Abstract
Background
The cerebrospinal fluid neutrophil-to-lymphocyte ratio (CSF NLR) as a diagnostic biomarker of bacterial meningitis has been reported in adult trials. The aim of this study was to evaluate the CSF NLR as a diagnostic biomarker of bacterial meningitis in children and to define an optimal CSF NLR concentration.
Methods
We performed a retrospective cohort study of children with clinical findings compatible with meningitis. CSF NLR was calculated as the ratio of neutrophil count to lymphocyte count in cerebrospinal fluid (CSF). Initial data included clinical, radiological, and laboratory diagnostics.
Results
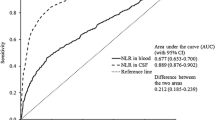
We determined CSF parameters from children with infectious meningitis (n = 348) and subdivided them into bacterial meningitis (n = 112) and viral meningitis (n = 236). CSF NLR was significantly higher in bacterial meningitis than in viral meningitis (P < 0.001), and its level was higher in Gram-negative bacterial infections than in Gram-positive bacterial infections (P = 0.01). In the receiver operating characteristic curve analysis, CSF NLR was better than CSF protein/sugar/WBC in the ability to distinguish bacterial meningitis from viral meningitis (AUC 0.91 ± 0.02 versus 0.88 ± 0.03/0.87 ± 0.03/0.86 ± 0.03), and using a cutoff point of 0.68, the sensitivity was 0.90, and the specificity was 0.75. Compared with Gram-positive infection, CSF NLR with Gram-negative infection was higher (media, IQR (1.18 (0.19–2.33) versus 3.90 (1.50–8.91), P = 0.01).
Conclusion
CSF NLR is a more useful diagnostic tool to distinguish between bacterial meningitis and viral meningitis in children. While at a cutoff value of 0.68, CSF NLR has better sensitivity and specificity for bacterial meningitis, and the higher level of CSF NLR could be related to Gram-negative bacterial infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infectious meningitis is a severe inflammatory central nervous system (CNS) disorder with high rates of morbidity and mortality in children. The most common pathogenic agents are viruses and bacteria [1]. Viral meningitis (VM)’ prognosis is good for most of them to offer appropriate supportive care. However, bacterial meningitis (BM) requires accurate diagnosis and prompt treatment due to high mortality rates and neurological impairments [2, 3]. Therefore, seeking a high sensitivity and specificity clinically biomarker that may differentiate BM from VM in children, is crucial to a favorable outcome.
Although detecting pathogens of CSF remains the gold standard for diagnosis, the results may not always be positive or available for early diagnosis [4]. Given most of the children with meningitis are distributed mainly in developing countries with poor medical infrastructure, rapid diagnosis is normally carried out via clinical symptoms and CSF conventional markers, such as leukocyte counts, protein, sugar, and Gram staining. Specifically, the increase in CSF white blood cell count has shown the predictive ability for BM, but the study found that its sensitivity was low in patients with comorbidities or atypical pathogens as causative agents [5]. Moreover, CSF protein and sugar would easily be regulated and controlled by the external environment so that it cannot be a simple maker to differentiate different central nervous system infections [6].
One Dutch study suggested that neutrophil-to-lymphocyte ratio (NLR) in peripheral blood may be a good biomarker that can differentiate between different types of infection [7] and can also predict the outcome of infection [8]. Similarly, in a study of acute meningitis, Mentis et al. found that the NLR tended to be higher in patients with bacterial infection than those with a viral infection, and the discrimination ability of NLR was significantly higher in CSF than in blood [9]. However, there are rare studies on CSF NLR of infectious meningitis in children, and more thorough studies need to be conducted. The aim of this study was to investigate whether the CSF NLR could be more useful to differentiate between children with meningitis due to bacterial infection and those with meningitis due to viral infectious causes and whether the causes of bacterial infections made any difference.
