Abstract
Neurocutaneous melanosis (NCM; MIM # 249400; ORPHA: 2481], first reported by the Bohemian pathologist Rokitansky in 1861, and now more precisely defined as neurocutaneous melanocytosis, is a rare, congenital syndrome characterised by the association of (1) congenital melanocytic nevi (CMN) of the skin with overlying hypertrichosis, presenting as (a) large (LCMN) or giant and/or multiple (MCMN) melanocytic lesions (or both; sometimes associated with smaller “satellite” nevi) or (b) as proliferative melanocytic nodules; and (2) melanocytosis (with infiltration) of the brain parenchyma and/or leptomeninges. CMN of the skin and leptomeningeal/nervous system infiltration are usually benign, more rarely may progress to melanoma or non-malignant melanosis of the brain. Approximately 12% of individuals with LCMN will develop NCM: wide extension and/or dorsal axial distribution of LCMN increases the risk of NCM. The CMN are recognised at birth and are distributed over the skin according to 6 or more patterns (6B patterns) in line with the archetypical patterns of distribution of mosaic skin disorders. Neurological manifestations can appear acutely in infancy, or more frequently later in childhood or adult life, and include signs/symptoms of intracranial hypertension, seizures/epilepsy, cranial nerve palsies, motor/sensory deficits, cognitive/behavioural abnormalities, sleep cycle anomalies, and eventually neurological deterioration. NMC patients may be symptomatic or asymptomatic, with or without evidence of the typical nervous system changes at MRI. Associated brain and spinal cord malformations include the Dandy-Walker malformation (DWM) complex, hemimegalencephaly, cortical dysplasia, arachnoid cysts, Chiari I and II malformations, syringomyelia, meningoceles, occult spinal dysraphism, and CNS lipoma/lipomatosis. There is no systemic involvement, or only rarely. Pathogenically, single postzygotic mutations in the NRAS (neuroblastoma RAS viral oncogene homologue; MIM # 164790; at 1p13.2) proto-oncogene explain the occurrence of single/multiple CMNs and melanocytic and non-melanocytic nervous system lesions in NCM: these disrupt the RAS/ERK/mTOR/PI3K/akt pathways. Diagnostic/surveillance work-ups require physical examination, ophthalmoscopy, brain/spinal cord magnetic resonance imaging (MRI) and angiography (MRA), positron emission tomography (PET), and video-EEG and IQ testing. Treatment strategies include laser therapy, chemical peeling, dermabrasion, and surgical removal/grafting for CMNs and shunt surgery and surgical removal/chemo/radiotherapy for CNS lesions. Biologically targeted therapies tailored (a) BRAF/MEK in NCM mice (MEK162) and GCMN (trametinib); (b) PI3K/mTOR (omipalisib/GSK2126458) in NMC cells; (c) RAS/MEK (vemurafenib and trametinib) in LCMNs cells; or created experimental NMC cells (YP-MEL).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurocutaneous melanosis (NCM; OMIM # 249400; ORPHA: 2481), now more precisely defined as neurocutaneous melanocytosis [49, 61], is a rare, sporadic, congenital syndrome characterised by the association of (1) congenital melanocytic nevi (CMN) with overlying hypertrichosis, occurring as (a) single large (or giant) nevi (LCMN), sometimes associated with smaller “satellite” nevi, or multiple nevi (MCMN), or a combination of both lesions, and (b) proliferative melanocytic nodules (PNs); and (2) melanocytosis (with infiltration) of the brain parenchyma and/or leptomeninges at magnetic resonance imaging (MRI) or histologically (Fig. 1) [14, 61, 63,65,65, 91, 94, 97, 142, 175, 185, 216].
Natural history of melanocytic lesions and neurocutaneous melanocytosis: traditionally progression from normal melanocyte to congenital melanocytic nevi (CMN) and/or to melanoma has been depicted in a linear fashion (linear progression); however, in individual lesions, certain stages may be skipped or never occur at all (non-linear progression pathways); linear progression through all stages (see A to D) in any individual lesion is probably fairly uncommon. (a) This pathway shows how skin melanocytes give rise (by acquiring NRAS gene mutations) to large congenital melanocytic nevi (CMN; left side pathway) or (by acquiring BRAFV600E gene mutations) to melanocytic nevi and later to basal nevi (right side pathway leading to pathway d); large CMN coupled to the events occurring in pathway b characterise neurocutaneous melanocytosis (NCM); large CMN that acquire NRAS, MAPK, PI3K, Akt, and/or mTOR gene mutations may give rise to skin melanoma transformation, which in turn can generate metastases and systemic melanoma. (b) This pathway shows how leptomeningeal melanocytes give rise (by acquiring NRAS gene mutations) to leptomeningeal melanocytosis and/or to brain parenchymal melanocytosis (i.e. neurocutaneous melanocytosis; NCM); leptomeningeal and/or brain melanocytosis may transform (by acquiring NRAS, MAPK, PI3K, Akt, and/or mTOR genes mutations) into nervous system melanoma, which in turn can generate metastases and organs’ melanoma. (c) This pathway shows how systemic melanocytes that acquire NRAS gene mutations give rise to organs melanocytosis, which in turn may progress (by acquiring NRAS, MAPK, PI3K, Akt, and/or mTOR genes mutations) to organs’ melanoma, and eventually can generate metastases and systemic melanoma. (d) This pathway is a pure skin progression pathway: melanocytic nevi and/or basal nevi that acquire NRAS and BRAFV600E gene mutations, may more commonly form de novo dysplastic nevi; approximately 2/3 of skin melanomas arise without a known benign precursor lesion, possibly as a result of late acquisition of a MAPK pathway mutation in already sensitised melanocyte(s) with other oncogenic changes (e.g. RAS, BRAF, NF1, PTEN and/or CDKN2A inactivation); the vast majority of nevi will never progress to melanoma, many will remain clinically stable over a lifetime, whereas others will regress (dead end pathways); some basal nevi may later give rise to dysplastic nevi, but this is probably fairly uncommon; it is not clear that dysplastic nevi progress to melanoma more commonly than banal nevi.
CMN is a particular melanocytic in utero proliferation characterised, per se, by an increased risk of melanoma transformation during infancy or adulthood [43, 94, 105, 163]. Individuals in the general population may have CMN as an isolated finding i.e. the so-called CMN syndrome (CMNS; or giant pigmented hairy nevus syndrome, GPHN; or giant congenital pigmented nevus, GCPN; or pigmented moles, PM; MIM # 137550; ORPHA: 626] [117, 128, 165, 183, 200].
On the other hand, individuals in the general population may also have meningeal melanocytosis, as a solitary manifestation: this is a rare, challenging, benign, diffuse pigmented tumour of the meningeal melanocytes that can form solitary extra-axial tumours, which invade the parenchyma presenting signs of malignancy [10, 142, 149].
The terms “melanosis” or “melanocytosis”, in NMC refer to an excess of melanocytes (Figs. 1 and 2) (in the skin, leptomeninges, and brain), which occurs as a diffuse or nodular proliferation, usually benign, but sometimes degenerating into its malignant counterpart [43, 61, 94, 97, 118, 163]. Thus, individuals with NCM are at higher risk for developing melanoma of the skin and/or central nervous system (CNS), or to develop non-malignant melanosis of the brain [14, 21, 94] (Fig. 1), which in turn can increase mortality because of its effects on increasing intracranial pressure [2, 36, 52, 94].
The multistep (I to IV) phases of synthesis, formation, growth, and maturation of melanosomes and melanin production (melanogenesis) in skin melanocytes. Melanosomes are organelles found in animal cells (e.g. skin and eye choroidal melanocytes; retinal pigment epithelial cells) and are the site for synthesis, storage and transport of melanin, the most common light-absorbing pigment (responsible for colour and photoprotection in animal cells and tissues) found in the animal kingdom. The melanogenesis takes place in melanosomes. As first, stimulation of membrane-bound melanocortin 1 receptor (MC1R) by alpha-melanocyte-stimulating hormone (αMSH) leads to activation of the MITF gene coding for the MITF protein, which in turn, via the tyrosinase enzyme TYRP1, starts (through the endoplasmic reticulum and the Golgi system) the development of the earliest precursor of the future melanosome, i.e. a vesicle (Stage I), which builds inside a fibrillar matrix formed by glycoproteins (e.g. PMEL17 and MART1) and gets tyrosinase and other enzymes of melanogenesis (Stage II). The melanosome produces melanin, which polymerises and settles on the internal fibrils (Stage III). In the last Stage IV melanosome fulfilled with melanin anchors (and moves, when necessary), through dynein, kinesin, microtubules, melanophilin, and myosin. Each type of melanin is synthesised in a separated melanosome. Then, mature stage IV melanosomes enter (via membrane fusion between melanocytes and keratinocytes; or vesicular tnasfer; or cytophagocytosis) into keratinocytes. Each of these steps is genetically pre-ordinated and modulated and can change secondarily to BRAF and/or NRAS mutations, or MAPK, PI3K, Akt, or mTOR signalling pathways influences. Abbreviations: αMSH, alpha-melanocyte-stimulating hormone; AP1, activator protein transcription factor 1; AP3, activator protein transcription factor 3; BLOC1, biogenesis of endosome/lysosome-related organelles subunit 1; BLOC2, biogenesis of endosome/lysosome-related organelles subunit 1; clathrin, clathrin protein forming coated vesicles; dynein, cytoskeletal motor protein moving along microtubules (MT); kinesin, kinesin motor protein moving along microtubules (MT); MART1, melanoma antigens recognised by T cells; MCR1, melanocortin receptor 1; melanophilin, carrier protein member of the exophilin family of the Rab effector subfamily; MITF, melanocyte inducing transcription factor; myosin, myosin motor protein; PMEL17, pre-melanosome protein 17; Rab27a, Rab subfamily of GTPase small membrane-anchorated protein; Rab7, Rab subfamily of GTPase small membrane-anchorated protein 7; Rab27a, Rab subfamily of GTPase small membrane-anchorated protein 27a; Rab32, Rab subfamily of GTPase small membrane-anchorated protein 32; Rab38, Rab subfamily of GTPase small membrane-anchorated protein 38; TYRP1, tyrosinase-related protein 1 [adapted and modified from ref. 17]
The typical cutaneous lesions are recognised at birth (“congenital”) [128]; neurological manifestations can appear, as acute manifestations of increased intracranial pressure in infancy, or more typically later in childhood or adult life [61, 91, 158, 164]. NMC patients may be symptomatic or asymptomatic [1], with or without evidence of the typical CNS changes at MRI [2, 14, 36, 52, 62, 94, 216]. Associated brain malformations are often recorded [94]. There is no systemic involvement in NCM, or only rarely [57, 61, 109, 150, 187]. Although patients with asymptomatic NCM may live without significant problems for extended periods, the onset of symptoms in NCM generally indicates the beginning of an aggressive clinical course, with a poor prognosis and frequently death occurring within 2–3 years of diagnosis [61, 91, 225]. In older series [45], severe/lethal disease was recorded in up of 92% of affected individuals, but more recent NCM surveys record lack of progression of abnormal imaging and/or lack of development of symptoms, for decades, after abnormal imaging [61, 91].
Postzygotic mosaic mutations in the NRAS (neuroblastoma RAS viral oncogene homologue; OMIM # 164790; located on chromosome 1p13.2) proto-oncogene, disrupt the RAS cell-signalling pathways (specifically, the RAS/MEK/ERK pathway and phosphatidylinositol 3-kinase-mediated/PI3K-Akt pathway) and drive melanocytic benign proliferations in utero, being responsible for single and/or multiple (small, medium-sized, and large/giant) CMNs, as well as for melanocytic and non-melanocytic central nervous system (CNS) lesions in NCM (Figs. 1 and 2) [19, 39, 48, 50, 51, 69, 75, 104, 130, 162, 186, 187, 197, 203, 228].
From a pathogenic viewpoint, it seems that either amplification of mutated NRAS [187, 205, 206] or the loss of NRAS [186], in certain cellular contexts (e.g. melanocytes within CMNs/NCM), represent new genetic mechanisms leading to melanoma and/or promoting malignant tumour progression; alternative mechanisms could be related to genetic abnormalities such as point mutations/variants or gene fusion in other genes (e.g. mutations/variants in BRAF, KRAS, APC, and MET genes; or gene fusion in ZEB2-ALK and SOX5-RAF1 genes) leading in turn to mlanocytic proliferations either in satellite nevi or within LCMN and/or to melanoma progression [129] (Figs. 1 and 2).
Standard treatment strategies include laser therapy, chemical-peeling, and dermabrasion, later completed by surgical removal/skin grafting for CMNs, neurosurgical shunt placement, and removal/chemotherapy for CNS lesions [61, 91].
Biologically targeted experimental therapies so far successfully tailored: (a) MEK pathway (e.g. the acute MEK inhibitor MEK162) in a murine model [157]; (b) the dual PI3K/mTOR pathway (e.g. omipalisib/GSK2126458) in clonigenic oncogenically transformed NCM-derived cells; and (c) the RAS-ERK pathway (e.g. vemurafenib and trametinib) in LCMNs cells [79, 136, 226]; or generated platforms with NCM cells (YP-MEL) for pre-clinical studies [170].
Historical background and terminology
The French physician and musician (inventor of the stethoscope at the Hopital Necker in Paris, in 1816), René Théophile Hyacinthe Laennec (1781–1826) (Fig. 3), was the first to apply the term “mélanose” (derived from the Greek word μελα, μελαν = black) to the presence of hyperpigmented tissues [113]. He described melanosis as masses, infiltration in the tissue of organs, or deposition on the surface of organs. His descriptions were extremely accurate and are still valid. Laennec in 1812 [114] also provided the first description of melanoma as a disease entity [61].
