Abstract
Purpose
Multiple imaging parameters have been examined to estimate the presence of syrinx and the need for surgery in Chiari I patients (CM1); however, no consistent or definitive criteria have been proposed. The objective of this study was to review existing and identify novel radiological and clinical characteristics of CM1 patients that associate syrinx development and surgical intervention.
Methods
Patients with Chiari I malformation diagnosed on imaging between 0 and 18 years were retrospectively reviewed from January 1, 2007 to February 12, 2020. Participants were included if they had a baseline MRI of the head and spine prior to surgical intervention if required. Forty age-matched controls with cranial imaging were identified for comparison. Imaging parameters and clinical symptoms were recorded.
Results
A total of 122 CM1 patients were included in this study. Of the 122 patients, 28 (23%) had syrinx, and 27 (22%) had surgery. The following imaging parameters associated with syrinx and surgical intervention were identified: midbrain length (P < 0.001; P = 0.032), the obex position (P = 0.002; P < 0.001) and medullary kinking (P = 0.041; P < 0.001). Among the clinical features, the presence of overall pain (P = 0.017; P = 0.042), neck pain (P = 0.005; P = 0.027), and sensory dysfunction (P < 0.001) were found to be strongly associated with syrinx and surgery.
Conclusion
While further investigation is needed, these specific radiological and clinical parameters should be considered when evaluating CM1 patients and may be used to guide further management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
CM1 is a radiologic diagnosis that has traditionally been defined as tonsillar descent of 5 mm or more below the foramen magnum (FM) [1, 2]. This finding is often detected incidentally on neuroimaging studies, with literature showing an incidence of 3.6% in children [3, 4]. CM1 can cause debilitating symptoms, including posterior headache and/or neck pain, ataxia, dysphagia, scoliosis, or sensory and motor deficits [5, 6]. Although clinical pathophysiology is poorly understood, symptoms are thought to be related to obstruction of CSF flow across the craniocervical junction with or without spinal cord syrinx formation [7, 8]. The estimated prevalence of syringomyelia is 40% in pediatric CM1 patients [3]. The pathogenesis of syringomyelia in CM1 remains largely unknown and multiple theories have been proposed [9].
In many centers, posterior fossa decompression (PFD) is indicated in CM1 patients presenting with syringomyelia to prevent progression and potential development of neurologic deficit. Once neurologic deficit develops, even with surgical intervention, it may only stabilize and not necessarily resolve. Therefore, early recognition is required to minimize the possibility of developing deficits [10]. While authors of previous studies have proposed multiple imaging and clinical parameters that are indicative of syrinx development and the need for surgery in CM1 patients, no definitive guidelines or criteria have been consistently utilized [11–15]. The aim of this study was to identify radiological and clinical parameters in pediatric CM1 patients that may be used to indicate the development of syrinx and/or surgical intervention.
Materials and methods
Patient population
This is a retrospective study of patients between 0 and 18 years old with a diagnosis of CM1. Participants were included only if they had a baseline MRI of the head and spine between January 1, 2007, and February 12, 2020, prior to surgical intervention (if required). Patients with syndromic features noted on imaging or clinical history were excluded (Fig. 1). Age-matched normal controls without tonsillar ectopia were identified among children who underwent MRI of the brain during the same period. MRI of the spine was not available for most control patients. During the study period, patients underwent surgical intervention only if they experienced clinical symptoms that were thought to be related to their Chiari I malformation and did not undergo surgery for radiographic findings alone if they were clinically asymptomatic.
Cases were identified through a search in the Epic electronic health record system. The diagnosis of Chiari I malformation was confirmed by chart review of clinical and imaging data. The study was approved by the Research Ethics Board at the Children’s Hospital of Eastern Ontario (CHEO).
Imaging data
Patients underwent MRI of the head and spine using a 1.5 Tesla magnet (Signa HDxt/GE Healthcare) or a 3 Tesla magnet (Magnetom Skyra/Siemens Healthineers). The following sequences were used for evaluating the radiological criteria in the brain: sagittal T2 thin weighted sequence, coronal 3D T1 weighted sequence with sagittal and axial reformats, and dynamic CSF flow sequence when available. The following sequences were used for evaluating the radiological criteria in the spine: sagittal T2 weighted sequence of the full spine, axial T2 weighted sequence of the full spine, and axial T1 weighted sequence of the lower spine. The presence of scoliosis was assessed on the sagittal T2 sequence of the full spine and posteroanterior (PA) radiograph of the spine whenever available. The images were reviewed in consensus by three investigators (MD, NG, and NW). Imaging measurements collected are shown in Figs. 2 and 3.
