Abstract
Introduction
ERF mutation is one of the most recently identified genetic aberrations associated with syndromic craniosynostosis. Data on the pattern of craniosynostosis, surgical management of ERF-related craniosynostosis and outcomes is limited. We report on our single-centre experience in paediatric cohort of patients with syndromic craniosynostosis secondary to ERF mutation.
Methods
A retrospective review of all paediatric craniofacial cases was performed over an 8-year period (2014–2022). All patients with genetically confirm ERF-related craniosynostosis were identified, and clinical parameters including, age, sex, pattern of craniosynostosis, associated tonsillar herniation and follow-up period were further analysed from electronic clinical and imaging systems. All patients were selected and discussed in multidisciplinary craniofacial meeting (composed of neurosurgical, maxillofacial, plastics and genetics teams) prior to any surgical intervention.
Results
Overall, 10 patients with ERF-related craniosynostosis were identified with a male-to-female ratio of 4:1 with mean age at the time of surgery of 21.6 months with a mean follow-up period of 5.2 years. ERF-confirmed cases led to variable craniosynostosis pattern with multi-sutural synostosis with concurrent sagittal and bilateral lambdoid involvement as the most common pattern (7/10). No patient pre-operatively had evidence of papilloedema on ophthalmological assessment. Eight out of 10 patients had associated low-lying tonsils/hind brain hernia pre-operatively. Eight out of 10 patients required surgery which included 2 fronto-orbital advancement, 3 calvarial remodelling, 2 posterior calvarial remodelling/release and 1 insertion of ventriculoperitoneal shunt.
Conclusion
Involvement of sagittal and lambdoid sutures is the most common pattern of craniosynostosis. ERF-related craniosynostosis can have variable pattern of suture fusion, and management of each patient requires unique surgical planning and execution based on clinical needs for the optimal outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
ERF gene, coding for ETS2 repressor factor (ERF) is a member of the ETS family of transcription factors, and mutations in ERF can lead to syndromic forms of craniosynostosis. This gene is mapped to chromosome 19q13.2 with autosomal dominant pattern of inheritance.
Syndromic craniosynostosis caused by ERF gene is also associated with facial dysmorphism, low-lying cerebellar tonsils, speech and language delay and learning difficulties and/or behavioural problems [1,2,3,4]. The overall prevalence of ERF mutations is estimated to be around 2% in patients with syndromic craniosynostosis and 0.7% in clinically nonsyndromic craniosynostosis [5].
ERF-related craniosynostosis has been shown to create a varied pattern of suture fusion with multi-suture involvement as the most common presentation [1, 6]. A significant number of these patients have previously been diagnosed as suspected other syndromes, but with increasing understanding of ERF-related features, correct diagnosis is being established.
Best surgical strategy and optimal management in this group of patients is not well defined in the literate with paucity of information on outcomes and rate of restenosis. We undertook this retrospective study to further elucidate features of ERF-related craniosynostosis and surgical-specific management in this cohort of patients.
Methods
A retrospective review of all paediatric craniofacial cases was performed over an 8-year period (2014–2022). All patients with genetically confirm ERF-related craniosynostosis were selected, and clinical parameters including age, sex, pattern of craniosynostosis, age at the time of surgery, associated tonsillar herniation and syrinx, follow-up period and clinical outcomes were further interrogated from available electronic clinical and imaging systems. Computed tomography (CT) head 3D reconstructions were used for the assessment of the pattern of craniosynostosis, and magnetic resonance imaging (MRI) brain and spine images were used for the determination of tonsillar descent and spinal syrinx. All patients were selected and discussed in multidisciplinary craniofacial meeting (composed of neurosurgical, maxillofacial, plastics and genetics team) prior to any surgical intervention. As part of our craniofacial service, all suspected syndromic or multi-suture cases were offered genetic testing and screened for mutations in ERF gene as well as other more common mutations observed in syndromic craniosynostosis.
Results
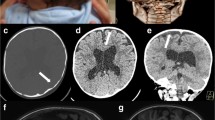
Overall, 10 cases of ERF-related craniosynostosis were identified over an 8-year period. The male-to-female ratio in this cohort was 8:2 (M:F = 4:1). The main reason for presentation to craniofacial services was due to dysmorphic appearance and cranial shape. Ophthalmological assessment in all patients did not reveal any gross papilloedema pre-operatively. Eight out of 10 patients in this cohort had evidence of hind brain hernia/cerebellar tonsillar descent. Interestingly, no associated syrinx was identified in any of cases. Five out of 10 patients had evidence of ventriculomegaly. Six out of 10 patients demonstrated evidence of copper beaten skull appearance on radiographs or lacunae/calvarial defects on CT head likely from chronic raised intracranial pressure (Fig. 1).