Pigmentation, due to the presence of melanocytes (which are normally recorded cells in the leptomeninges), in the brain, was observed, by neuropathologists, to the naked eye, since the XIX and early XX centuries [138, 145, 210] and later recorded at neuroimaging [68, 167].
The first clinical descriptions of NMC is attributed to the Bohemian physician, pathologist, historian, philosopher and liberal politician, baron Carl J. von Rokitansky (1804–1878) (Fig. 4), who, in 1861 [169], reported in Vienna on a 14-year-old girl with macrocephaly, mental retardation, and multiple large hairy pigmented skin nevi, who at post-mortem examination was found to have hydrocephalus, hydromyelia, with “… macroscopic and microscopic ….” thickening and diffuse infiltration of the skin, of the leptomeninges and the subependymal layer of the ventricles with “…benign, round melanin-containing granules in spindle and branched cells…” and “…. large/diffuse brownish-black melanocytic deposits ….”; in addition to that, there were “… small nodules of pigment the size of millet seeds scattered over the pia mater and ependyma ….”; he also noted that there was “….perivascular pigmentation…” with no parenchymal involvement of the brain or of any other organ [61, 153, 169].
The Bohemian physician, pathologist, historian, philosopher, and liberal politician, baron Carl J. von Rokitansky (1804–1878), who, in 1861, reported for the first time in Vienna, on a 14-year-old girl with neurocutaneous melanocytosis: the girl had clinically macrocephaly, cognitive disabilities, and multiple large hairy pigmented skin nevi, and, at post-mortem examination, hydrocephalus, hydromyelia, and thickening and diffuse infiltration of the skin, of the leptomeninges and the subependymal layer of the ventricles with brownish-black melanocytic deposits with no parenchymal involvement of the brain or of any other organ
Early in 1897, Bircher in Zurich used the term “naevus pilosus pigmentosus congenitus, extensus” to define giant congenital nevi, stressing also their peculiar shape. He reported on a patient with a “neck stole” nevus and made an extensive review of the literature in 34 patients with giant nevi, identified their location, and used designations such as a “bathing trunk” (“schwimmhosenart”), and other terms to describe their distribution [24].
The German physician and pathologist Siegfried Oberndorfer (1876–1944) made the second report on NMC [143, 144] in an 8-month-old infant in Munich, who also presented with marked macrocephaly and multiple deeply pigmented nevi: the skin nevi were so numerous that he called this pattern “panther type”; post-mortem examination revealed hydrocephalus and highly intensive pigmentation (more intense as compared to the report of Rokitansky in 1861 [169] of the brain, including the cerebrum, optic thalamus, the floor of the IV ventricle, and the cerebellum (these features were confirmed by later studies); numerous large and round cells contained much granular pigment. He was the first to state that both the skin and central nervous system pigmentation were a primary condition, originating during embryogenesis, not secondary to metastatic colonisation from the skin.
Grahl in 1906 [72] and MacLachlan in 1914 [122] contributed with further detailed reports in a newborn (with extensive CMN of the lower part of the abdomen and thighs) and a 2-month-old girl (with four CMN of the anterior and posterior chest), respectively.
Wilcox in 1939 [221] reported an infant with hydrocephalus and an extensive CMN of the skin and brain and proposed that this condition, which he named “melanomatosis of the skin and central nervous system”, should be included amongst the dawning group of the so-called congenital neurocutaneous syndromes, a heterogeneous group of conditions first introduced in the medical literature, few years before, by Yakovlev and Guthrie in 1931 [175, 181, 223]. Touraine in 1941 proposed the term “melanoblastose neuro-cutanee” to emphasise its congenital character [210].
The Belgian neurologist and pathologist, Ludo Van Bogaert (1860–1989) first introduced, in the 1940s [212] the term “neurocutaneous melanosis”, which he initially thought was a familial condition.
In 1949 [211] Touraine published an extensive review of the NCM literature that led several authors to call NMC “Touraine syndrome” [55, 122, 152, 202, 219].
Fox and colleagues, in 1964 [64], adopted the term neurocutaneous melanosis, reported three additional cases, and made a comprehensive review of the literature. Bolande in 1974 [26] included NCM in the group of “neurocristopathies” [27, 61].
In 1972 Fox first proposed three criteria for the diagnosis of NCM [63]: (1) large or numerous pigmented nevi in association with leptomeningeal melanosis or melanoma; (2) no evidence of malignant change in any cutaneous lesion; and (3) no evidence of melanoma in any location other than the meninges [63].
In 1991, Kadonaga and Frieden [97] further defined the terminology with regard to the size of the lesions and specifically distinguished neurocutaneous melanosis from a possible, simultaneous occurrence of primary and metastatic melanoma; they introduced new criteria for diagnosis [61]:
-
1.
Large or multiple congenital nevi in association with meningeal melanosis or melanoma: large refers to a lesion > 20 cm (in adults); or 9 cm in the head or 6 cm in the body (in neonates and children); multiple signifies > 3 lesions;
-
2.
No evidence of cutaneous melanoma, except in patients in whom the examined areas of the meningeal lesions are histologically benign;
-
3.
No evidence of meningeal melanoma, except in patients in whom the cutaneous lesions are histologically benign.
The problem with their review of the criteria [97] is that they did not mention giant congenital nevi and therefore they did not define or distinguish giant from large nevi, despite the fact that 66% were “giant pigmented nevi” in their review [61]. Since then, many authors use the terms large and giant interchangeably. Ruiz-Maldonado in 2004 [183] proposed a classification that defines more precise measurements to distinguish large and giant nevi: he proposed that large nevi are 11–20 cm and giant nevi are from 21 cm to more than 40 cm [61]. On the other hand, the term “giant” nevus is well defined and it has been widely used for many years by multiple authors after Reed and colleagues used this term in 1965 [166].
Kadonaga and Frieden [97] considered those cases with histological confirmation of the CNS lesions as definite; all others were labeled provisional. A rare form of spinal leptomeningeal melancytosis without cutaneous nevi has been described in a few young adults. Fox and colleagues [63] designated those cases as “formes frustes”. This pattern is less frequent in children [31]. Kadonaga and Frieden [97] excluded cases without cutaneous lesions.
Incidence and prevalence
Neurocutaneous melanocytosis is a rare syndrome: approximately 300 cases have been reported worldwide [5].
Approximately 1% of neonates are born with small CMN [41, 58, 119, 124, 125, 215]. LCMN (rather than MCMN), are estimated to occur in less than 1 in 20,000 individuals in the general population [97, 105, 200]: amongst these individuals, only up to 12% will have NMC; thus, the overall incidence for NMC is quite rare [61, 91]. In a worldwide registry of patients with LCMN, 26 out of 379 (i.e. 6.68%) had NCM: 17 out of these 26 (i.e. 65%) were neurologically symptomatic [3]. As neuroimaging is performed in more individuals who are at high risk based on the extent and/or distribution of the skin findings but asymptomatic, this percentage may be higher (closer to 25%) [94, 216].
There is no gender difference. It, apparently, occurs more often in the white (Caucasian) race, whilst sporadically in blacks [41].
Clinical manifestations
Neurocutaneous melanocytosis is characterised by (Fig. 1):
-
1.
Three types of cutaneous lesions: (a) benign CMN; (b) proliferative melanocytic nodules; and eventually (c) malignant transformation into melanoma of previous lesions;
-
2.
Neurological manifestations secondary to melanocytic proliferation, benign or malignant, of the CNS, including either the leptomeninges or brain parenchyma.
The typical cutaneous lesions are recognised at birth; neurological manifestations usually appear later [158, 164]. There is no systemic involvement in NCM, or only rarely [57, 109, 150, 187, 213].
Cutaneous findings
-
(a)
Benign congenital melanocytic nevi
These lesions are present, and usually recognised, at birth, as single or multiple melanocytic nevi with abundant hair [204]. Approximately 80% of individuals with large or giant nevi present with associated smaller “satellite” nevi [45, 46, 61, 117, 128, 165, 183, 200]: the mean number of satellite nevi can range from 0 to 2,500, with a mean number of 80 and a median number of 20.
The colour of the skin complexion and hair is similar: it may be very dark (80%) and/or light brown (16%) or mottled (4%), darker in blacks [119, 153, 165, 200]. In some neonates this hyperpigmentation can fade over months resembling later to dark port wine stains: thus, a history of strong pigmentation at birth and concomitant hypertrichosis are of diagnostic importance [61, 91].
According to the proposed criteria by Ruiz-Maldonado [183], the size of CMN is defined as small (sCMV) < 1.5 cm, medium (mCMN) 1.5 to 10 cm, large (lCMN) from 11 to 20, and giant (gCMN or GCMN) from 21 cm to more than 40 cm maximum diameter [58]. With respect to age, the size is usually equal to or greater than 20 cm in adults; 9 cm on the scalp or 6 cm in the body, in infants [61, 91, 96, 134]. Variations in clonogenicity and tumourigenic properties in NRAS-mutated CMNs parallel and increase with their size [75].
Most reports do not include the measurement of large or giant nevi (lCMN or GCMN), as these usually cover extensive areas of the body, thus more often is described the body surface [71]. In the most severe cases, the nevus can cover 80% of the body surface [108]: these patients are at higher risk for developing leptomeningeal and cutaneous melanoma [63]. Patients with numerous satellite nevi involving the head, posterior neck, or the paravertebral areas are at the greatest risk of developing NCM [61, 91, 120].
The CMN is usually distributed over the body in typical patterns: according to Martin da Silva et al [128] 6 repeatable patterns of distribution of lCMN or GCMN can be recognised (the “6B patterns”), including (1) “bolero” or “shoulder stole” (mainly involving the upper aspect of the back, including the neck and shoulders, usually sparing the upper limbs) (Fig. 5); (2) “back” (on the back, often round-shaped, without involvement of the buttocks or shoulders) (Fig. 6a-c); (3) “bathing-trunk” (mostly involving the genital region and buttocks) (Fig. 7); (4) “breast/belly” or (isolated to the chest and/or abdomen without involvement of bolero or bathing trunk distributions) (Fig. 8); (5) “body extremity” (isolated to lower extremities and sometimes also to part of the buttocks) (Fig. 9a–c); and (6) “body” or also “life-vest jacket” (both bolero and bathing trunk involvement) (Fig. 10a, b). All these 6B patterns of CMN distribution, except the “body extremity” pattern, reflect the archetypical pattern of distribution of mosaic skin lesions classified as “type 4 patchy pattern without midline separation,” which consists of large skin patches not respecting the dorsal and ventral midline (Fig. 11a) [80, 81, 84, 172,179,180,181,182,183,184,185,180, 182]. There are six known archetypical patterns of distribution of skin mosaicism according to the classification proposed by Happle [80,81,82,83,84,85, 209 ]. Additional sub-patterns for GCMN can be recorded, including (a) the “cape-like” distribution (over the occipital area and/or the upper back, a variant of the bolero pattern) (Fig. 12a, b); (b) the “biker-glove” distribution, with sparing of the distal digits (Fig. 13a-c) [107, 156]; (c) the “coat sleeve” or “stocking-like” in the face (Fig. 14); and (d) the “unilateral” pattern of distribution, which stops at the midline (Fig. 15: also known as (“type 5 lateralised archetypical pattern”) [80,82,83,84,84, 182, 209]. Isolated involvement of the extremities (Figures 9a, b and 13a-c) is the least frequent [128]; in extensive nevi involving the extremities, atrophy (secondary to fat and/or bone reduced growth) of the affected limb can occur (Fig. 9b, c) [20, 37, 76, 92, 128, 156, 185, 222].
Pattern 2 (“6B patterns”): a ideogram showing the “back” patterning, which is localised on the back, often round-shaped, without involvement of the buttocks or shoulders); b a child with neurocutaneous melanocytosis and a giant/large congenital hairy melanocytic nevus over the posterior region of his trunk: note the great amount of satellite melanocytic nevi over the upper part of the trunk and limbs; c a child with neurocutaneous melanocytosis and a giant/large congenital melanocytic nevus over his trunk: note that the nevus is partially sparing the buttocks, but has large and smaller satellite melanocytic nevi over the shoulders and limbs, configuring a mixed pattern (courtesies of prof. Sergiusz Jozwiak, University of Warsaw, Poland; © Springer Publishers) [96]
a Pattern 3 (“6B patterns”): ideogram showing the “bathing-trunk” patterning, which is mostly involving the genital region and buttocks. b a 30-month-old with a typical distribution of CMN over the buttocks and genital region. This girl had also a cape-like CMN (see Fig. 14)
Pattern 5 (“6B patterns”): a ideogram showing the “body extremity” patterning, which is confined to the lower extremities and sometimes also to part of the buttocks; b a child who later developed neurological manifestations of neurocutaneous melanocytosis, showing a giant/large congenital hairy melanocytic nevus localised to the left leg; c anterior X-rays of the limbs showing reduced growth of the bones and fat tissue in the left leg (labelled as “S”, sinistra, in Italian = left) (courtesy of Dr. Piero Pavone, University of Catania, Italy)
Pattern 6 (“6B patterns”): ideograms showing the a “body” or b “life-vest jacket” patterning, which is characterised by the co-occurrence of both bolero (pattern 1) and bathing trunk (pattern 3) involvement; c an infant with neurocutaneous melanocytosis and a typical “life-vest jacket” congenital melanocytic nevus
Ideogram showing one of the six archetypical patterns of distribution of mosaic skin lesions proposed by Happle [80, 81, 84] and classified as “type 4 patchy pattern without midline separation”, which consists of large skin patches not respecting the dorsal and ventral midline: this pattern reflects the distribution of all the 6B patterns of distribution of congenital melanocytic nevi in the general population and, more specifically, in neurocutaneous melanocytosis.
a, b ideograms showing the additional sub-pattern (“6B patterns”) of distribution of congenital melanocytic nevi, classified as “biker-glove” distribution, with sparing of the distal digits (this pattern is a sub-type of pattern 5 “body-extremity”); c a child with neurocutaneous melanocytosis and a large/giant congenital melanocytic nevus of the lower limb, which spares the distal digits of the foot
a Ideograms showing the additional sub-pattern (“6B patterns”) of distribution of congenital melanocytic nevi, classified as “coat sleeve” or “stocking-like” in the face; b a 30-month-old girl with neurocutaneous melanocytosis and multiple medium-sized congenital melanocytic nevi over the occipital area of the scalp; and the buttocks (see Fig. 7b), thus configuring a mixed pattern of distribution of congenital melanocytic nevi
Ideograms showing the additional sub-pattern (“6B patterns”) of distribution of congenital melanocytic nevi, classified as “unilateral” pattern of distribution, which stops at the midline (this pattern reflects one of the six archetypical patterns of distribution of mosaic skin lesions proposed by Happle [80, 81, 84] and classified as “type 5 lateralised archetypical pattern”
Usually, the presence, number, and distribution of the satellite nevi modify and complicate the borders and framework of the 6B pattern of distribution of CMNs (Figs. 6b-c, 7b, 12b) [126, 128].