Radiological measurements acquired. A, B, and C Sagittal 3D T1 MR sequence of the brain. Length of the clivus (A), length of the foramen magnum (B), length of the supraocciput (C), position of the obex (D), length of the herniated tonsils (E), length of the vermis (F), length of the midbrain (G), retroflexion angle (H), retroversion angle (I), whole tonsillar length (J), occipital protuberance angle (K), cerebellar tentorium angle (L), base of the skull angle (M), and pB-C2 line (N)
Clinical evaluation
The patient’s clinical charts were reviewed for the presence or absence of specific symptoms, including headaches, facial movement dysfunction, brainstem dysfunction, apnea, ocular dysfunction, sensation dysfunction, auditory dysfunction, tongue movement, dysphagia, swallowing abnormality, corporal motor and sensory dysfunction, and bladder/bowel dysfunction. Clinical data were reviewed by two investigators (CO and AT). When clinical information was not included in the chart, it was indicated as not available.
Statistical analysis
All radiological features are expressed as means with standard deviations for continuous variables and as frequencies with percentages for discrete variables. Radiological features between the groups were compared using the Wilcoxon rank sum for continuous variables and Fisher’s exact test for discrete variables. Two-sided P-values less than 0.05 were considered statistically significant. Statistical analysis was carried out using R version 4.0.2 [16]. Holm’s adjustment for multiple testing was performed [17].
Results
A total cohort of 122 CM1 patients was included in this study (Table 1). The average duration of follow-up for Chiari I patients from the first to the last clinical visit was 48 months (± 41.1 SD), and the average time between the first and last MRI was 47 months (± 36.9 SD). A total of 54.9% of the CM1 patients were male. Of the 122 patients, 28 (23%) were found to have a syrinx and 27 (22%) underwent surgery. A total of 10 patients (37%) had only craniocervical decompression and 17 patients (63%) had craniocervical decompression with duroplasty. A total of 5 patients (4%) in our cohort needed more than one surgical intervention due to new symptomatology, for example, occipital headaches or increased intracranial pressure. A total of 40 control patients were included, in whom the main indication for brain MRI was headaches (85%). Most of these headaches were diffuse (37.5%) or frontal (20%) in location. Cervical (10%) and occipital headaches (10%) were less common. Other diagnoses included prematurity, hallucinations, and atypical syncope. MRI of the brain in all control patients was normal.
Radiological variables associated with syrinx
The statistically significant radiological variables associated with the presence of syrinx are shown in Table 2. When comparing patients with CM1 presenting with syrinx to those without, the midbrain length was found to be increased (mean 13.9 mm, SD 1.4 vs mean 12.8 mm, SD 1.6; P < 0.001) as well as having a longer supraocciput length (40.36 mm, SD 5.3 vs 37.99 mm, SD 5.2; P = 0.026), greater retroversion of the dens (69.2° vs 75.2°; P = 0.006) and an obex position below the foramen magnum (57.1% vs 24.5%; P < 0.001) (Fig. 4). The presence of scoliosis (P < 0.001), medullary kinking (P = 0.041), and prominence of the central canal (P = 0.032) were significantly more common in CM1 patients with syringomyelia compared to CM1 patients without syringomyelia. Of the CM1 patients identified with the prominence of the central canal (n = 30) at baseline, 11 had already developed syrinx (36.6%), 3 remained stable and did not develop syrinx (10%), 8 had no follow-up (26.6%), 3 had resolved (10%), and 5 patients (16.6%) developed syrinx at follow up.