Patients and methods
Study design, setting, and participants
This retrospective observational study was conducted based on the cases at the Department of Pediatrics, Qilu Hospital, Shandong University. The time period ranges from June 1, 2014, to December 31, 2020. The data from clinical, radiological, and laboratory diagnostics were collected consecutively from children older than 1 month of age with the clinical diagnosis of infectious meningitis. This study has received approval from Shandong Qilu Hospital Ethics Committee (project number: KYLL-2017(KS)-621). All eligible children were taken blood samples and cerebrospinal fluid examination. In our institution, the diagnosis of infectious meningitis was based on the following article (Definition of Infectious Meningitis). BM patients were divided into three groups (group 1: cases in 1 month–4 years old; group 2: cases in 4–6 years old; group 3: cases in 6–16 years) according to the double scissors of leukocyte classification (first crossing time: 4–6 days; second crossing time: 4–6 years). We excluded children treated with antibiotics for more than 72 h at lumbar puncture or vein puncture, those with a history of medical therapy affecting leukocyte counting or leukocyte function, and those with connective tissue disorders (e.g., juvenile rheumatoid arthritis and systemic lupus erythematosus) or hematologic diseases complicated by encephalitis.
Definition of infectious meningitis
The diagnosis of infectious meningitis was based on the children’s histories, a positive CSF or blood culture, and the presence of some or all of the following clinical signs and symptoms, such as fever, nuchal rigidity, headache, convulsion, impaired consciousness sign, etc. The diagnoses of BM was referred to the guidelines of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID): with any of (1) positive CSF or blood culture; (2) positive Gram-staining; (3) CSF total leukocyte counts > 1000/mm3, as well as any of the following additions: (1) CSF neutrophil > 1/mm3, (2) CSF sugar < 50% of serum sugar, (3) CSF protein > 50 mg/dL [10]. The diagnostic of VM meets with at least one of the rules listed as follows: (1) the detection positive of viral ribonucleic acid (RNA) or deoxyribonucleic acid (DNA) with PCR in the CSF or serology; (2) CSF pleocytosis (< 1000/mm3) with any of the following: predominant lymphocytic pleocytosis, CSF sugar > 60% of blood sugar or CSF protein 50–250 mg/dL [11].
Study procedures
We collected demographics, such as age, sex, clinical symptoms and signs, and other general information. CSF was obtained on admission and/or within 24–72 h again, ranging from patients with suspected initial diagnosis meningitis to the collection of each specimen type. CSF was analyzed regarding leukocyte cell count, NLR, levels of protein, glucose, and lactate. All assays were done in strict accordance with the manufacturers’ instructions.
Statistical analysis
Descriptive data are presented as mean ± standard deviation (SD) or median with interquartile ranges (IQR). We use t-test or Mann–Whitney U tests for group comparisons of continuous variables, using chi-square test for categorical variables and using the Kruskal–Wallis test with Bonferroni correction for multiple comparisons. Receiver operator characteristic (ROC) curves and areas under the curve (AUC) were constructed to determine the optimal cutoff values as well as the sensitivity and specificity of blood and CSF parameters. The data was analyzed by SPSS 22.0, and it was regarded as statistically significant when the P-value was less than 0.05.
Results
Sociodemographic, clinical symptoms, neuroimaging, and routine laboratory parameters are summarized in Table 1. Among 348 children patient cases with clinical findings compatible with meningitis, 112 (32.2%) of which were diagnosed with BM and 236 (67.8%) of which were with VM. Children with BM that had a median age of 1.7 (0.1–5) years old, were younger compared with VM (with a median age of 5.3 years old, ranging from 0.4 to 10.1). The two groups were statistically significant (P = 0.001). The 112 BM samples were divided into three subgroups by age, namely 1 month to 4 years old group, 4 to 6 years old group, and 6 to 16 years old group. CSF NLR average was 4.4 ± 1.5, 3.2 ± 1.6, and 6.4 ± 1.2, respectively. There was no significant difference among the three groups. The age distribution of the BM group centralized from infancy, including 80 cases (71.4%) children under the age of 2 years old. Over 3 years old children mostly have susceptible factors: five cases have a history of craniocerebral trauma, three cases secondary to tympanitis, one case with cutaneous fistula, and one case with a cleft palate.