CMVs have been also reported in the mucous membranes [29, 184].
CMN usually originate from the posterior midline [84, 128, 191, 203]. The nevus on the back sometimes has a midline vertex over the thoracic or cervical spine [44, 97, 106, 129, 166].
Intractable pruritus (likely secondary to serotonin-mediated mechanisms) [186], an uncommon complication arising in LCMN, may be debilitating [60, 66, 136, 186] and can benefit of non-conventional treatment with ondansetron [66] or trametinib [136].
-
(b)
Benign proliferative nodules
Proliferative nodules arise as secondary proliferation within giant CMN, particularly in the “bathing trunk” or in the “life-vest” nevi, which are mostly located in the back and hip regions [128, 129, 203, 215]. As true melanoma can occur in the neonate [112, 205], the development of any secondary proliferation in a CMN is of great concern [17, 19, 22, 161, 195, 214, 215]. Proliferative nodules are usually reported as single or multiple lesions [2, 24, 40, 71, 184, 215] and may be also present at birth [61, 91, 215] or, more often, can appear later. Smaller papular lesions, associated with proliferative nodules and giant CMN have also been described [24, 166, 223, 224].
The histology of these nodules is that of delayed melanocytic maturation, indicative of benign nature [215]; with time they may also regress [17]. The main processes involved in their clinical evolution are maturational, proliferative, and apoptotic [17, 195]. Expression of 5-hydroxymethylcytosine (5-hmC) levels can help in distinguishing PNs from true melanoma transformation [155].
-
(c)
Malignant transformation of melanocytic nevi and proliferative nodules
The development of malignant melanoma arising in small (sCMN) and medium (mCMN) CMN is rare (Fig. 1) [17, 25, 45, 46, 61, 91, 133, 205, 215, 224]. The incidence of malignant melanomas arising in LCMN/GCMN has been reported as high as 12% [46] and more frequent (95%) in the axial localization usually within the intradermal part of the nevus [46, 166]. The calculated 5-year risk of developing melanoma in LCMN is 2.3%, whilst the risk of developing NCM is 2.5% [25]. The risk of malignant transformation is proportionate to the extent (>> in larger nevi) and distribution (>> in lesions of the head and upper trunk) of the CMN; the risk is highest in the first 5 to 10 years of life and carries a significant mortality [17, 46, 76, 215]. An additional risk factor is the presence of large numbers of satellite nevi [20, 45, 46, 120] and axial location [46].
Neoplasms of other tissues derived from neural crest (e.g. schwannomas) can occur within CMN [61].
Benign placental infiltration by melanocytes has been rarely recorded in neonates with CMN [13]. The placenta should be always examined in these cases and should not be confused with congenital melanoma [61]. Placental metastases from cutaneous malignant melanoma in both mother and foetus are less rare than benign melanocytic infiltration [13].
Neurological findings
In general, neurological manifestations present as acute or subacute signs/symptoms with a ominous onset (Figs. 16 and 17) [61, 91]. Once neurological manifestations appear, the prognosis is poor because there is usually a relentlessly progressive course with high mortality in infancy and early childhood [35, 119, 154]. The prognosis is usually less ominous with involvement of the brain parenchyma rather than leptomeninges [6, 145, 225].
This 30-month-old girl with neurocutaneous melanocytosis had a congenital melanocytic nevus over the scalp (shown in Fig. 14b) and buttocks (shown in Fig. 7b): she underwent brain MRI examination at age 2 years when she was still neurologically asymptomatic; MRI studies revealed hydrocephalus (a) associated to the Dandy-Walker malformation (b); upon admission at age 30 months, her clinical conditions were severely deteriorated including seizures and clinical manifestations of increased intracranial pressure; a new MRI study (c, d) revealed two large subdural hemispheric fluid collections, signal intensity changes in the leptomeninges and in the subarachnoid spaces secondary to proliferation and infiltration by melanocytes; the evacuation of both fluid collections and the insertion of a V-P shunt, though assuring an immediate improvement, could not avoid her death after a few months.
Intra-operative images of the 30-month-old girl shown in Figs. 7b, 14b and 16: note the diastasis of the coronal suture and the fluid escaping under high pressure after dura mater puncturing, which is related to intracranial hypertension (yellow arrows); the abnormal colour of the dura mater and the arachnoid membrane is due to the melanocytic infiltration (c); melanocytic cells accumulated also in the subarachnoid spaces
Age at onset
Neurological signs/symptoms typically present in the first or second year of life or so (Fig. 16). Neonates and infants usually present with acute onset.
Leptomeningeal and parenchymal melanocytosis has been recorded in neonates at MRI: it may remain asymptomatic for several months or years [61, 91, 193]. A second but uncommon peak of onset occurs in the 2nd and 3rd decades [97]. In patients with later onset of manifestations the usual findings are discrete intracranial masses, with slow to moderate growth rates: these patients usually present focal epileptic activity at video-EEG and/or focal seizures, localised sensorimotor deficits and difficulties in speech [44, 124, 125, 158].
Increased intracranial pressure
The most common (two-thirds of NCM patients) manifestation, includes signs/symptoms of intracranial hypertension [64, 76, 97, 189, 190], secondary to obstructive hydrocephalus (Figs. 16 and 17).
In about 10% of these patients there is a special association with Dandy-Walker malformation complex (DWM complex; see below) (Fig. 16). The onset of intracranial hypertension in infants is overt, with rapidly increasing head circumference, irritability, headache, re-current vomiting, and “setting sun sign” [73, 171]. These patients are brought to hospital seriously ill and urgently require a ventriculoperitoneal shunt. The course is characterised by rapid improvement after surgery but, unfortunately, there often is a relapse days or weeks later, death usually occurring shortly thereafter [64, 76, 110, 119, 140].
Tumours in the brain parenchyma are the second most frequent cause of intracranial hypertension. The communicating type of hydrocephalus, in two-thirds of patients, is attributed to accumulation of melanotic cells in the basal subarachnoid cisterns, with subsequent obstruction of cerebrospinal flow (CSF) flow and prevention of CSF reabsorption in the arachnoid villi (Fig. 17); in the remaining third, hydrocephalus is non-communicating due to aqueductal stenosis or outlet 4th ventricular obstruction [90]. Infants often have normal development initially [76, 132], later showing regression in ambulation and language [45, 132]. With disease progression, some patients develop an ataxic gait and, later in the course, lose the ability to sit upright [45, 76, 97]. In some children delayed development precedes the onset of acute neurological manifestations.
Seizures/epilepsy
This is one of the most common manifestations in NCM at all ages [158]. Seizures are present in patients with parenchymal involvement and practically in all patients who present with DWM complex (Figs. 16 and 17). In some reports semiology is not provided, but usually seizures are generalised, tonic-clonic [38], myoclonic [140], or partial motor and focal dyscognitive seizures [41, 45, 64, 188]. Focal dyscognitive seizures are common with involvement of the temporal lobes, particularly the amygdala [158], which can be successfully treated by anterior temporal lobectomy [33, 47, 67]. Focal epilepsy as the only manifestation is rare [6, 225]. Status epilepticus followed by intractable complex partial seizures with rapidly deteriorating course is described in young children [40]. Infantile spasms syndrome, West syndrome, and Lennox-Gastaut syndrome have been also reported [45, 131, 220]. Infrequently, epilepsy begins in young adulthood [225]. Pellino and colleagues [158], emphasised that children with parenchymal melanosis can experience epilepsy and developmental delay; the distribution of parenchymal melanocytosis (specifically, in the amygdala), was the best predictor of epilepsy prognosis and epilepsy surgery was the best choice in isolated amygdala localization.
Spinal involvement
Involvement of the spinal cord is recorded in approximately 20% of patients, who develop symptoms of myelopathy, radiculopathy, or bowel or bladder dysfunction [63, 98, 154]. Clinically, patients may rapidly deteriorate with progressive motor deficits, hemiparesis or quadriparesis, and aphasia in the terminal period [71, 159, 188, 218, 227]. Diffuse leptomeningeal thickening, arachnoiditis and secondary syringomyelia [47, 157], and spinal cord compression can occur [97]. There have been reports of children with melanocytosis in temporal lobes, hydrocephalus, meningeal spinal enhancement, and an extensive subarachnoid CSF accumulation with cord compression and syringomyelia [116, 160]. Extramedullary melanoma infiltrating the entire subarachnoid space and spine has been also reported [198]. The absence of spinal symptoms with extensive infiltration of the spinal cord is rare, and usually, it may appear terminally [28, 202]. Infrequently, NCM is associated with spina bifida occulta [7, 24, 87, 194, ].
Dysphagia
Incoordination of the Oropharyngeal muscles or frank dysphagia can be a terminal sign [59] and has been reported in a number of patients with lower brainstem infiltration [131].
Other abnormalities
A sleep cycle disorder can also be recorded. In about 10% of patients NCM is diagnosed because of developmental delay [30, 61, 91, 120].
Late onsets
Manifestations appearing later in life are usually chronic and may be associated with neuropsychiatric manifestations, including depression or psychosis [11]. The oldest and only patient, who became symptomatic at 65 years of age and died shortly after, was a female with a hairy CMN [103]: malignant melanoma in the temporal lobe was confirmed at post-mortem.
Natural History
NMC patients may be symptomatic or asymptomatic, with or without evidence of the typical CNS changes at MRI [1, 14, 15, 16, 22, 94, 216]. More recent NCM surveys record lack of progression of abnormal imaging and/or lack of development of symptoms, for decades, after abnormal imaging [61, 91]. Neurological manifestations of NCM are caused by leptomeningeal melanocytosis, intracranial melanoma, and intracerebral or subarachnoid haemorrhage. Leptomeningeal melanosis tends to occur in the inferior surface of the cerebellum, the frontal, temporal and occipital lobes, the ventral surface of the pons, medulla and cerebral peduncles, the upper cervical cord and the ventral surface of the lumbosacral cord. Leptomeningeal infiltration is probably the most common cause of neurological symptoms in NMC patients [61, 91, 94, 125].
Associated brain and spinal cord malformations
Dandy-Walker malformation complex
The overall spectrum of the Dandy-Walker malformation (DWM) complex (i.e. (a) Dandy-Walker malformation; (b) Dandy-Walker variant; (c) mega-cisterna magna; and (d) posterior fossa arachnoid cyst) [94, 216], has been frequently reported in association with NCM [8, 33, 35, 38, 42, 52, 61, 71, 73, 90, 91, 94, 98,102,100, 102, 108, 119, 127, 131, 171, 193, 201, 216]. Several hypotheses have been raised to explain this, highly likely, non-casual association, including: (a) obstruction by melanocytes of the outgoing foramen of the 4th ventricle; (b) maldevelopment of the cerebellum and 4th ventricle induced by the leptomeningeal abnormalities; and (c) the most credited theory, which postulates that the leptomeningeal melanocytosis interferes with the normal inductive effects of primitive meningeal cells resulting in hypogenesis of the vermis and consequent retro-cerebellar cyst formation [ 61, 91, 216]: these inductive effects could be triggered by factors from the surrounding mesenchyme, in particular Forkhead box protein C1 (i.e. the protein product of FOXC1 gene), which stimulates production of stromal cell-derived factor 1-alpha (SDF1α) and bone morphogenic protein 2,4 (Bmp 2,4), key morphogens for cerebellar Purkinje and granule cell development, respectively; melanocytosis may also interfere with proliferation of neurons in the cerebellar external granular layer, a process stimulated by secretion of Sonic Hedgehog protein (SHH) [62, 216].
It has been suggested that the DWM complex, in line with the above hypotheses, might be an early marker of profound infiltration of melanocytes in the CNS and thus constitutes an increased risk for malignant transformation [61, 91, 216].
Other non-DWM nervous system malformations
Besides the DWM complex, CNS development in NCM is normal. However, a number of disruptions of the brain, cerebellum, posterior fossa, and spinal cord have been reported in association with NCM, including hemimegalencephaly, polymicrogyria, nodular heterotopia, corpus callosum hypogenesis, subdural arachnoid cysts, Chiari I and Chiari II malformations, syringomyelia, meningoceles, and occult spinal dysraphism [2, 23, 34, 61, 62, 91, 135, 220]. Most of, if not all, these malformations are very common brain malformations and, therefore, it is not clear if their presence, in any way, indicates their increased prevalence in NCM. Overall, either the DWM and the other non-DWM CNS malformations indicate that NCM could be regarded as a complex (neurocutaneous) malformation syndrome with predisposition to tumour formation.