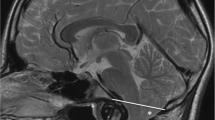
A Sagittal T1WI of the brain. Features of Chiari I malformation, including a short clivus (white star), retroversion of the dens (thick white arrow), herniation of the cerebellar tonsils (gray arrow with black outline), position of the obex below the foramen magnum (white dashed arrow), and kinking of the medulla (thin white arrow). B, C Sagittal T2WI of the upper spine. Presence of an associated syrinx (white star with black outline) involving the cervical, thoracic, and lumbar spinal cord
In contrast, whole tonsillar length, length of the herniated tonsils, clivus length, length of the foramen magnum, the low-lying position of the conus, and the presence of fatty filum were found to be statistically different in CM1 patients in comparison to controls but were not associated with a syrinx in patients with CM1 (Table 2).
There was no statistically significant association observed in the remaining radiological parameters with CM1 or syrinx formation, including skull base angle, pB-C2 length, basilar invagination, atlantooccipital fusion, retroflexion of the dens, vermis length, and occipital protuberance angle.
Radiological variables associated with surgery
When comparing patients with CM1 who did and did not undergo surgery (Table 3), the presence of syrinx was identified as an indication for surgery (P < 0.001); however, differences in syrinx dimension were not statistically significant (P = 0.310). The mean whole tonsillar length (37.30 mm vs 32.92 mm; P = 0.005) and the length of the herniated tonsils (14.67 mm vs 10.40 mm; P < 0.001) were found to be increased in CM1 patients that underwent surgery when compared to conservatively managed patients. The presence of medullary kinking (51.9% vs 9.5%; P < 0.001) and obex position below the foramen magnum (70.4% vs 21.1%; P < 0.001) were also found to be strongly associated with surgery. The midbrain length was found to be increased in CM1 patients with surgery (P = 0.025), with a mean value of 13.57 mm (± 1.75 SD) in the surgery group, compared to 12.90 mm (± 1.50 SD) in the no surgery group. Also, when evaluated together, obex position, midbrain length, and medullary kinking were more strongly associated with surgery (P = 0.006) compared to midbrain length alone.
A greater clivus length (P < 0.001), shorter FM length (P = 0.029), shorter supraocciput length (P < 0.001), prominent central canal (P < 0.001), scoliosis (P < 0.001), low-lying conus (P < 0.001), and fatty filum (P < 0.001) were found to be more common in CM1 than control patients. However, these variables were not indicative of surgical intervention in CM1 patients.
Clinical features associated with syrinx
The statistically significant clinical criteria in CM1 patients with syrinx compared to CM1 patients without syrinx and controls are shown in Table 4. Among the evaluated clinical characteristics, patients with CM1 and syrinx were distinguished by the presence of overall body pain (P = 0.010), neck pain (P = 0.005), and sensory dysfunction (P < 0.001) when compared to CM1 patients without a syrinx. Headaches that were diffuse (P < 0.001) in location were more frequently seen in controls and CM1 patients without syrinx in comparison to CM1 patients with syrinx. Headaches requiring medication to alleviate them were more common in CM1 patients when compared to controls (P = 0.030). The presence of lower back pain (P = 0.040) and motor dysfunction (0.040) were found to be more common in CM1 patients in comparison to controls. However, there was no statistically significant difference between the CM1 patients with or without syrinx.
Clinical features associated with surgery
A comparison of clinical features between patients who underwent surgery, patients who were managed conservatively, and controls are seen in Table 5. The presence of occipital headaches (P = 0.007), overall pain (P = 0.042), neck pain (0.027), apnea (0.007), swallowing abnormality (0.007), motor dysfunction (P = 0.027), and sensation dysfunction (P < 0.001) were found to be indications for surgery. The absence of pain was more commonly associated with CM1 patients managed conservatively (P = 0.042) and control patients (P = 0.001).
Discussion
Several studies have attempted to evaluate different radiological and clinical parameters in patients with CM1, syringomyelia, and the need for surgical intervention [13, 14, 18,19,20,21,22,23]. Obex position, retroversion angle of the dens, scoliosis, and medullary kinking have also been previously reported [13, 14, 21, 24, 25]. Tubbs et al. hypothesized that a posteriorly inclined den in CM1 displaces the brainstem posteriorly at the level of the obex and inhibits egress of CSF into the subarachnoid space, thereby propelling it into the spinal cord (a mechanism of syrinx formation proposed by Gardner and Angel) [26]. An inferiorly displaced brainstem and consequently obex would also contribute to the obstruction at the craniocervical junction [27]. As Greitz’s group hypothesized, when there is obstruction of the subarachnoid space at the level of the FM, there is a dysregulation of pressures between the subarachnoid space and the spinal cord [28]. Impaired absorption of CSF through the intramedullary venous channels subsequently leads to fluid accumulation and central canal dilation, resulting in syrinx formation [29]. Craniovertebral junction abnormalities including a short clivus, a decreased length of the foramen magnum, and an increased angle of the cerebellar tentorium have been described in patients in Chiari I. However, its correlation with syringomyelia or surgery remains unclear [11, 13, 18].
