely available to any researcher wishing to use them for non-commercial purposes, without breaching participant confidentiality. All clinical information of pediatric patients can be obtained from the Data Processing Center of the First Affiliated Hospital of Xinjiang Medical University.
References
Ullrich NJ, Pomeroy SL (2003) Pediatric brain tumors. J Neurol Clin 21(4):897–913
Walker D, Wilne S, Grundy R, Kennedy C (2016) A new clinical guideline from the Royal College of Paediatrics and Child Health with a national awareness campaign accelerates brain tumor diagnosis in UK children--"HeadSmart: Be Brain Tumour Aware". J Neuro Oncol 18(3):445–454
La Madrid AM, Kieran MW (2018) Epigenetics in clinical management of children and adolescents with brain tumors. J Curr Cancer Drug Targets 18(1):57–64
Duke ES, Packer RJ (2020) Update on Pediatric Brain Tumors: the Molecular Era and Neuro-immunologic Beginnings. J Curr Neurol Neurosci Rep 20(8):30
Warren KE (2004) NMR spectroscopy and pediatric brain tumors. J Oncologist 9(3):312–318
Pollack IF, Jakacki RI (2011) Childhood brain tumors: epidemiology, current management, and future directions. J Nat Rev Neurol 7(9):495–506
Makino K, Nakamura H, Yano S et al (2010) Population-based epidemiological study of primary intracranial tumors in childhood. J Childs Nerv Syst 26(8):1029–1034
Ostrom QT, Patil N, Cioffi G et al (2020) CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2013–2017. J Neuro Oncol 22(12 Suppl 2):iv1-iv96
Kadri H, Mawla AA, Murad L (2005) Incidence of childhood brain tumors in Syria (1993–2002). J Pediatr Neurosurg 41(4):173–177
Maaz AUR, Yousif T, Saleh A et al (2021) Presenting symptoms and time to diagnosis for Pediatric Central Nervous System Tumors in Qatar: a report from Pediatric Neuro-Oncology Service in Qatar. J Childs Nerv Syst 37(2):465–474
Glod J, Rahme GJ, Kaur H et al (2016) Pediatric Brain Tumors: Current Knowledge and Therapeutic Opportunities. J J Pediatr Hematol Oncol 38(4):249–260
de Robles P, Fiest KM, Frolkis AD et al (2015) The worldwide incidence and prevalence of primary brain tumors: a systematic review and meta-analysis. J Neuro Oncol 17(6):776–783
Wilne S, Collier J, Kennedy C et al (2007) Presentation of childhood CNS tumors: a systematic review and meta-analysis. J Lancet Oncol 8(8):685–695
Ostrom QT, Francis SS, Barnholtz-Sloan JS (2021) Epidemiology of Brain and Other CNS Tumors. J Curr Neurol Neurosci Rep 21(12):68
Akeret K, Staartjes VE, Vasella F et al (2020) Distinct topographic-anatomical patterns in primary and secondary brain tumors and their therapeutic potential. J J Neurooncol 149(1):73–85
Reichert JL, Chocholous M, Leiss U et al (2017) Neuronal correlates of cognitive function in patients with childhood cerebellar tumor lesions. J PLoS One 12(7):e0180200
Bouffet E (2000) Common brain tumors in children: diagnosis and treatment. J Paediatr Drugs 2(1):57–66
Riaz Q, Naeem E, Fadoo Z et al (2019) Intracranial tumors in children: a 10-year review from a single tertiary health-care center. J Childs Nerv Syst 35(12):2347–2353
Duffner PK (2007) Diagnosis of brain tumors in children. J Expert Rev Neurother 7(7):875–885
Wanner M, Rohrmann S, Korol D et al (2020) Geographical variation in malignant and benign/borderline brain and CNS tumor incidence: a comparison between a high-income and a middle-income country. J J Neurooncol 149(2):273–282
Harrup R, White VM, Coory M et al (2021) Treatment and Outcomes for Central Nervous System Tumors in Australian Adolescents and Young Adults: A Population-Based National Study. J J Adolesc Young Adult Oncol 10(2):202–208
Acknowledgements
Many thanks are due to colleagues from the Data Management Department of Xinjiang Medical University for providing the clinical data of pediatric patients.
Funding
Xinjiang Uygur Autonomous Region Natural Science Foundation Youth Project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by [Guofeng Fan], [Jia Zeng], [Xiaoyu Zhao], and [Cengjun Sheng]. The first draft of the manuscript is written by [Xuchao Wu] and [Dangmurenjiafu·Geng] and [Guohua Zhu] commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate.
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors have no competing interests to declare relevant to this article’s content.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, X., Dangmurenjiafu·Geng, Fan, G. et al. Epidemiology of pediatric central nervous system tumors in Uyghur: experience from a single center. Childs Nerv Syst 39, 909–914 (2023). https://doi.org/10.1007/s00381-022-05766-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05766-3