Lipomas/lipomatosis
A few case reports relate the coexistence of giant CMN to lipomatosis and hemihypertrophy [71] and intraspinal lipoma [101], which are anomalies derived from abnormal development of the neural crest [61].
Other associated systemic anomalies
These include anectodic reports of urinary tract anomalies (e.g. renal agenesis, renal pelvis and urethral malformations, renal cysts), Hirschprung’s disease, transposition of the great vessels, duodenal atresia and neoplasms (e.g. embryonic rhabdomyosarcoma, melanoblastoma, malignant schwannoma, and neuroectodermal neoplasm) [54, 61, 93, 109, 125].
Pathology/neuropathology
Types and distribution of intracranial melanin
Normal intracranial melanin occurs only in two forms: (1) melanosomic melanin (Fig. 2); and (2) neuromelanin [61, 141]. In both forms, melanin appears as granules: however, either form is different from an ultrastructural viewpoint. Melanosomic melanin (or “true” melanin) is the same type of melanin as that seen in the skin and iris of the eye. These melanin granules are confined to melanosomes within melanocytes (Fig. 2). Neuromelanin, on the other hand, presents as scattered intraneuronal inclusions of granular melanin not contained within melanosomes. The distribution of these two types of melanin in the nervous system is also different. In the brain, melanosomic melanin is normally found only in the leptomeninges, where it is contained in melanocytes. They are most concentrated in the leptomeninges over the ventral aspect of the medulla oblongata [61, 88, 141]. Baader, in 1935 [12] found those cells most prominently in the sulcus between pons and medulla, over the cerebral peduncles and over the base of the brain. Symmers, in 1905 [206], described these areas of pigmentation also at the level of the lumbar and cervical enlargements and optic chiasm. Neuromelanin is confined to certain groups of neurons such as the zona compacta of the substantia nigra, locus coeruleus, dorsal motor nucleus of the vagus, tegmentum of the brainstem, and scattered neurons in the roof of the fourth ventricle. The number of melanocytes increases slowly with age and, in general, is proportionate to skin pigmentation [68, 88, 141, 206]. Roca de Vinals and colleagues [168] found melanocytes in the pia mater/arachnoid in 85% of normal adults studied at autopsy. Less frequently, melanocytes also have been identified in the meninges of young infants (aged 2 months), and even in foetuses [59].
Neuropathological findings
Aggregates of melanocytes often form dark nodules of variable size resembling tumours, but more often form a nodular sheet or patch of black tissue covering brainstem, cerebellum, and the spinal cord. The brain parenchyma is infiltrated, particularly via the perivascular Virchow-Robin spaces [64, 188], and the choroid plexi and ependymal surface of the ventricles also are involved [47]. The lumen of distended meningeal and cerebral blood vessels, particularly veins, may be engorged with melanocytes [59].
At neurosurgery (Fig. 17) and/or at gross pathology of the brain, dark melanotic meninges are noted not only at the surface but also between cerebellar folia and in the sulci of the cerebral cortex [211]. Gross melanotic aggregates infiltrate the parenchyma, particularly the amygdala (less the hippocampus or other parts of the temporal lobe). Hamartomas of the amygdala have been also recorded in children [67]. Normally there are no melanocytes in the amygdala. Other sites of pigmented melanocytic infiltration include the cerebellar dentate nuclei, thalami, the area postrema, and the base of the frontal lobes [15, 16, 20, 47, 61, 64, 201]. Normally pigmented neurons of the brain in the substantia nigra and locus coeruleus are usually spared. Parenchymal pigmented lesions have a stronger predilection for grey vs. white matter [64]. An exception is the optic nerves and chiasm, in which neoplastic transformation to melanoma also may occur [59, 64, 188].
The accumulation of melanocytes in the leptomeninges is predominantly infratentorial and around the spinal cord, but can also occur supratentorially over the cerebral convexities and may be extensive [42, 55, 64, 198].
Microscopically, the aggregates of melanocytes contain melanin within melanosomes. These vesicular organelles are related to lysosomes (Fig. 2) [111]. The cells generally are not anaplastic and mitoses are infrequent. Melanocytes may be pleomorphic, fusiform (spindle-shaped, bipolar), round, oval, or polygonal often arranged in clusters, cords, or nests, but not rosettes [64, 72, 131, 211]. Sub-ventricular nodules, if large, may denude the overlying ependyma. These nodules occur not only in the lateral ventricles but also in the third and fourth ventricles. Nuclei show little variation in shape or internal structure. However, the degree of pigmentation varies considerably from one area to another [59, 64].
The histopathological features of the cutaneous nevi are identical to those found in CMN without leptomeningeal melanocytosis, including nevus cells extending into the dermis or into the deep dermis or even the subcutis, surrounding nerve, and blood vessels [52, 134].
Ultrastructure enables a classification of four stages of maturation of melanosomes (Fig. 2), including melanin deposition within it, completely filled by stage 4; proteolytic processing of melanosomal matrix proteins in stage 1 delays catalytic function and melanin synthesis until the melanosome becomes a mature organelle [111]. Pigmented cells of meningeal melanocytosis without cutaneous lesions exhibit similar ultrastructure [118].
The high incidence of association of NCM with DWM complex can be understood within the context of meningeal neural crest tissue. It may be related to a defective ectodermal/mesodermal interaction between meninges and cerebellum [15, 16, 215]. Because the cerebellum develops from midline fusion of bilateral dorsal growth of the rhombic lips of His, unlike the cleavage of the prosencephalon, the presence of abnormal leptomeninges with foetal melanocytes may impair fusion or normal deposition of extracellular matrix [52, 199]. Failure of fusion of the cerebellar primordia leads to hypoplasia of the posterior vermis and a widely open vallecula (i.e. foramen of Magendie), through which the fourth ventricle expands to form a voluminous cyst in the cisterna magna. Cerebellar granule cell proliferation and migration is not completed until 18 months of age. Normal cerebellar development requires hepatocyte growth factor (HGF) signalling and its receptor Met, localised to granule cell precursors [61, 91, 215]. Interference with HGF or Met by abnormal meninges may impede cerebellar maturation even postnatally.
The lineages and identity of melanocytes in the meninges, can be confirmed by immunohistochemistry markers of melanocytes, which include S-100b protein, human melanoma black-45 (HMB-45), and Melan-A and tyrosinase [20, 67, 119, 131].
Malignancy
Meningeal lesions, presenting as masses, form a spectrum ranging from “well-differentiated” melanocytomas, to lesions of intermediate malignancy, to overtly malignant melanomas [61, 91, 215]. Melanocytomas as solitary low-grade tumours do not invade surrounding structures. They usually are characterised by a benign clinical course, but local recurrence may occur. Intermediate lesions exhibit histological features suggestive of more aggressive behaviour, such as invasion of the CNS, but lack the overt cytological atypia of melanoma. Distinction between “benign” melanocytosis and malignant melanoma is much more difficult to determine in the meninges and CNS than in skin. The usual criteria of malignant transformation applied to the skin in the development of melanoma are infiltration of surrounding tissue by individual melanocytes, high mitotic and proliferative indices, and cellular and nuclear pleomorphism. All of these features are seen in melanocytosis of the CNS without necessarily denoting neoplastic transformation. Atypia and frank anaplasia are rare but, when it occurs and if necrosis is part of the lesion and cannot be attributed to chemo- or radiotherapy, the diagnosis of melanoma is more definite in the meninges and CNS. Another criterion for melanoma rather than melanocytosis in the CNS is rapid growth and behaviour as a mass lesion. Nodular proliferations in subependymal regions or in the periphery of the brain are not necessarily neoplastic. Necrosis with or without hemorrhage often accompanies malignancy but also can be secondary to radiotherapy or chemotherapy. However, infiltrates into the periphery of the CNS at any level by melanocytes does not cause parenchymal destruction and even myelinated axons coursing next to the infiltrates are well preserved.
Melanocytosis can cause obstructive hydrocephalus and can also be life-threatening by infiltrating essential brainstem structures of autonomic and respiratory function without histological criteria of malignancy. Despite the above reservations about diagnosis of malignancy, frontal, occipital and temporal lobe melanomas arising within the parenchymal infiltrations are well described [64, 131, 132, 202] and intracerebellar lesions were amongst the earliest recognised, but any of the parenchymal or extra-axial lesions are capable of malignant transformation, as with the cutaneous lesions. Mitoses are reported by some authors as rare in benign melanocytosis but become more frequent with conversion to melanoma [132]; mitotic figures can be frequent in benign melanocytic proliferative lesions. Malignant transformation into melanoma occurs in the meningeal lesions, particularly those around the cerebellum [115]. Differences between nodular melanocytosis and true melanoma have a basis in genetic mutation hence genetic studies should complement neuropathology.
Natural history
The characteristic NCM skin lesions (i.e. single LCMN or multiple CMN), are typically evident at birth. During the first years of life, the small satellite nevi may appear. Neurological manifestations may appear acutely during infancy or more often, later in childhood (Figs. 6b, c, 7b, 14b, 16 and 17) or even in adult life.
The risk of developing symptomatic NCM in an individual with LCMNs is 2.5–11%, especially when LCMNs are widely extensive an/or located in the facial region and/or in the posterior axis with satellite melanotic nevi [2, 45]. In about 2.5–15% patients with LCMNs, malignant melanoma may ensue [25, 78, 131, 132]. The prognosis in symptomatic NCM is poor, even in the absence of malignant melanoma [40, 70, 137].
The prognosis for asymptomatic patients is more difficult to predict [62]. Clinically, neurological manifestations of NCM usually appear in the first 2 years of life. Median survival time is 6.5 years after onset of symptoms, with more than 50% of deaths within the first 3 years from onset of neurological manifestations [2, 123, 192]. NCM associated with the DWM complex is usually at higher risk for rapid neurological deterioration, with death usually occurring by age 4 years [61].
Patients with leptomeningeal involvement have a potential for malignant degeneration with prevalence figures ranging from 40 to 65% according to different reports [124, 125].
In the past [45], severe/lethal disease was recorded in up of 92% of affected individuals, but more recent NCM surveys record lack of progression of abnormal imaging and/or lack of development of symptoms, for decades, after abnormal imaging [61, 91, 215].
Overall, an increased lifetime risk of CNS melanoma is associated with clinical and imaging signs of NCM, but the latter do not necessarily signify the eventual development of NCM during childhood [94]. Recommended treatment is the early removal of large CMN, which have a high incidence of malignant degeneration and metastatic potential (see below).
NCM has been detected as early as in the foetal period [89, 95].
NCM can appear at later/older ages: manifestations appearing later in life are usually chronic and may be associated with neuropsychiatric manifestations, including depression or psychosis [11]. The oldest recorded NCM patient who became symptomatic later in life was a 65 year-old woman, [103].
Molecular genetics/pathogenesis
Molecular genetics
Bauer et al. [19] demonstrated that NRAS rather than BRAF gene mutations [50] led to CMN. However, it was Dessars and colleagues, later on [51], who first identified a postzygotic somatic NRAS (neuroblastoma RAS viral oncogene homologue) proto-oncogene (MIM # 164790; located on chromosome 1p13.2) mutation in samples from 19 (70%) of 27 patients with CMN syndrome (CMNS; MIM # 137550): specifically, 14 nevi carried a Q61K mutation (164790.0008), 4 carried a Q61R mutation (164790.0002), and 1 carried a G13R mutation (164790.0001).
Kinsler and colleagues [105] identified somatic oncogenic missense mutations affecting codon 61 of the NRAS gene, in affected cutaneous and brain tissues from 12 of 15 patients with CMN syndrome and/or NCM. Affected skin samples from 10 of 13 patients carried a somatic heterozygous mutation, including 8 with Q61K (164790.0008) and 2 with Q61R (164790.0002). The same codon 61 mutation was found in each of the anatomically separate melanocytic nevi from the same patient. In addition, all the 11 brain samples from 5 patients from whom neurologic tissue was available were positive for a somatic Q61K mutation; this included both melanocytic and non-melanocytic tissue, such as a choroid plexus papilloma and meningioma. In patients with both neurologic and skin samples available, the same mutation was present in both affected tissues. None of the patients carried an NRAS mutation in the blood. Pre- and post-malignant skin tissue, obtained from a patient with malignant melanoma, showed a progression from heterozygosity to homozygosity for the Q61K mutation with the onset of malignancy. Mutations at codon 61 in the NRAS gene affect the guanosine triphosphate-binding site and result in constitutive activation of NRAS [105].
Charbel and colleagues [39] studied a series of large and giant CMNs and compared them with small and medium CMNs using complex genomic strategies. Large/giant CMNs displayed NRAS mutations in 94.7% of cases (18/19): in addition to that, NRAS mutation was the sole recurrent somatic event found in such melanocytic proliferations. The genetic profile of small-medium CMNs was significantly different, with 70% of cases bearing NRAS mutations and 30% showing BRAF mutations.
Similar findings have been also recorded by Dereure [48], Shih and colleagues [197], Guegan and colleagues [75], Girolami and colleagues [69] and Martins da Silva and colleagues [129] either in CMN and in diffuse leptomeningeal and brain parenchymal infiltration [129, 162, 203].