A 3D CT reconstruction of the skull in a patient with ERF-related craniosynostosis demonstrating lacunae/bony defects and evidence of fusion of the posterior sagittal and superior third of bilateral lambdoid sutures. B Skull X-ray radiograph demonstrating copper beaten appearance reflecting longstanding raised intracranial pressure in ERF-related craniosynostosis despite no papilloedema pre-operatively
Multi-sutural craniosynostosis was the most common observed pattern of craniosynostosis with concurrent sagittal and lambdoid fusion being the most frequent (7/10). Eight out of 10 patients required surgical intervention with 2 patients treated conservatively. Indication for surgery included abnormal head shape, evidence of chronic raised intracranial pressure such as copper beaten skull appearance and lacunae/bone defects and suture diasthesis. The mean age at the time of surgery was 21.6 months. Of 8 patients undergoing surgery, 7 required craniofacial/calvarial modifying surgeries including 2 fronto-orbital advancement, 3 calvarial remodelling and 2 posterior calvarial remodelling/release. One patient required ventriculoperitoneal shunt only due to the presence of hydrocephalus due to venous sinus hypertension.
The mean follow-up period in this cohort was 5.2 years. Of patients with long-term follow-up MRI imaging, 1 case showed improvement in low-lying tonsils. Three patients had no further descent with stabilisation, 2 patients showed progression of tonsillar descent over the follow-up period despite surgery, and 2 patients did not have long-term follow-up imaging available.
Two cases with progression of “Chiari” and tonsillar descent were both cases operated at very young age. One of these currently is awaiting posterior calvarial distraction for further progression of Chiari with worsening ventriculomegaly (Fig. 2). The remaining patient with progression of Chiari is being monitored closely with regular clinical and radiological follow-up. Detailed characteristics of each ERF patient and surgical management is summarised in Table 1.
A–B 3D CT reconstruction of the skull for a patient with posterior sagittal and bilateral partial lambdoid fusion at age of 22 days. C Sagittal T2-weighted MRI brain demonstrating mild tonsillar descent in this patient with ERF-related craniosynostosis at age of 3 months. D Sagittal T2-weighted MRI brain at 14 months of age demonstrating progression of tonsillar descent over time despite surgery at age of 4 months
Discussion
ERF-related craniosynostosis was first described in 2013 in 12 unrelated families accounting for 7.1% of a cohort of 127 patients with undiagnosed clinically syndromic craniosynostosis and 2.9% of a total cohort of 412 undiagnosed patients with syndromic or nonsyndromic craniosynostosis [4]. Over the past 8 years, there has been increasing number of identified ERF-related cases of craniosynostosis leading to better understanding of this subset of craniosynostosis patients. In addition to multi-sutural craniosynostosis, this genetic aberration has been associated with facial dysmophism, low-lying cerebellar tonsils/Chiari, behavioural problems and language and speech delay [1, 4].
ERF-related craniosynostosis can present with variable multi-sutural sutural synostosis [1, 7]. Posterior sagittal and bilateral lambdoid with or without coronal suture involvement appears to be the most common pattern of craniosynostosis [1]. Our results are consistent with other studies with 70% of patients in our cohort having evidence of posterior sagittal and bilateral lambdoid involvement.
Although ERF-related craniosynostosis has many features of other syndromic craniosynostosis cases, ERF cohort differs in some aspects which maybe unique. Firstly, patients with ERF-related craniosynostosis do not appear to have evidence of gross papilloedema on presentation with the same frequency seen in other syndromic craniosynostosis types such as Crouzon or Pfeiffers. Reasons for this is unclear although may represent early presentation of these patients to craniofacial services prior to development of gross papilloedema or suture diasthesis and presence of calvarial lacunae and defects compensating for raised intracranial pressure to some extent.
Unlike other syndromic causes of craniosynostosis, the so-called Chiari or cerebellar tonsillar descent appears to be much more frequently observed, although interestingly this is not associated with syrinx. This maybe a further difference compared to other syndromic craniosynostosis, whereby syrinx can be seen associated with low-lying tonsils frequently. It is unclear if Chiari in ERF-related cases is truly a primary Chiari or secondary to raised intracranial pressure or combination of these two.