Our results are concordant with what has been described in the literature, associating tonsillar length, medullary kinking, and obex position with the need for surgery [11, 14, 21, 24, 30, 31]. In a recent study, Alford et al. concluded that these imaging criteria may be directly linked to the development and progression of symptoms [11]. Haller et al. proposed that when tonsil position and obex position were combined, they were better associated with the use of PFD than when evaluated independently. The association of tonsillar descent with syringomyelia, however, remains controversial in the literature [15, 21, 32]. Our results emphasize that tonsillar ectopia alone does not associate with syrinx development, but rather the constellation of findings that may be seen with tonsillar descent. Other radiological parameters such as atlas assimilation, supraocciput length, angle of the cerebellar tentorium, length of the foramen magnum, and pB-C2 distance have not been strongly associated with surgery in the literature, which is parallel to our findings [11, 12].
The presence of syrinx has been independently associated with surgical intervention in previous studies, which correlates with our results [11, 14, 33,34,35]. Treatment for syringomyelia in patients with CM1 is largely restricted to surgical intervention in the form of PFD. In most cases, syringomyelia will resolve after PFD; however, some studies have reported a progression of syrinx and symptoms even after PFD. Of note, cases of spontaneous resolution of the syrinx without surgical intervention have been described. These inconsistencies emphasize that there is still much to be understood about the relationship between CM1 and syringomyelia [36, 9].
The association between central canal prominence and syringomyelia has been controversial in the literature [37]. 16.6% of the CM1 patients identified with the prominence of the central canal in our cohort at baseline developed syrinx on follow-up imaging. Our results support the theory that a prominent central canal might be the site for the initial accumulation of fluid during syrinx cavity pathogenesis in children with CM1 [31, 37, 38]. Milhorat et al. also concluded that differences in canal patency can affect the development of syringomyelia in patients with hindbrain herniation [39].
In our study, midbrain length was found to be strongly associated with syrinx and surgery. Elongation of the midbrain has been described in Chiari II malformation [20, 40, 41]. However, little is known about the morphology of the midbrain in patients with CM1. Rare cases of midbrain deformity associated with CM1 have been reported in the literature [42], but morphometry of the midbrain has not been previously evaluated before in patients with Chiari I malformation. It is known that elongation of the medulla and fourth ventricle occurs in patients with caudal migration of the obex below the foramen magnum, an entity known as Chiari malformation 1.5 [20]. Although the pathophysiology of CM1 is still poorly understood, one leading hypothesis is that overcrowding of the hindbrain occurs secondary to underdevelopment of the occipital bone, resulting in obstruction of the CSF flow [20, 43]. We infer that these mechanical factors may contribute to caudal migration of the brainstem as well. Perhaps a longer midbrain length predisposes one to develop symptomatic Chiari I malformation by increasing the likelihood of foramen magnum and CSF flow obstruction. The lower position of the obex, in combination with the descended tonsils, may be more prone to compression and outflow obstruction during periods of vascular engorgement of the tonsils, such as with the Valsalva maneuver or straining [20], which has been emphasized in the theories proposed by Tubbs et al., Gardner and Angel, and Greitz’ group in the development of syrinx and likelihood of having surgery [29, 26–28]. However, this finding needs to be taken with caution and it should be assessed in future studies to determine its significance.
Pain or headache within the occipital region is the most common presenting symptom in children and adults with CM1, which is concordant with our results [8, 5, 22, 44, 45]. Intractable occipital headaches and neck pain are common indications for surgery [1]. Occipital headaches have also been correlated with obex position [14]. Both occipital headaches and neck pain were significantly associated with the need for surgery in our study. Several authors have also described the correlation of pain with syringomyelia, [27, 46, 47] however, little is known about the location and characteristics of pain in patients with CM1 and syrinx. In our study, the presence of pain, particularly neck pain, was statistically associated with the presence of syrinx.