The main clinical manifestations in children with meningitis were fever (94.3%) followed by nuchal rigidity (67.8%), vomiting (56.9%), and Brudzinski’s (24.1%). No statistical difference for the above mentioned indications has been shown in the two groups (P > 0.05). And the occurrence of convulsion and consciousness disorder was especially higher in the BM group compared with the VM group (P < 0.05).
Neuroimaging was performed on 90.5% (315/348) patients, noting brain lesions on imaging studies in 70.2% (73/104) BM samples, shown as single or double lateral subdural effusion, hydrocephalus, the white matter loss and softening, or ventricle enlargement. VM samples exhibited brain lesions on imaging studies was only 5.2% (11/211), which was obviously lower than BM (P < 0.001).
The identified infectious pathogens were seen in 114 of 348 patients (Table 2). The etiology was confirmed by Gram-staining, bacterial culture, and/or polymerase chain reaction (PCR) in 39 (34.8%) patients with BM: Streptococcus pneumoniae (10), Escherichia coli (7), Meningitides Neisseria (5), and others (17). Among the 236 children with VM, 75 (31.8%) patients were identified positive through PCR. The most frequent causative microorganism was enterovirus (50), followed by herpes simplex 1 and 2 (8), and varicella zoster (5).
Figure 1 shows the diagnostic efficiency of blood and CSF parameters. Receiver operating curve analysis for NLR and protein in CSF were most notable. The area under the curve corresponded to CSF NLR 0.91 (95% confidence interval (CI) 0.87–0.95) versus CSF protein/sugar/WBC 0.88 (95% confidence interval (CI) 0.83–0.94)/0.87 (95% confidence interval (CI) 0.80–0.93)/0.86 (95% confidence interval (CI) 0.81–0.92). Using a cutoff point of 0.68 for CSF NLR, the sensitivity was 0.90, the specificity was 0.75.
CSF NLR levels between both groups (BM with and without identified infectious pathogens) were similar (1.50 (0.35–2.53) versus 1.11 (0.25–3.45), P = 0.44). There was a significant increase in CSF NLR in children with Gram-negative infection when compared to Gram-positive infection (media, IQR (1.18 (0.19–2.33) versus 3.90 (1.50–8.91), P = 0.01). There was no significant correlation between Gram-positive infection group and identified infectious pathogens group (P = 0.52) but with the Gram-negative infection group (P = 0.03) (Fig. 2).
Discussion
Bacterial meningitis is an important reason for morbidity and mortality in children. Each year, nearly 400,000 children lose their lives due to BM, and it is observed that in developing countries, death incidents relating to BM are much higher [12]. Fever (92.2%), nuchal rigidity (67.8%), headache (39.7%), convulsion (24.1%), and consciousness disorder (7.8%) are the typical clinical manifestations in this cohort, and one or more of these signs and symptoms are commonly absent. In this study, BM children are more prone to have convulsion and consciousness disorder, but other clinical symptoms have no significant difference. Therefore, it is very hard to distinguish between BM and VM if only judge by clinical manifestation. Second, obtaining neuroimaging in time can be challenging Due to time delay of transporting children suffering from cerebritis. For these reasons, there is usually a need for tests that are fast with a high level of specificity and sensitivity and that can be used in early diagnosis.