Gene function
The NRAS gene is a member of the RAS gene (GTPase) family, which includes the HRAS (Harvey rat sarcoma, or transforming protein p21; MIM # 190020; on chromosome 11p15.5) and KRAS (V-K1-RAS2-Kirsten rat sarcoma; MIM # 190070; on chromosome 12p12.1) proto-oncogenes, encoding for GTPase proteins, which primarily regulate cell division and proliferation, and apoptosis through important RAS cell-signalling pathways, including the RAS/MEK/ERK pathway and phosphatidylinositol 3-kinase-mediated Akt pathway [147, 148, 228]. The NRAS protein product through signal transduction, relays signals to the cell’s nucleus, instructing the cell to proliferate or to differentiate. N-Ras can be bound to a GTP molecule (activated form) or to a GDP molecule (conversion of GTP into GDP, inactivated form) [228].
Pathogenic mechanisms
The RAS gene/GTPase family (i.e. NRAS, HRAS, and KRAS) is involved in carcinogenesis in a number of tumours including, bladder, breast, gastric, lung, pancreatic, colorectal, skin, and thyroid neoplasms and blood cancers [147, 228].
The findings of Dessars and colleagues [51], Kinsler and colleagues [105], Charbel and colleagues [39], Dereure [48], Shih and colleagues [197], Salgado and colleagues [186], Guegan and colleagues [75], Girolami and colleagues [69], and Martins da Silva and colleagues [129] nicely demonstrated that single/multiple [small, medium-sized, and large/giant) CMNs and NCM, as well as non-melanocytic CNS lesions, result from somatic mosaicism, the mutation probably occurring in a progenitor cell in the developing neural crest or neuro-ectoderm, lethal in the germline [129, 162, 203]. These findings also strongly suggested that NRAS mutations are sufficient to drive melanocytic benign proliferations in utero (reviewed in [129, 162, 203] (Fig. 1).
The mechanisms underlying malignant progression in patients with large and/or giant CMN still remain obscure (Fig. 1). Salgado and colleagues [186], by describing novel genetic findings in a 17-month-old boy with a “bathing-trunk” CMN succumbed to congenital metastatic melanoma of the brain, spinal cord, lung, liver, testis, bone marrow, and, retrospectively, of the placenta, tentatively explained possible mechanisms resulting in the most severe form of NCM. Next-generation sequencing and chromosome microarray revealed in this boy duplication of a mutated NRAS gene, leading to an aggressive clinical course and disseminated disease; quantitative PCR showed a five-fold increase in NRAS protein expression in the melanoma cell line vs. normal melanocytes. Three amino acid-changing germline variants were detected, including homozygous TP53 p.P72R, heterozygous KIT p.M541L, and homozygous KDR (VEGFR2) p.Q472H: notably, all these three genes are involved in malignancy and other potentially relevant pathways, such as mast cell and melanocytic signalling, as well as angiogenesis.
Takahashi and colleagues [207, 208] had explored a different mechanism in the RB1 (retinoblastoma transcriptional co-repressor 1; MIM # 614041) gene, which is known to predispose humans and mice to tumour development. He had assessed the effect of NRAS loss on tumour development in Rb1 heterozygous mice [207, 208]. Loss of 1 or 2 NRAS alleles significantly reduced the severity of pituitary tumours arising in Rb1 +/− animals by enhancing their differentiation. By contrast, C-cell thyroid adenomas occurring in Rb1 +/− mice progressed to metastatic medullary carcinomas after loss of NRAS. In Rb1/Nras doubly heterozygous mice, distant medullary thyroid carcinoma metastases were associated with loss of the remaining wild type Nras allele. Loss of NRAS in Rb1-deficient C cells resulted in elevated RAS homologue family A (RhoA) activity, and this was causally linked to the invasiveness and metastatic behaviour of these cells [207, 208].
Thus, it seems that either amplification of mutated NRAS [207, 208] or the loss of NRAS [186], in certain cellular contexts (e.g. melanocytes in CMNs/NCM), represent new genetic mechanisms leading to melanoma and/or promoting malignant tumour progression [129, 162, 203].
Biologically targeted therapies
All these findings prompted the development of biologically targeted therapies in NCM, which so far successfully tailored: (a) MEK pathway (e.g. the acute MEK inhibitor MEK162) in a murine model [157]; (b) the dual PI3K/+mTOR pathway (e.g. Omipalisib/GSK2126458) in clonigenic oncogenically transformed NCM-derived cells [18]; and (c) the RAS-ERK pathway (e.g. vemurafenib and trametinib) in LCMNs cells [79, 136, 226]; or (d) generated platforms with NCM cells (YP-MEL) for pre-clinical studies [170].
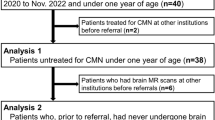
Diagnostic work-up and surveillance protocols
The diagnosis of NCM is based principally upon physical and accurate dermatological examination, dermoscopy, and early (i.e. the first few months) imaging (MRI) of the brain and spinal cord [61, 91, 216, 217]. Genetic testing (i.e. MPLA and/or NGS or sequencing) for NRAS gene mutations could confirm the clinical/imaging diagnosis [129, 162, 203].
The characteristic skin lesions found at birth usually are the first manifestations of NCM [61, 91, 129, 151]. CMN can easily be diagnosed at glance; satellite nevi could require additional evaluation and dermoscopy. Plastic surgeons should be contacted immediately after referral for optioning partial/near-total surgical removal. On clinical examination only, Ruiz-Maldonado and colleagues [185], found neurological abnormalities, such as mild or minimal motor deficits, nerve dysfunction, and impaired mental status in patients thought to be asymptomatic.
The melanocytic nevi should be examined by parents at home once a month and by a physician every 6 months with dermoscopy and serial photographs for later comparison. Neurologically asymptomatic patients should be followed with repeated neurological examination.
CT scan of the brain (and spinal cord) in children with NCM may show associated hypoplasia of the pons and cerebellum, but the foci of melanin-containing cells show only subtle hyperdensity and are difficult to see unless they have converted to melanoma [15, 16, 216, 217].
Brain and spinal cord MRI demonstrates increased signal intensity on T1-weighted images without contrast and decreased signal intensity on T2-weighted sequences (diffuse or localised in the leptomeninges, associated or not with cortical and subcortical plaque(s) and/or nodular lesions), which reflect the paramagnetic properties of stable free radicals within melanin pigment (Fig. 16) [31, 47, 70]. The conspicuity of these MRI lesions is variable, becoming less conspicuous on both T1- and T2-weighted images (more so on T2) with maturity/myelination, with some lesions no longer visible by age 3–5 years; in addition to that, melanin resorption by macrophages could make it less conspicuous. Therefore, it is important to image these patients early in order to identify the melanocytosis. Recommendations include early MRI (first few months) when quality scans can be obtained during natural sleep without sedation [15, 16, 94, 216].
The amygdala (40%), pons (20%) and cerebellum (15%) are the most common locations of melanocytosis, followed by the cerebral cortex, thalamus, midbrain, and medulla. Macroscopic pigmentation may be seen in normal patients under physiological conditions; excessive benign melanotic cells, in the meninges, rather than their distribution, differentiates pathological melanosis from physiological pigmentation. The pia/arachnoid invaginates into the brain with developing blood vessels to form the perivascular spaces. In NCM, melanotic cells infiltrate and fill the perivascular spaces; they do not extend into the Virchow-Robin spaces under normal physiological conditions. The absence of oedema, necrosis, or haemorrhage on initial or available follow-up scans also suggests benign lesions. However, MRI cannot distinguish benign from malignant melanocytes: malignant melanomas may lack oedema, haemorrhage and necrosis. Moreover, non-contrast MR images lack sensitivity in detecting leptomeningeal melanocytic infiltration unless malignant degeneration occurs; new presence of leptomeningeal enhancement or growth on sequential scans should raise suspicion for malignant transformation [94, 216, 217].
Hindbrain malformations, including small or dysmorphic pons or cerebellar hemispheres, or hypoplasia of the inferior vermis, are recorded and are significantly associated with simultaneous hindbrain melanosis. However, cerebellar melanosis is often transient, disappearing with brain maturation. Additional findings include loss of visibility of cerebellar melanosis in hypoplastic regions, with or without cerebellar volume loss on follow-up MRI; thus, it is not clear that the melanosis is causative. This association may be explained by interference with the effects of factors from the surrounding mesenchyme, in particular Forkhead box protein C1 (i.e. the protein product of FOXC1 gene), which stimulates production of stromal cell-derived factor 1-alpha (SDF1α) and bone morphogenic protein 2,4 (Bmp 2,4), key morphogens for cerebellar Purkinje and granule cell development, respectively. Melanosis may also interfere with proliferation of neurons in the cerebellar external granular layer, a process stimulated by secretion of Sonic Hedgehog protein (SHH). If melanosis is limited to the vermis, the malformation may resemble Dandy-Walker malformation. Whatever the mechanism, cerebellar hypoplasia in the setting of CMN is strongly suggestive of NCM and its presence should stimulate a search for other manifestations. Evaluating these patients with new advanced imaging techniques may help better understand these hindbrain anomalies [94, 217].
MRI of the CNS has been recognised as a useful screening for NCM in asymptomatic patients with LCMN [94, 215]. In 25% of asymptomatic infants with LCMN and/or MCMN, MRI allows the detection of CNS melanocytosis. The most common findings in this group, are T1-signal shortening compatible with melanin deposits in the infratentorial structures [2, 33, 40, 94, 217]. FLAIR sequences well record leptomeningeal hyperintensities [15, 94]. Neuroimaging is also of utmost importance in the diagnostic work-up of associated CNS malformations, including the DWM complex.
In an ideal setting of experienced pediatric radiologists, a more sophisticated diagnostic and follow-up approach is recommended for NCM. In the very young infant (< 4–5 months old), non-contrast heavily T1- and T2-weighted volumetric sequences using small voxel size (≤ 1 × 1 × 1 mm), with reformations in three (or more) orthogonal planes, should be sufficient for the initial MRI performed; nevi are rather easily detected in unmyelinated brain. As the brain matures (myelination, size) over the middle and later months of the first year, the melanocytosis becomes more difficult to identify and additional sequences such as diffusion-weighted imaging (DWI), SWI and contrast-enhanced T1 images become necessary to detect melanocytosis; imaging at 3 T improves the sensitivity of these (especially SWI). In addition, the use of advanced sequences such as diffusion tensor imaging and thin section volumetric acquisitions may reveal additional lesions; however, some level of sedation may be necessary. Finally, the use of earmuffs and earplugs along with a blanket to keep the baby warm whilst minimizing motion degradation during acquisition of volumetric T1 and T2 images with 1-mm or sub-millimetre thickness allows detection of even small melanotic foci and excel- lent assessment for associated malformations [56, 94, 216].
As MRI cannot detect malignant transformation of benign CNS melanocytosis, [F-18]2-fluoro-2-deoxyglucose (FDG) [53] and C-11-methionine positron emission tomography/computed tomography (PET/CT), has been used in suggesting clues to a diagnosis of malignant transformation, but diffuse leptomeningeal radiotracer uptake is sometimes noted in melanocytic infiltration with no histopathological evidence of malignancy, suggesting that it may reflect increased cell glucose and amino acid metabolism [32]. Thus, detection of malignant transformation remains a difficult task [94, 216, 217]. Most likely, new neurological symptoms, imaging signs such as oedema adjacent to melanosis, or rapid growth of melanosis are the best indications of malignancy.
The risk of patients, with initial negative imaging evidence of melanocytosis, later developing melanocytosis or malignant melanoma remains unknown. The lifetime risk of developing neurological symptoms remains unknown but may be low.
CSF analyses record increased CSF pressure, elevated protein, aseptic leukocytosis, and normal glucose and, thus, could result falsely negative. Conversely, the presence of melanin-containing cells may support the diagnosis of NCM [4, 125].
Video-EEG recordings may be useful for studying eventual jerks or seizure-like episodes and could help in localising the CNS infiltration, if any. Especially when seizures appear focal or generalised, abnormalities may be detected [153, 158].
Differential diagnosis
Differential diagnosis may require cooperation between dermatologists, neurologists, and expert paediatric radiologists.
Differential diagnosis of NCM should be carried out with respect to:
-
1.
Solitary or multiple, benign, small, or medium-sized CMN of the skin not associated with nervous system and/or systemic involvement;
-
2.
CMNS, or giant pigmented hairy nevus syndrome (or GPHN, giant congenital pigmented nevus, or pigmented moles; MIM # 137550), caused by mutations in NRAS (neuroblastoma RAS viral oncogene homologue; MIM # 164790; on chromosome 1p13.2) proto-oncogene [147, 148];
-
3.
Primary malignant melanoma of the leptomeninges;
-
4.
Metastatic melanoma or intracranial dissemination of malignant melanoma of the skin—found at any age;
-
5.
Progonoma: a benign pigmented neuroectodermal tumour of infancy, with different tissue components in addition to melanotic cells, which appears in cranial bones and in neighbouring areas of the meninges, without infiltration of the brain;
-
6.
Melanotic nerve sheath tumour: a solitary, melanin-bearing slow-growing plexiform neurofibroma with no metastases;
-
7.
Familial progressive hyperpigmentation with or without hypopigmentation (FPHH; melanosis universalis hereditaria or MUH; MIM # 145250; on chromosome 12q21.32; ORPHA: 79146) [147, 148], caused by mutations in KITLG (v-KIT sarcoma viral ligand; MIM # 184745) proto-oncogene, characterised by diffuse hyperpigmentation of variable intensity with café-au-lait spots, associated or not with large leaf-shaped areas of depigmentation, and sometimes with retarded growth and cognitive disability.