Surgical management of ERF-related craniosynostosis is dictated by sutures involved with those involving metopic requiring anterior augmenting procedures such as fronto-orbital advancement and those with multi-sutural involvement and significant low-lying cerebellar tonsils and fusion of posterior sagittal and bilateral lambdoid sutures requiring vault expansion/calvarial remodelling or posterior augmenting procedures. Two cases in our cohort showed evidence of progression of tonsillar descent over the course of follow-up, and both occurred in patients undergoing surgery at a very young age with evidence of bone reformation and re-synostosis. This may be due to surgical intervention at young age and associated higher risk of re-synostosis. Careful attention to combination of sutures involved would allow selection of best surgical approach. Additionally, cases with no features of raised intracranial pressure and asymptomatic can be treated conservatively as were 2 cases in our cohort.
This study has a number of limitations including retrospective nature of study, small number of cohort and short follow-up period. Increasing understanding and reporting on features of this subset of craniosynostosis patients and outcomes will allow better characterisation and optimisation of surgical management for this cohort of patients. Longer follow-up data is required to elucidate long-term effects of surgical intervention and impact on tonsillar descent and cognitive outcomes in this group of patients.
Conclusion
ERF-related craniosynostosis represents a newly recognised subset of patients with varied craniosynostosis pattern and poses unique surgical challenges. Longer follow-up is required to allow optimisation of surgical management in this cohort of patients.
Data availability
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- CSF:
-
Cerebrospinal fluid
- MRI:
-
Magnetic resonance imaging.
References
Glass GE, O’Hara J, Canham N, Cilliers D, Dunaway D, Fenwick AL, Jeelani NO, Johnson D, Lester T, Lord H, Morton JEV, Nishikawa H, Noons P, Schwiebert K, Shipster C, Taylor-Beadling A, Twigg SRF, Vasudevan P, Wall SA, Wilkie AOM, Wilson LC (2019) ERF-related craniosynostosis: the phenotypic and developmental profile of a new craniosynostosis syndrome. Am J Med Genet A 179(4):615–627
Care H, Luscombe C, Wall SA, Dalton L, Johnson D, Wilkie AOM (2022) Cognitive, behavioural, speech, language and developmental outcomes associated with pathogenic variants in the ERF gene. J Craniofac Surg
Moddemann MK, Kieslich M, Koenig R (2022) Intrafamilial variability in six family members with ERF-related craniosynostosis syndrome type 4. Am J Med Genet A
Twigg SR, Vorgia E, McGowan SJ, Peraki I, Fenwick AL, Sharma VP, Allegra M, Zaragkoulias A, Sadighi Akha E, Knight SJ, Lord H, Lester T, Izatt L, Lampe AK, Mohammed SN, Stewart FJ, Verloes A, Wilson LC, Healy C, Sharpe PT, Hammond P, Hughes J, Taylor S, Johnson D, Wall SA, Mavrothalassitis G, Wilkie AO (2013) Reduced dosage of ERF causes complex craniosynostosis in humans and mice and links ERK1/2 signaling to regulation of osteogenesis. Nat Genet 45(3):308–313
Wilkie AOM, Johnson D, Wall SA (2017) Clinical genetics of craniosynostosis. Curr Opin Pediatr 29(6):622–628
Körberg I, Nowinski D, Bondeson ML, Melin M, Kölby L, Stattin EL (2020) A progressive and complex clinical course in two family members with ERF-related craniosynostosis: a case report. BMC Med Genet 21(1):90
Chaudhry A, Sabatini P, Han L, Ray PN, Forrest C, Bowdin S (2015) Heterozygous mutations in ERF cause syndromic craniosynostosis with multiple suture involvement. Am J Med Genet A 167A(11):2544–2547
Author information
Authors and Affiliations
Contributions
Fardad Afshari has collected the data and written the article. Pasquale Gallo, Ahad Shafi, Jaime Grant, Amy Drew, Peter Noons, Jagajeevan Jagadeesan, Martin Evans and Helen Brittain have contributed to editing and data collection under the supervision of Desiderio Rodrigues.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Appropriate consent has been obtained.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Afshari, F.T., Gallo, P., Shafi, A. et al. ERF-related craniosynostosis and surgical management in the paediatric cohort. Childs Nerv Syst 39, 983–988 (2023). https://doi.org/10.1007/s00381-022-05700-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05700-7