There are several limitations to our study. First, this is a retrospective study limited to a single center, which introduces the possibility of bias. Second, not all the MR studies included in our study had the same imaging protocol; for example, sagittal T2 sequence of the brain was not included in all the reviewed MRIs. Third, our moderate sample size resulted in a relatively small number of patients with a syrinx who underwent surgery. Lastly, the main indication for an MRI in control patients was headaches, which might have led to a bias when comparing the presence of headaches in CM1 patients versus controls.
Conclusion
Our study investigates radiological and clinical features of CM1 associated with syrinx and surgery. While further research is needed, these results suggest that the length of the herniated tonsils is not the only parameter to consider when evaluating patients with CM1. The obex position, the presence of syrinx, and medullary kink should be included as radiological parameters when evaluating CM1 patients and may be useful to guide clinical management. Furthermore, midbrain length is a novel criterion to consider, however, its significance will need to be assessed in future studies. The presence of neck pain, occipital headaches, apnea, swallowing abnormality, and motor and sensory dysfunction should be considered clinical parameters. These features may be used to identify patients at risk of developing syrinx, prompt further investigation for syrinx, and evaluate the need for surgery. These results warrant assessment and replication in larger prospective studies.
References
Alexander H, Tsering D, Myseros JS, Magge SN, Oluigbo C, Sanchez CE, Keating RF (2019) Management of Chiari I malformations: a paradigm in evolution. Child Nerv Syst. https://doi.org/10.1007/s00381-019-04265-2
Barkovich AJ, Wippold FJ, Sherman JL, Citrin CM (1986) Significance of cerebellar tonsillar position on MR. AJNR Am J Neuroradiol 7:795–799
Arnautovic A, Splavski B, Boop FA, Arnautovic KI (2015) Pediatric and adult Chiari malformation type I surgical series 1965–2013: a review of demographics, operative treatment, and outcomes. J Neurosurg Pediatr. https://doi.org/10.3171/2014.10.PEDS14295
Chatrath A, Marino A, Taylor D, Elsarrag M, Soldozy S, Jane JA (2019) Chiari I malformation in children—the natural history. Child’s Nervous System. https://doi.org/10.1007/s00381-019-04310-0
McClugage SG, Oakes WJ (2019) The Chiari I malformation. J Neurosurg Pediatr. https://doi.org/10.3171/2019.5.PEDS18382
Pepper J, Elhabal A, Tsermoulas G, Flint G (2020) Symptom outcome after craniovertebral decompression for Chiari type 1 malformation without syringomyelia. Acta Neurochir. https://doi.org/10.1007/s00701-020-04631-z
Shoja MM, Tubbs RS, Oakes WJ (2013) Embryology and pathophysiology of the Chiari I and II malformations. In: The Chiari Malformations. Springer New York, New York, NY
Steinbok P (2004) Clinical features of Chiari I malformations. Child Nerv Syst. https://doi.org/10.1007/s00381-003-0879-x
Holly LT, Batzdorf U (2019) Chiari malformation and syringomyelia. J Neurosurg Spine. https://doi.org/10.3171/2019.7.SPINE181139
Attal N (2004) Effects of surgery on the sensory deficits of syringomyelia and predictors of outcome: a long term prospective study. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp.2003.026674
Alford EN, Atchley TJ, Leon TJ, Laskay NMB, Arynchyna AA, Smith BP, Aban I, Johnston JM, Blount JP, Rozzelle CJ, Oakes WJ, Rocque BG (2021) Imaging characteristics associated with surgery in Chiari malformation type I. J Neurosurg Pediatr. https://doi.org/10.3171/2020.9.PEDS20347