Management
Skin lesions
The treatment of large/giant CMNs is still a challenge, including serial resection, resection with skin grafting, and resection and coverage with expanded skin flap (skin expanders) [74, 77, 139].
Non-surgical treatments, such as laser therapy, chemical peeling, and dermabrasion, only remove superficial pigment and nevus cells in the dermis. Recurrence of the pigment is common, and the remaining nevus cells deep in the lesion still have malignant transformation potential [61, 91].
Skin grafts and tissue expansion can completely remove the lesion, thus further reducing the potential risk for malignant transformation and improving the overall cosmetic burden and outcome. However, even experienced surgeons become stranded when the nevus involves too large an area on the body [77, 86, 139, 226].
Patients after excision are left with large wounds that are difficult to close. Traditionally, these defects have been repaired with split-thickness skin grafts, full-thickness skin grafts, the use of tissue expanders and a variety of flaps and power-stretching of the skin [77]. Complete excision of giant nevus involves multiple surgical procedures starting in early infancy and completing the work-up in adolescence [9]. These surgical excisions cause scarring, which creates further problems. Dermabrasion is probably less effective in reducing the risk of malignancy. Removal of cutaneous lesions does not reduce the risk of CNS malignant melanoma. Some authors do not recommend undertaking surgical procedures in symptomatic patients because of their poor prognosis [134].
Recently, new methods have been developed for the closure of large skin defects in pediatric patients with the use of tissue expansion [121], artificial skin substitutes, and/or with epidermis and superficial dermis of the lesions [74]. Advantages include coverage of large wounds, decrease or elimination of donor site pain and morbidity, and decreased scarring and wound contractures [61, 91].
Nervous system lesions
Shunt insertion (ventriculo-peritoneal or cysto-peritoneal) is an effective palliative measure for patients with NCM and associated hydrocephalus (Fig. 17) [52, 146, 196]. Despite treatment, however, the prognosis of these patients remains poor owing to malignant progression and leptomeningeal spread of lesions, in particular, in cases associated with the DWM complex. A cell filter in the shunt tubing may limit the spread of malignant cells, but may increase the risk of obstruction [121, 153, 160]. If the syringomyelia is associated with NCM the syrinx drainage should be considered.
Children with seizures and/or epilepsy should be treated with anticonvulsant medication. In refractory epilepsy with amygdala infiltration, control can be achieved with anterior temporal lobectomy and hippocampectomy [67].
The radicular pain secondary to infiltration of the roots should be treated with analgetics [153].
Medical treatment
Treatment options for symptomatic NCM are unsatisfactory. In addition to conventional treatment of seizures, for malignant melanoma, combinations of chemotherapy (vincristine, dacarbazine, cyclophosphamide, and intraventricular methotrexate] can result in improvement and prolong the patient’s survival [40]. Repeated cycles may be given. Rapid response to chemotherapy (i.e. combination of cyclophosphamide, sorafenib, and temozolomide) and radiotherapy has been also reported [205]. Usually, however, chemo- and radiotherapy, show relatively poor on symptoms and no effects on survival [2, 52, 160].
In cases of intractable pruritus, ondansetron, a selective antagonist of 5-hydroxytryptamine type 3 receptors, can show efficacy [60, 66].
Mir and colleagues [136] treated a 7-year-old girl with a giant congenital melanocytic nevus and an AKAP9-BRAF fusion with trametinib, which resulted in rapid resolution of the patient's lifelong, intractable pain and pruritus as well as dramatic improvement in the extent of her nevus.
In cases with extremely poor prognosis, psychological support of the family is of utmost importance.
References
Abbo O, Dubedout S, Ballouhey Q, Maza A, Sevely A, Galinier P (2012) Asymptomatic neonatal neurocutaneous melanosis. Arch Pediatr 19:1319–1321. https://doi.org/10.1016/j.arcped.2012.09.009
Acosta FL Jr, Binder DK, Barkovich AJ, Frieden IJ, Gupta N (2005) Neurocutaneous melanosis presenting with hydrocephalus. J Neurosurg 102:96–100. https://doi.org/10.3171/ped.2005.102.1.0096
Agero AL, Benvenuto-Andrade C, Dusza SW, Halpern AC, Marghoob AA (2005) Asymptomatic neurocutaneous melanocytosis in patients with large congenital melanocytic nevi: a study of cases from an Internet-based registry. J Am Acad Dermatol 53:959–965. https://doi.org/10.1016/j.jaad.2005.07.046
Akinwunmi J, Sgouros S, Moss C, Grundy R, Green S (2001) Neurocutaneous melanosis with leptomeningeal melanoma. Pediatr Neurosurg 35:277–279. https://doi.org/10.1159/000050437
Alikhan A, Ibrahimi OA, Eisen DB (2012) Congenital melanocytic nevi: where are we now? Part I. Clinical presentation, epidemiology, pathogenesis, histology, malignant transformation, and neurocutaneous melanosis. J Amer Acad Dermatol 67:495.e1-17; quiz 512-4. https://doi.org/10.1016/j.jaad.2012.06.023
Andermann F, Mathieson G, Wilkinson RD (1980) Amygdaloid melanosis: a form of neurocutaneous melanosis associated with partial complex seizures. In: Canger R, Angeleri F, Penry K (eds) Adv Epileptol: XIth International Epilepsy Congress. Raven Press, New York, pp 115–122
Ansarin H, Soltani-Arabshahi R, Mehregan D, Shayanfar N, Soltanzadeh P (2006) Giant congenital melanocytic nevus with neurofibroma-like changes and spina bifida occulta. Int J Dermatol 45:1347–1350. https://doi.org/10.1111/j.1365-4632.2006.02776.x
Arai M, Nosaka K, Kashihara K, Kaizaki Y (2004) Neurocutaneous melanosis associated with Dandy–Walker malformation and a meningohydroencephalocele. J Neurosurg 100:501–505. https://doi.org/10.3171/ped.2004.100.5.0501
Arneja JS, Gosain AK (2007) Giant congenital melanocytic nevi. Plast Reconstr Surg 120:26–40e. https://doi.org/10.1097/01.prs.0000267583.63342.0a
Asanuma K, Kasai Y, Takegami K, Ito H, Yoshikawa T, Uchida A (2008) Spinal neurocutaneous melanosis without cutaneous nevi. Spine (Phila Pa 1976) 33:E798–E801. https://doi.org/10.1097/BRS.0b013e3181808c9a
Azzoni A, Argentieri R, Raja M (2001) Neurocutaneous melanosis and psychosis: a case report. Psychiatry Clin Neurosci 55:93–95. https://doi.org/10.1046/j.1440-1819.2001.00794.x
Baader O (1935) Über die Piamelanose. Zeitschrift fur Zellforschung und Mikroskopische Anat 22:735–753
Ball RA, Genest D, Sander M, Schmidt B, Barnhill RL (1998) Congenital melanocytic nevi with placental infiltration by melanocytes. Arch Dermatol 134:711–714. https://doi.org/10.1001/archderm.134.6.711
Barbarot S (2015) Revisiting neurocutaneous melanosis spectrum: do we have to undertake systematic magnetic resonance imaging in children with congenital melanocytic naevi? Br J Dermatol 173:639–640. https://doi.org/10.1111/bjd.13976
Barkovich AJ, Raybaud C (2019) Pediatric neuroimaging, 6th edn. Wolters Kuver, Philadelphia
Barkovich AJ, Frieden IJ, Williams ML (1994) MR of neurocutaneous melanosis. AJNR Am J Neuroradiol 15:859–867
Bastian BC (2014) The molecular pathology of melanoma: an integrated taxonomy of melanocytic neoplasia. Annu Rev Pathol 9:239–271. https://doi.org/10.1146/annurev-pathol-012513-104658
Basu D, Salgado CM, Bauer B, Khakoo Y, Patel JR, Hoehl RM, Bertolini DM, Zabec J, Brzozowski MR, Reyes-Múgica M (2018) The dual PI3K/mToR Inhibitor omipalisib/GSK2126458 inhibits clonogenic growth in oncogenically-transformed cells from neurocutaneous melanocytosis. Cancer Genomics Proteomics 15:239–248
Bauer J, Curtin JA, Pinkel D, Bastian BC (2007) Congenital melanocytic nevi frequently harbor NRAS mutations but no BRAF mutations. J Invest Dermatol 127:179–182. https://doi.org/10.1038/sj.jid.5700490
Becher OJ, Souweidane M, Lavi E, Kramer K, Lis E, Marghoob AA, Kakhoo Y (2009) Large congenital melanotic nevi in an extremity with neurocutaneous melanocytosis. Pediatr Dermatol 26:79–82. https://doi.org/10.1111/j.1525-1470.2008.00828.x
Beckwitt EC, Van Houten B (2017) Molecular cartography of mutational landscapes in melanomas. EMBO J 36:2812–2814. https://doi.org/10.15252/embj.201797944
Bekiesińska-Figatowska M, Sawicka E, Żak K, Szczygielski O (2016) Age related changes in brain MR appearance in the course of neurocutaneous melanosis. Eur J Radiol 85:1427–1431. https://doi.org/10.1016/j.ejrad.2016.05.014
Bett BJ (2006) Large or multiple congenital melanocytic nevi: occurrence of neurocutaneous melanocytosis in 1008 per- sons. J Am Acad Dermatol 54:767–777
Bircher MO (1897) Zur Aetiologie des Naevus pilosus pigmentosus congenitus extensus. Arch Derm Syph (Berlin) 41:195
Bittencourt FV, Marghoob AA, Kopf AW, Koenig KL, Bart RS (2000) Large congenital melanocytic nevi and the risk for development of malignant melanoma and neurocutaneous melanocytosis. Pediatrics 106:736–741. https://doi.org/10.1542/peds.106.4.736
Bolande RP (1974) The neurocristopathies: a unifying concept of disease arising in neural crest maldevelopment. Hum Pathol 5:409–429
Bolande RP (1997) Neurocristopathy: its growth and development in 20 years. Pediatr Pathol Lab Med 17:1–25
Bouton J (1958) Primary melanoma of the leptomeninges. J Clin Pathol 11:122–127
Brocheriou C, Kufferr VO (1985) Pigmented lesions of the oral cavity. Ann Pathol 5:221–229
Burstein F, Seier H, Hudgins PA, Zapiach L (2005) Neurocutaneous melanosis. J Craniofac Surg 16:874–876. https://doi.org/10.1097/01.scs.0000181050.06696.4d
Byrd SE, Reyes-Mugica M, Darling CF, Chou P, Tomita T (1995) MR of leptomeningeal melanosis in children. Eur J Radiol 20:93–99. https://doi.org/10.1016/0720-048x(95)00632-z
Cabanillas M, Ginarte M, Monteagudo B, Toribio J (2009) Role of positron emission tomography in the management of neurocutaneous melanocytosis. Pediatr Dermatol 26:351–352. https://doi.org/10.1111/j.1525-1470.2009.00915.x
Caceres A, Trejos H (2006) Neurocutaneous melanosis with associated Dandy–Walker complex. Childs Nerv Syst 22:67–72. https://doi.org/10.1007/s00381-004-1043-y
Cai C, Zhang Q, Yang W, Shen C (2008) Giant congenital melanocytic nevus coexistent with Chiari II malformation. Neuropediatrics 39:272–275. https://doi.org/10.1055/s-0028-1104576
Cajaiba MM, Benjamin D, Halaban R, Reyes-Mugica M (2008) Metastatic peritoneal neurocutaneous melanocytosis. Am J Surg Pathol 32:156–161. https://doi.org/10.1097/PAS.0b013e3181238cd2
Caldarelli M, Tamburrini G, Di Rocco F (2005) Neurocutaneous melanosis. J Neurosurg 103:382. https://doi.org/10.3171/ped.2005.103.4.0382
Caradona SA, Skidmore R, Gupta A, Bush CH, Ford MJ (2000) Giant congenital melanocytic nevus with underlying hypoplasia of the subcutaneous fat. Pediatr Dermatol 17:387–390. https://doi.org/10.1046/j.1525-1470.2000.017005387.x
Chaloupka JC, Wolf RJ, Varma PK (1996) Neurocutaneous melanosis with the Dandy-Walker malformation: a possible rare pathoetiologic association. Neuroradiology 38:486–489. https://doi.org/10.1007/bf00607285
Charbel C, Fontaine RH, Malouf GG, Picard A, Kadlub N, El-Murr N, How-Kit A, Su X, Coulomb-L’Hermine A, Tost J, Mourah S, Aractingi S, Guégan S (2014) NRAS mutation is the sole recurrent somatic mutation in large congenitalmelanocytic nevi. J Invest Dermatol 134:1067–1074