Regarding BM diagnosis, positive CSF culture or positive Gram staining, which is accepted as the golden standard, cannot be obtained for all patients, and besides, the results can be obtained only after 24–72 h [13]. In the present study, the global positive rate of the bacteria was 34.8%, and the most prevalent infectious pathogen detected was Streptococcus pneumonia. Infectious pathogens in our cohort are similar to those reported in several other studies regarding BM [14]. Even though there are new markers emerging from various studies, CSF conventional markers are still considered the acute phase reactant, which is mostly used [15]. Our study identified CSF conventional markers are simple, quick, and cheaper compared with other biomarkers and have a good performance for diagnosis BM. Studies in adults have indicated that adding CSF NLR to routine CSF examination is better in estimating the chance of BM in a very limited time [9].
NLR is a novel marker of inflammation, and it has been demonstrated regarding its ability to distinguish bacterial and viral infection. The mechanism of the increase in NLR of patients with meningitis is not clear, but it has been linked with the innate (i.e., neutrophils) and adaptive (i.e., lymphocytes) immune responses in the body [16]. The present study shows that CSF NLR values were much higher in BM. For children with low CSF NLR, VM was more likely to occur. In the comparison between BM and VM, the AUC of CSF NLR value was 0.91. At a cutoff value of 0.68, the sensitivity was 0.90, and the specificity was 0.75. These results indicate that the CSF NLR may be helpful in the differential diagnosis of children with infectious meningitis and also in deciding which children should be considered for antibiotic therapy. However, Mentis et al. found the CSF NLR value was significantly more discriminatory for patients aged over 14 years old than those aged 0–14. They concluded that care is required when applying diagnostic tests of CSF NLR for meningitis in different age groups because of patient heterogeneity [17]. In the present study, no significant differences were observed in CSF NLR in children of different ages. Since BM was commonly found in children under 2 years old, children of 4–6 years old and above 6 years old was a small part of the BM group and has little influence on the results. Furthermore, all cases were unhealthy children, and CSF NLR of diseases was not correlated with age.
Finally, our results indicate that patients with Gram-negative infection had significantly higher NLR compared to patients with Gram-positive infection. The main factor that distinguishes Gram-negative bacteria from Gram-positive bacteria is that the cell outer membrane contains endotoxin or lipopolysaccharide (LPS). The shedding LPS that interacts with Toll-like receptor 4 can activate the NF-κB pathway, causing an inflammatory reaction [18]. It is widely known that tumor necrosis factor alpha (TNF-α) and interleukin 6 (IL-6) functions as the downstream factor of the NF-κB pathway. A study by Turkmen et al. showed the NLR correlates with TNF-α and IL-6 concentrations [19]. However, the higher level of CSF NLR possibly being related to Gram-negative infection need to be confirmed by other future studies aiming to investigate in large numbers of children BM due to the small sample size of this experiment.
References
Beaman MH (2018) Community-acquired acute meningitis and encephalitis: a narrative review. Med J Aust 209(10):449–454
Ouchenir L, Renaud C, Khan S, Bitnun A, Boisvert AA, McDonald J, Bowes J, Brophy J, Barton M, Ting J, Roberts A, Hawkes M, Robinson JL (2017) The epidemiology, management, and outcomes of bacterial meningitis in infants. Pediatrics 140(1):e20170476
Hasbun R, Rosenthal N, Balada-Llasat JM, Chung J, Duff S, Bozzette S, Zimmer L, Ginocchio CC (2017) Epidemiology of meningitis and encephalitis in the United States, 2011–2014. Clin Infect Dis 65(3):359–363