Atchley TJ, Alford EN, Rocque BG (2020) Systematic review and meta-analysis of imaging characteristics in Chiari I malformation: Does anything really matter? Child Nerv Syst. https://doi.org/10.1007/s00381-019-04398-4
Gad KA, Yousem DM (2017) Syringohydromyelia in patients with Chiari i malformation: a retrospective analysis. Am J Neuroradiol 38:1833–1838. https://doi.org/10.3174/ajnr.A5290
Haller G, Sadler B, Kuensting T, Lakshman N, Greenberg JK, Strahle JM, Park TS, Dobbs MB, Gurnett CA, Limbrick DD (2020) Obex position is associated with syringomyelia and use of posterior fossa decompression among patients with Chiari I malformation. J Neurosurg Pediatr. https://doi.org/10.3171/2020.2.PEDS19486
Stovner LJ, Rinck P (1992) Syringomyelia in Chiari malformation. Neurosurgery. https://doi.org/10.1227/00006123-199211000-00013
R Core Team (2020) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Holm S (1979) A simple sequentially rejective multiple test procedure. Scand J Stat 6:65–70
Al-Habib A, al Abdulsalam H, Ahmed J, Albadr F, Alhothali W, Alzahrani A, Abojamea A, Altowim A, Ullah A, Alkubeyyer M (2020) Association between craniovertebral junction abnormalities and syringomyelia in patients with chiari malformation type-1. Neurosciences 25:308–315. https://doi.org/10.17712/nsj.2020.4.20200008
Halvorson KG, Kellogg RT, Keachie KN, Grant GA, Muh CR, Waldau B (2016) Morphometric analysis of predictors of cervical syrinx formation in the setting of Chiari I malformation. Pediatr Neurosurg. https://doi.org/10.1159/000442991
Hiremath SB, Fitsiori A, Boto J, Torres C, Zakhari N, Dietemann JL, Meling TR, Vargas MI (2020) The perplexity surrounding chiari malformations - are we any wiser now? Am J Neuroradiol 41:1975–1981
Strahle J, Muraszko KM, Kapurch J, Bapuraj JR, Garton HJL, Maher CO (2011) Chiari malformation type I and syrinx in children undergoing magnetic resonance imaging: Clinical article. J Neurosurg Pediatr 8:205–213. https://doi.org/10.3171/2011.5.PEDS1121
Wu YW, Chin CT, Chan KM, Barkovich AJ, Ferriero DM (1999) Pediatric Chiari I malformations: do clinical and radiologic features correlate? Neurology. https://doi.org/10.1212/WNL.53.6.1271
Yan H, Han X, Jin M, Liu Z, Xie D, Sha S, Qiu Y, Zhu Z (2016) Morphometric features of posterior cranial fossa are different between Chiari I malformation with and without syringomyelia. Eur Spine J 25:2202–2209. https://doi.org/10.1007/s00586-016-4410-y
Milhorat TH, Chou MW, Trinidad EM, Kula RW, Wolpert C, Speer MC (1999) Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients
Tubbs RS, Iskandar BJ, Bartolucci AA, Oakes WJ (2004) A critical analysis of the Chiari 1.5 malformation. J Neurosurg Pediatr 101. https://doi.org/10.3171/ped.2004.101.2.0179
Tubbs RS, Wellons JC, Blount JP, Grabb PA, Oakes WJ (2003) Inclination of the odontoid process in the pediatric Chiari I malformation. J Neurosurg Spine. https://doi.org/10.3171/spi.2003.98.1.0043
Tubbs RS, Lyerly MJ, Loukas M, Shoja MM, Oakes WJ (2007) The pediatric Chiari I malformation: a review. Child Nerv Syst. https://doi.org/10.1007/s00381-007-0428-0
Sandoval-Garcia C, Iskandar BJ (2013) Research on the pathophysiology of Chiari I-related symptoms and syringomyelia, with emphasis on dynamic MRI techniques. In: The Chiari Malformations. Springer New York, New York, NY
Koyanagi I, Houkin K (2010) Pathogenesis of syringomyelia associated with Chiari type 1 malformation: Review of evidences and proposal of a new hypothesis. Neurosurg Rev. https://doi.org/10.1007/s10143-010-0266-5
Bollo RJ, Riva-Cambrin J, Brockmeyer MM, Brockmeyer DL (2012) Complex Chiari malformations in children: an analysis of preoperative risk factors for occipitocervical fusion. J Neurosurg Pediatr. https://doi.org/10.3171/2012.3.PEDS11340