Chu WCW, Lee V, Chan Y, Shing MMK, Chik KW, Li CH, Ma KC (2003) Neurocutaneous melanomatosis with a rapidly deteriorating course. Am J Neuroradiol 24:287–290. https://doi.org/10.1177/088307389601100515
Cramer SF, Salgado CM, Reyes-Múgica M (2016) The high multiplicity of prenatal (congenital type) nevi in adolescents and adults. Pediatr Dev Pathol 19:409–416. https://doi.org/10.2350/15-06-1662-OA.1
Craver RD, Golladay SE, Warrier RP, Gates AJ, Nelson JS (1996) Neurocutaneous melanosis with Dandy–Walker malforma- tion complicated by primary spinal leptomeningeal melanoma. J Child Neurol 11:410–414. https://doi.org/10.1177/088307389601100515
Damsky WE, Bosenberg M (2017) Melanocytic nevi and melanoma: unraveling a complex relationship. Oncogene 36:5771–5792. https://doi.org/10.1038/onc.2017.189
de Andrade DO, Dravet C, Raybaud C, Broglin D, Laguitton V, Girard N (2004) An unusual case of neurocutaneous melanosis. Epileptic Disord 6:145–152
DeDavid M, Orlow SJ, Provost N, Marghoob AA, Rao BK, Wasti Q, Huang CL, Kopf AW, Bart RS (1996) Neurocutaneous melanosis: clinical features of large congenital melanocytic nevi in patients with manifest central nervous system melanosis. J Am Acad Dermatol 35:529–538. https://doi.org/10.1016/s0190-9622(96)90674-x
DeDavid M, Orlow SJ, Provost N, Marghoob AA, Rao BK, Huang CL, Wasti Q, Kopf AW, Bart RS (1997) A study of large congenital melanocytic nevi and associated malignantmelanomas: review of cases in the New York University Registry and the world literature. J Am Acad Dermatol 36:409–416. https://doi.org/10.1016/s0190-9622(97)80217-4
Demirci A, Kawamura Y, Sze G, Duncan C (1995) MR of parenchymal neurocutaneous melanosis. AJNR Am J Neuroradiol 16:603–606
Dereure O (2014) Neurocutaneous melanosis and multiple congenital melanocytic naevi are associated with post-zygotic N-ras mutations. Ann Dermatol Venereol 141:314–315. https://doi.org/10.1016/j.annder.2013.12.006
Derinkuyu BE, Boyunaga O, Unal S, Ucar M, Ergenekon E (2015) Neurocutaneous melanocytosis, hemimegalencephaly and large ovarian cyst in a newborn. Pediatr Radiol 45:1249–1252. https://doi.org/10.1007/s00247-015-3284-1
Dessars B, De Raeve LE, El Housni H, Debouck CJ, Sidon PJ, Morandini R, Roseeuw D, Ghanem GE, Vassart G, Heimann P (2007) Chromosomal translocations as a mechanism of BRAF activation in two cases of large congenital melanocytic nevi. J Invest Dermatol 127:1468–1470. https://doi.org/10.1038/sj.jid.5700725
Dessars B, De Raeve LE, Morandini R, Lefort A, El Housni H, Ghanem GE, Van den Eynde BJ, Ma W, Roseeuw D, Vassart G, Libert F, Heimann P (2009) Genotypic and gene expression studies in congenital melanocytic nevi: insight into initial steps of melanotumorigenesis. J Invest Dermatol 129:139–147. https://doi.org/10.1038/jid.2008.203
Di Rocco F, Sabatino G, Koutzoglou M, Battaglia D, Caldarelli M, Tamburrini G (2004) Neurocutaneous melanosis. Childs Nerv Syst 20:23–28. https://doi.org/10.1007/s00381-003-0835-9
D'Souza MM, Prasad A, Sachdev N, Manchanda S, Choudhary A, Sharma R, Jaimini A, Tripathi M, Mondal A (2011) Neurocutaneous melanosis: assessment on F-18 FDG and [11C]-methionine PET/CT and MRI. Clin Nucl Med 36:906–909. https://doi.org/10.1097/RLU.0b013e31821a290d
Dunin-Wąsowicz D, Jóźwiak S, Chrzanowska K, Dąbrowki D (1996) Neurocutaneous melanosis- report of cases. Neur Dziec 5:95–100
Earle SA, Marshall DM (2005) Management of giant congenital nevi with artificial skin substitutes in children. J Craniofac Surg 16:904–907. https://doi.org/10.1097/01.scs.0000180485.20043.d5
Edelstein S, Naidich TP, Newton TH (2005) The rare phakomatoses. In: Tortori-Donati P (ed) Pediatric neuroradiology. Brain. Springer, Berlin and Heidelberg, pp 819–854
El Mabood SA, Wahba Y, Yahia S, Sarhan MM, Mansour AK, Provenzano A, Elmahdi HS, Darwish A (2019) Neurocutaneous melanosis is not always a benign disease. Indian J Dermatol Venereol Leprol. https://doi.org/10.4103/ijdvl.IJDVL_456_18
Errichetti E, Patriarca MM, Stinco G (2017) Dermoscopy of congenital melanocytic nevi: a ten-year follow-up study and comparative analysis with acquired melanocytic nevi arising in prepubertal age. Eur J Dermatol 27:505–510. https://doi.org/10.1684/ejd.2017.3088
Farnell FJ, Globus JH (1931) Primary melanoblastosis of the leptomeninges and brain. Arch Neurol Psychiatr 25:803–823
Feng J, Sethi A, Reyes-Mugica M, Antaya R (2005) Life-threatening blood loss from scratching provoked by pruritus in the bulky perineal nevocytoma variant of giant congenital melanocytic nevus in a child. J Am Acad Dermatol 53:S139–S142. https://doi.org/10.1016/j.jaad.2004.12.040
Flores-Sarnat L (2013) Neurocutaneous melanocytosis. Handb Clin Neurol 111:369–378. https://doi.org/10.1016/B978-0-444-52891-9.00042-7
Foster RD, Williams ML, Barkovich AJ, Hoffman WY, Mathes SJ, Frieden IJ (2008) Giant congenital melanocytic nevi: the significance of neurocutaneous melanosis in neurologically asymptomatic children. Plast Reconstr Surg 107:933–941. https://doi.org/10.1097/00006534-200104010-00005
Fox H (1972) Neurocutaneous melanosis. Handb Clin Neurol 33:414–428
Fox H, Emery JL, Goodbody RA, Yates PO (1964) Neurocutaneous melanosis. Arch Dis Child 39:508–516. https://doi.org/10.1136/adc.39.207.508
Frieden I, Williams M, Barkovich AJ (1994) Giant congenital melanocytic nevi: brain magnetic resonance findings in neurologically asymptomatic children. J Am Acad Dematol 31:423–429. https://doi.org/10.1016/s0190-9622(94)70204-7
Frigon C, Desparmet J (2006) Ondansetron treatment in a child presenting with chronic intractable pruritus. Pain Res Manag 11:245–247. https://doi.org/10.1155/2006/873870
Fu YJ, Morota N, Nakagawa A, Takahashi H, Kakita A (2010) Neurocutaneous melanosis: surgical pathological features of an apparently hamartomatous lesion in the amygdala. J Neurosurg Pediatr 6:82–86. https://doi.org/10.3171/2010.3.PEDS1025
Gebarski SS, Blaivas MA (1996) Imaging of normal leptomeningeal melanin. AJNR Am J Neuroradiol 17:55–60
Girolami I, Cima L, Ghimenton C, Zannoni M, Mombello A, Riva G, Cirielli V, Corradi G, Vogrig A, Di Stefano G, Novelli L, Gessi M, Eccher A (2018) NRAS(Q61K) mutated diffuse leptomeningeal melanomatosis in an adult patient with a brief review of the so-called “forme fruste” ofneurocutaneous melanosis. Brain Tumor Pathol 35:217–223. https://doi.org/10.1007/s10014-018-0328-x
Gondo K, Kira R, Tokunaga Y, Hara T (2000) Age-related changes of the MR appearance of CNS involvement in neurocutaneous melanosis complex. Pediatr Radiol 30:866–868. https://doi.org/10.1007/s002470000348
Gonul M, Soylu S, Gul U, Aslan E, Unal T, Ergül G (2009) Giant congenital melanocytic naevus associated with Dandy-Walker malformation, lipomatosis and hemihypertrophy of the leg. Clin Exp Dermatol 34:e106–e109. https://doi.org/10.1111/j.1365-2230.2008.03191.x
Grahl F (1906) Angeborener ausgedehnter Naevus pigmentosus in Verbindung mit Pigmentfiecken im Gehirn. Beitr Pathol Anat 39:66–81
Green LJ, Nanda VS, Roth GM, Barr RJ (1997) Neurocutaneous melanosis and Dandy–Walker syndrome in an infant. Int J Dermatol 36:356–359. https://doi.org/10.1046/j.1365-4362.1997.d01-517.x
Gu C, Wang XX, Luo X, Liu F, Zhou XY, Yang J, Yang Q, Wang X (2018) An alternative strategy treated giant congenital melanocytic nevi with epidermis and superficial dermis of the lesions. Medicine (Baltimore) 97:e9725. https://doi.org/10.1097/MD.0000000000009725
Guégan S, Kadlub N, Picard A, Rouillé T, Charbel C, Coulomb-L'Hermine A, How-Kit A, Fraitag S, Aractingi S, Fontaine RH (2016) Varying proliferative and clonogenic potential in NRAS-mutated congenital melanocytic nevi according to size. Exp Dermatol 25:789–796. https://doi.org/10.1111/exd.13073
Guidetti V, Garcovich A, Giuffré R, Curatolo P (1978) Nevo gigante congenito e melanosi neurocutanea. Considerazioni su due casi clinici. Minerva Pediatr 30:1961–1972
Häfner HM, Breuninger H (2018) Serial excision with power-stretching of the skin in giant melanocyticnevi therapy. J Plast Reconstr Aesthet Surg 71:443–445. https://doi.org/10.1016/j.bjps.2017.11.011
Hale EK, Stein J, Ben-Porat L, Panageas KS, Eichenbaum MS, Marghoob AA, Osman T, Kopf AW, Polsky D (2005) Association of melanoma and neurocutaneous melanocytosis with large congenital melanocytic naevi – results from the NYU – LCMN registry. Br J Dermatol 152:512–517. https://doi.org/10.1111/j.1365-2133.2005.06316.x
Hao J, Fan W, Li Y, Tang R, Tian C, Yang Q, Zhu T, Diao C, Hu S, Chen M, Guo P, Long Q, Zhang C, Qin G, Yu W, Chen M, Li L, Qin L, Wang J, Zhang X, Ren Y, Zhou P, Zou L, Jiang K, Guo W, Deng W (2019) Melatonin synergizes BRAF-targeting agent vemurafenib in melanoma treatment by inhibiting iNOS/hTERT signaling and cancer-stem cell traits. J Exp Clin Cancer Res 38:48. https://doi.org/10.1186/s13046-019-1036-z
Happle R (1993a) Mosaicism in human skin. Understanding the patterns and mechanisms. Arch Dermatol 129:1460–1470
Happle R (1993b) Pigmentary patterns associated with human mosaicism: a proposed classification. Eur J Dermatol 3:170–174
Happle R (1996) Segmental forms of autosomal dominant skin disorders: different types of severity reflect different states of zygosity. Am J Med Genet 66:241–242. https://doi.org/10.1002/(SICI)1096-8628(19961211)66:2<241::AID-AJMG24>3.0.CO;2-S
Happle R (1997) A rule concerning the segmental manifestation of autosomal dominant skin disorders. Review of clinical examples providing evidence for dichotomous types of severity. Arch Dermatol 133:1505–1509
Happle R (2014) Mosaicism in human skin. understanding nevi, nevoid skin disorders, and cutaneous neoplasia. Springer-Verlag, Berlin/Heidlber
Happle R (2018) The concept of type 2 segmental mosaicism, expanding from dermatology to general medicine. J Eur Acad Dermatol Venereol 32:1075–1088. https://doi.org/10.1111/jdv.14838
Heffel DF, Thaller S (2005) Congenital melanosis: an update. J.Craniofac.Surg. 16(5):940–944. https://doi.org/10.1097/01.scs.0000179751.29284.51
Heuer S (1917) Ein Fall von ausgedehntem schwimmhosenar- tigem Naevus pigmentosus pilosus congenitus mit Hamatom des Ruckens und Spina bifido occulta: Seine Beziehung zur v Recklinghausen’schen Krankheit. Bruns Beitr Klin Chir 104:388–426
Hirano A (1991) Neurons and astrocytes. In: Davis RL, Robertson DM (eds) Textbook of neuropathology, 2nd edn. Williams & Wilkins, Baltimore, pp 15–18
Hosli I, Holzgreve W, Danzer E, Tercanli S (2001) Two case reports of rare fetal tumors: an indication for surface rendering? Ultrasound Obstet Gynecol 17:522–526. https://doi.org/10.1046/j.1469-0705.2001.00407.x
Hsueh C, Ho C, Chiu N, Shen EY (2004) Neurocutaneous melanosis with hydrocephalus: report of one case. Acta Neurol Taiwanica 13:29–33
Islam MP (2015) Neurocutaneous melanosis. Handb Clin Neurol 132:11–117. https://doi.org/10.1016/B978-0-444-62702-5.00007-X
Itin PH, Lautenschlager S (1998) Lower and upper extremity atrophy associated with a giant congenital melanocytic nevus. Pediatr Dermatol 15:287–289. https://doi.org/10.1046/j.1525-1470.1998.1998015287.x
Iwabuchi T, Shimotake T, Furukawa T, Tsuda T, Aoi S, Iwai N (2005) Neurocutaneous melanosis associated with Hirschsprung’s disease in male neonate. J Pediatr Surg 40:11–13. https://doi.org/10.1016/j.jpedsurg.2005.05.030