Venkatesan A, Tunkel AR, Bloch KC et al (2013) Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis 57(8):1114–1128
Viallon A, Desseigne N, Marjollet O, Birynczyk A, Belin M, Guyomarch S, Borg J, Pozetto B, Bertrand JC, Zeni F (2011) Meningitis in adult patients with a negative direct cerebrospinal fluid examination: value of cytochemical markers for differential diagnosis. Crit Care. 15(3):R136
Precit MR, Yee R, Pandey U, Fahit M, Pool C, Naccache SN, Dien Bard J (2020) Cerebrospinal fluid findings are poor predictors of appropriate FilmArray meningitis/encephalitis panel utilization in pediatric patients. J Clin Microbiol. 58(3):e01592-e1619
Loonen AJM, de Jager CPC, Tosserams J, Kosters R, Hilbink M, Wever PC et al (2014) Biomarkers and molecular analysis to improve bloodstream infection diagnostics in an emergency care unit. PLoS ONE 9:e87315
Djordjevic D, Rondovic G, Surbatovic M, Stanojevic I, Udovicic I, Andjelic T, Zeba S, Milosavljevic S, Stankovic N, Abazovic D, Jevdjic J, Vojvodic D (2018) Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically ill and injured patients: which ratio to choose to predict outcome and nature of bacteremia?. Mediators Inflamm 2018:3758068
Mentis AF, Kyprianou MA, Xirogianni A, Kesanopoulos K, Tzanakaki G (2016) Neutrophil-to-lymphocyte ratio in the differential diagnosis of acute bacterial meningitis. Eur J Clin Microbiol Infect Dis 35(3):397–403
Van de Beek D, Cabellos C, Dzupova O et al (2016) ESCMID guideline: diagnosis and treatment of acute BM. Clin Microbiol Infect 22(Suppl 3):S37-62
McGill F, Griffiths MJ, Solomon T (2017) Viral meningitis: current issues in diagnosis and treatment. Curr Opin Infect Dis 30(2):248–256
Costerus JM, Brouwer MC, Bijlsma MW, van de Beek D (2017) Community-acquired bacterial meningitis. Curr Opin Infect Dis 30(1):135–141
McGill F, Heyderman RS, Panagiotou S, Tunkel AR, Solomon T (2016) Acute bacterial meningitis in adults. Lancet 388(10063):3036–3047
Dittrich T, Marsch S, Egli A, Rüegg S, De Marchis GM, Tschudin-Sutter S, Sutter R (2020) Predictors of infectious meningitis or encephalitis: the yield of cerebrospinal fluid in a cross-sectional study. BMC Infect Dis 20(1):304
van Ettekoven CN, van de Beek D, Brouwer MC (2017) Update on community-acquired bacterial meningitis: guidance and challenges. Clin Microbiol Infect 23(9):601–606
Xu JB, Xu C, Zhang RB, Wu M, Pan CK, Li XJ, Wang Q, Zeng FF, Zhu S (2020) Associations of procalcitonin, C-reaction protein and neutrophil-to-lymphocyte ratio with mortality in hospitalized COVID-19 patients in China. Sci Rep 10(1):15058
Mentis AA, Kyprianou MA, Tzanakaki G (2017) Age-specific application of neutrophil-to-lymphocyte ratio in meningitis: a nationwide study. Eur J Clin Microbiol Infect Dis 36(9):1553–1557
Zhou H, Ding G, Liu W, Wang L, Yongling Lu, Cao H, Zheng J (2004) Lipopolysaccharide could be internalized into human peripheral blood mononuclear cells and elicit TNF-alpha release, but not via the pathway of toll-like receptor 4 on the cell surface. Cell Mol Immunol 1(5):373–377
Turkmen K, Erdur FM, Ozcicek F, Ozcicek A, Akbas EM, Ozbicer A, Demirtas L, Turk S, Tonbul HZ (2013) Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patients. Hemodial Int 17(3):391–396
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the Ethics Committee of Shandong Qilu Hospital Ethics Committee (project number: KYLL-2017(KS)-621) and performed in compliance with the Helsinki declaration. Written informed consent was waived by the Ethics Committee of Shandong Qilu Hospital due to the retrospective nature and anonymous data collection.
Conflict of interest
Authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Cao, M., Zhu, X. et al. The cerebrospinal fluid neutrophil to lymphocyte ratio is a sensitive biomarker for bacterial meningitis in children. Childs Nerv Syst 38, 1165–1171 (2022). https://doi.org/10.1007/s00381-022-05501-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05501-y