Strahle J, Smith BW, Martinez M, Bapuraj JR, Muraszko KM, Garton HJL, Maher CO (2015) The association between Chiari malformation type I, spinal syrinx, and scoliosis. J Neurosurg Pediatr 15:607–611. https://doi.org/10.3171/2014.11.PEDS14135
Moore HE, Moore KR (2014) Magnetic resonance imaging features of complex Chiari malformation variant of Chiari 1 malformation. Pediatr Radiol. https://doi.org/10.1007/s00247-014-3021-1
Aitken LA, Lindan CE, Sidney S, Gupta N, Barkovich AJ, Sorel M, Wu YW (2009) Chiari type I malformation in a pediatric population. Pediatr Neurol. https://doi.org/10.1016/j.pediatrneurol.2009.01.003
Greenberg JK, Yarbrough CK, Radmanesh A, Godzik J, Yu M, Jeffe DB, Smyth MD, Park TS, Piccirillo JF, Limbrick DD (2015) The Chiari severity index. Neurosurgery. https://doi.org/10.1227/NEU.0000000000000608
Schijman E, Steinbok P (2004) International survey on the management of Chiari I malformation and syringomyelia. Child Nerv Syst. https://doi.org/10.1007/s00381-003-0882-2
Papaker MG, Abdallah A, Cesme DH, Gönen G, Asiltürk M, Avyasov R, Sofuoğlu ÖE, Abdallah BG, Emel E (2020) Clinical and radiological evaluation of treated Chiari I adult patients: Retrospective study from two neurosurgical centers. Neurosurg Rev. https://doi.org/10.1007/s10143-020-01414-z
Holly LT, Batzdorf U (2002) Slitlike syrinx cavities: a persistent central canal. J Neurosurg Spine. https://doi.org/10.3171/spi.2002.97.2.0161
Takamura Y, Kawasaki T, Takahashi A, Nunomura K, Tiba K, Hasunuma M, Itou T (2001) A craniocervical injury—induced syringomyelia caused by central canal dilation secondary to acquired tonsillar herniation. J Neurosurg Spine. https://doi.org/10.3171/spi.2001.95.1.0122
Milhorat TH, Kotzen RM, Anzil AP (1994) Stenosis of central canal of spinal cord in man: Incidence and pathological findings in 232 autopsy cases. J Neurosurg. https://doi.org/10.3171/jns.1994.80.4.0716
Cai C, Oakes WJ (1997) Hindbrain herniation syndromes: the Chiari malformations (I and II)
Cesmebasi A, Loukas M, Hogan E, Kralovic S, Tubbs RS, Cohen-Gadol AA (2015) The Chiari malformations: a review with emphasis on anatomical traits. Clin Anat 28:184–194
Hunter JV, Youl BD, Moseley IF (1992) Neuro-radiology MRI demonstration of midbrain deformity in association with Chiari malformation
el Gammal T, Mark E, Brooks B (1988) MR imaging of Chiari II malformation. Am J Roentgenol 150:163–170. https://doi.org/10.2214/ajr.150.1.163
Olszewski AM, Proctor MR (2018) Headache, Chiari I malformation and foramen magnum decompression. Curr Opin Pediatr. https://doi.org/10.1097/MOP.0000000000000679
Saletti V, Esposito S, Frittoli M, Valentini LG, Chiapparini L, Bulgheroni S, Riva D (2011) Neurological pictures in paediatric Chiari I malformation. Neurol Sci. https://doi.org/10.1007/s10072-011-0744-8
Cahan LD, Bentson JR (1982) Considerations in the diagnosis and treatment of syringomyelia and the Chiari malformation. J Neurosurg. https://doi.org/10.3171/jns.1982.57.1.0024
Gamache FW Jr, Ducker TB (1990) Syringomyelia: a neurological and surgical spectrum. J Spinal Disord 1990 Dec;3(4):293-8. PMID: 2134442
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by CHEO REB#20/11X, file number 20200042.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dien Esquivel, M.F., Gupta, N., Wilson, N. et al. Pediatric Chiari I malformation: novel and traditional measurements associated with syrinx and surgery. Childs Nerv Syst 38, 2119–2128 (2022). https://doi.org/10.1007/s00381-022-05644-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05644-y