Jakchairoongruang K, Khakoo Y, Beckwith M (2018) Barkovich AJ (2018) New insight into neurocutaneous melanosis. Pediatr Radiol 48:1786–1796. https://doi.org/10.1007/s00247-018-4205-x
Johnson JM, Patten LL, Robson CD, Teele RL (2010) Ultrasonographic detection of intracranial melanocytosis in an infant. Pediatr Radiol 40:210–214. https://doi.org/10.1007/s00247-009-1402-7
Jozwiak S, Borkowska J (2008) Neurocutaneous melanosis. In: Ruggieri M, Pascual-Castroviejo I, Di Rocco C (eds) Neurocutaneous disorders. Phakomatoses and hamartoneoplastic syndromes. Springer, Wien/New York, pp 1–17
Kadonaga N, Frieden J (1991) Neurocutaneous melanosis. Definition and review of the literature. J Am Acad Dermatol 24:747–755. https://doi.org/10.1016/0190-9622(91)70115-i
Kadonaga JN, Barkovich AJ, Edwards MS, Frieden IJ (1992) Neurocutaneous melanosis in association with the Dandy–Walker complex. Pediatr Dermatol 9:37–43. https://doi.org/10.1111/j.1525-1470.1992.tb00323.x
Kalayci M, Cağavi F, Bayar U, Gül S, Dursun A, Ermis B, Açikgöz B (2006) Neurocutaneous melanosis associated with Dandy–Walker malformation. Acta Neurochir 148:1103–1106. https://doi.org/10.1007/s00701-006-0739-z
Kang SG, Yoo DS, Cho KS, Kim DS, Chang ED, Huh PW, Kim MC (2006) Coexisting intracranial meningeal melanocytoma, dermoid tumor, and Dandy-Walker cyst in a patient with neurocutaneous melanosis. Case report J Neurosurg 104:444–447. https://doi.org/10.3171/jns.2006.104.3.444
Kasantikul V, Shuangshoti S, Pattanaruenglai A, Kaorophtan M (1989) Intraspinal melanotic arachnoid cyst and lipoma in neurocutaneous melanosis. Surg Neurol 31:138–141. https://doi.org/10.1016/0090-3019(89)90328-5
Kim YJ, Won YD, Kim KT, Chang ED, Huh PW (2006) Parenchymal neurocutaneous melanosis in association with intraventricular dermoid and Dandy-Walker variant: a case report. Korean J Radiol 7:145–148. https://doi.org/10.3348/kjr.2006.7.2.145
Kimura H, Itoyama Y, Fujioka S, Ushing Y (1997) Neurocutaneous melanosis with intracranial malignant melanoma in an adult: a case report. No Shinkei Geka 25:819–822
Kinsler VA, Thomas AC, Ishida M, Bulstrode NW, Loughlin S, Hing S, Chalker J, McKenzie K, Abu-Amero S, Slater O, Chanudet E, Palmer R, Morrogh D, Stanier P, Healy E, Sebire NJ, Moore GE (2013) Multiple congenital melanocytic nevi and neurocutaneous melanosis are caused by postzygotic mutations in codon 61 of NRAS. J Invest Dermatol 133:2229–2236. https://doi.org/10.1038/jid.2013.70
Kinsler VA, O'Hare P, Bulstrode N, Calonje JE, Chong WK, Hargrave D, Jacques T, Lomas D, Sebire NJ, Slater O (2017) Melanoma in congenital melanocytic naevi. Br J Dermatol 176:1131–1143. https://doi.org/10.1111/bjd.15301
Kiratli H, Sahin A (2004) Fundus features of a case of neurocutaneous melanosis. Ophthalmic Genet 25:271–276. https://doi.org/10.1080/13816810490498206
Kittler NW, Mathes EF, Kinsler V, Frieden IJ (2019) The biker-glove pattern of congenital melanocytic nevi. Pediatr Dermatol 36:918–921. https://doi.org/10.1111/pde.13939
Ko SF, Wang HS, Lui TN, Ng SH, Ho YS, Tsai CC (1993) Neurocutaneous melanosis associated with inferior vermian hypoplasia: MR Findings. J Comput Assist Tomogr 17:691–695. https://doi.org/10.1097/00004728-199309000-00004
Koksal N, Bayram Y, Murat I, Murat D, Bostan O, Sevinir B, Yazici Z (2003) Neurocutaneous melanosis with transposition of the great arteries and renal agenesis. Pediatr Dermatol 20:332–334. https://doi.org/10.1046/j.1525-1470.2003.20412.x
Kudel TA, Bingham WT, Tubman DE (1979) Computed tomographic findings of primary malignant leptomeningeal melanoma in neurocutaneous melanosis. Am J Radiol 133:950–951
Kushimoto T, Basrur V, Valencia J, Matsunaga J, Vieira WD, Ferrans VJ, Muller J, Appella E, Hearing VJ (2001) A model for melanosome biogenesis based on the purification and analysis of early melanosomes. Proc Nat Acad Sci U S A 98:10698–10703. https://doi.org/10.1073/pnas.191184798
LaChance A, Shahriari M, Kerr PE, Grant-Kels JM (2016) Melanoma: kids are not just little people. Clin Dermatol 34:742–748. https://doi.org/10.1016/j.clindermatol.2016.07.009
Laennec RTH (1806) Sur les melanoses. Bulletin de la Faculte de Me ́decine de Paris 1:24–26
Laennec RTH (1812) Extrait du memoire de M Laennec, sur les mélanoses. Bull Ec Soc Med 24
Lamas E, Diez Lobato R, Sotelo T, Ricoy JR, Castro S (1977) Neurocutaneous melanosis Report of a case and review of the literature. Acta Neurochir (Wien) 36:93–05. https://doi.org/10.1007/BF01405990
Leany BJ, Rowe PW, Klug GL (1985) Neurocutaneous melanosis with hydrocephalus and syringomyelia (case report). J Neurosurg 62:148–152
Levy R, Lara-Corrales I (2016) Melanocytic nevi in children: a review. Pediatr Ann 45:e293–e298. https://doi.org/10.3928/19382359-20160720-07
Limas C, Tio FO (1972) Meningeal melanocytoma (“melanotic meningioma”). Its melanocytic origin as revealed by electron microscopy. Cancer 30:1286–1294. https://doi.org/10.1002/1097-0142(197211)30:5<1286::aid-cncr2820300522>3.0.co;2-v
Livingstone E, Claviez A, Spengler D et al (2009) Neurocutaneous melanosis: a fatal disease in early childhood. J Clin Oncol 27:2290–2291
Lovett A, Maari C, Decarie JC, Mracoux D, McCulag C, Hatami A, Savard P, Powell J (2009) Large congenital melanocytic nevi and neurocutaneous melanocytosis: one pediatric center’s experience. J Am Acad Dermatol 61:766–774. https://doi.org/10.1016/j.jaad.2008.11.022
Ma T, Fan K, Li L, Xie F, Li H, Chou H, Zhang Z (2017) Tissue expansion in the treatment of giant congenital melanocytic nevi of the upper extremity. Medicine (Baltimore) 96:e6358. https://doi.org/10.1097/MD.0000000000006358
MacLachlan WWG (1914) Extensive pigmentation of the brain associated with nevi pigmentosi of the skin. J Med Res 29:433–447
Makin GW, Eden OB, Lashford LS, Moppett J, Gerrard MP, Davies HA, Powell CV, Campbell AN, Frances H (1999) Leptomeningeal melanoma in childhood. Cancer 86:878–886
Makkar HS, Frieden IJ (2002) Congenital melanocytic nevi: an update for the pediatrician. Curr Opin Pediatr 14:397–403. https://doi.org/10.1097/00008480-200208000-00007
Makkar HS, Frieden IJ (2004) Neurocutaneous melanosis. Semin Cutan Med Surg 23:138–144. https://doi.org/10.1016/j.sder.2004.01.007
Marghoob AA, Dusza S, Oliveria S, Halpern AC (2004) Number of satellite nevi as a correlate for neurocutaneous melanocytosis in patients with large congenital melanocytic nevi. Arch Dermatol 140:171–175. https://doi.org/10.1001/archderm.140.2.171
Marnet D, Vinchon M, Mostofi K, Catteau B, Kerdraon O, Dhellemmes P (2009) Neurocutaneous melanosis and the Dandy. Walker complex: an uncommon but not so insignificant association. Childs Nerv Syst 25:1533–1539. https://doi.org/10.1007/s00381-009-0976-6
Martins da Silva VP, Marghoob A, Pigem R, Carrera C, Aguilera P, Puig-Butillé JA, Puig S, Malvehy J (2017) Patterns of distribution of giant congenital melanocytic nevi (GCMN): the 6B rule. J Am Acad Dermatol 76:689–694. https://doi.org/10.1016/j.jaad.2016.05.042
Martins da Silva V, Martinez-Barrios E, Tell-Martí G, Dabad M, Carrera C, Aguilera P, Brualla D, Esteve-Codina A, Vicente A, Puig S, Puig-Butillé JA, Malvehy J (2019) Genetic abnormalities in large to giant congenital nevi: beyond NRAS mutations. J Invest Dermatol 139:900–908. https://doi.org/10.1016/j.jid.2018.07.045
Mateos Gonzalez ME, Nieto del Rincon N, Torres Valdivieso MJ, López-Laso E, López Pérez J, Hde las Heras Simón R, Muñoz MJ, Onsurbe Ramírez I, Lillo Lillo M (2000) Neurocutaneous melanosis. An Esp Pediatr 52:573–576
McClelland S 3rd, Charnas LR, SantaCruz KS, Garner HP, Lam CH (2007) Progressive brainstem compression in an infant with neurocutaneous melanosis and Dandy-Walker complex fol- lowing ventriculoperitoneal shunt placement for hydrocephalus. J Neurosurg 107:500–503. https://doi.org/10.3171/PED-07/12/500
Mena-Cedillos CA, Valencia-Herrera AM, Arroyo-Pineda AI, Angeles Salgado-Jiménez M, Espinoza-Montero R, Martínez-Avalos AB, Perales-Arroyo A (2002) Neurocutaneous melanosis in association with the Dandy-Walker complex, complicated by melanoma: report of a case and literature review. Pediatr Dermatol 19:237–242. https://doi.org/10.1046/j.1525-1470.2002.00073.x
Merkel EA, Mohan LS, Shi K, Panah E, Zhang B, Gerami P (2019) Paediatric melanoma: clinical update, genetic basis, and advances in diagnosis. Lancet Child Adolesc Health 3:646–654. https://doi.org/10.1016/S2352-4642(19)30116-6
Miller VS (2004) Neurocutaneous melanosis. In: Miller VS, Roach ES (eds) Neurocutaneous syndromes. Cambridge University Press, Cambridge, pp 112–127
Mimouni F, Han BK, Barnes L, Ballard JL, Dignan PS, Kiessling MA, Lucky AW (1986) Multiple hamartomas associated with intracranial malformation. Pediatr Dermatol 3:219–225. https://doi.org/10.1111/j.1525-1470.1986.tb00517.x
Mir A, Agim NG, Kane AA, Josephs SC, Park JY, Ludwig K (2019) Giant congenital melanocytic nevus treated with trametinib. Pediatrics 143:e20182469. https://doi.org/10.1542/peds.2018-2469
Miranda P, Esparza J, Hinojosa J, Munoz A (2005) Neurocutaneous melanosis and congenital melanocytic nevus in the head. Pediatr Neurosurg 41:109–111
Mohinke O (1859) Ueber Pigment in der Arachnoidea spinalis. Virchows Arch F Path Anat 16:1179
Mutti LA, Mascarenhas MRM, Paiva JMG, Golcman R, Enokihara MY, Golcman B (2017) Giant congenital melanocytic nevi: 40 years of experience with the serial excision technique. An Bras Dermatol 92:256–259. https://doi.org/10.1590/abd1806-4841.20174885
Narayanan HS, Gandhi DH, Girimaji SR (1987) Neurocutaneous melanosis associated with Dandy-Walker syndrome. Clin Neurol Neurosurg 89:197–200
Norman MG, Ludwin SK (1991) Congenital malformations of the nervous system. In: Davis RL, Robertson DM (eds) Textbook of neuropathology, 2nd edn. Williams & Wilkins, Baltimore, pp 272–273
Noronha C, Rocha L (2019) Meningeal melanocytosis: a challenging diagnosis. Lancet Oncol 20:e343. https://doi.org/10.1016/S1470-2045(19)30298-0
Oberndorfer S (1903) Hydrocephalus congenitus (5 Liter Inhalt); Pigment naevi; Endotheliom des Kleinhirns. Mu€nch Med Wochenschr 50:1235
Oberndorfer S (1908) Pigment und Pigmentbildung. In: Lubarsch-Ostertag (Ed.), Ergebnisse der allgemeinen Pathologie. Vol. 12. Heft I, 77.
Ollivier d’Angers CP (1824) De la moelle épiniere et de ses maladies (Treatise on the Spinal Marrow and its Diseases). Crevot, Paris
Omar AT 2nd, Bagnas MAC, Del Rosario-Blasco KAR, Diestro JDB, Khu KJO (2018) Shunt surgery for neurocutaneous melanosis with hydrocephalus: case report and review of the literature. World Neurosurg 120:583–589.e3. https://doi.org/10.1016/j.wneu.2018.09.002
OMIM TM (2020) Oline Mendelian Inheritance in Man. An Online Catalogue of Human Genes and Genetic Disorders. Available at: https://omim.org
ORPHANET TM (2020) The Portal for rare diseases and orphan drugs. Available at: https://www.orpha.net/consor/cgi-bin/index.php
Padilla-Vázquez F, Escobar-de la Garma VH, Ayala-Arcipreste A, Mendizábal-Guerra R, Cuesta-Mejía T (2017) Melanocytoma and meningeal melanocytosis, similar but different lesions. Cir Cir 85:273–278. https://doi.org/10.1016/j.circir.2016.11.006
Pant K, Chawla R, Bhatia A, Jaggi OP, Raghu M, Goyal R (1988) Neurocutaneous melanosis with interstitial lung involvement--a rare association. Indian J Chest Dis Allied Sci 30:46–50
Paprocka J, Jamroz E, Kajor M, Marszał E (2004) Neurocutaneous melanosis – case report. Wiad Lek 57:520–523
Pascual-Castroviejo I (1983) Melanoblastosis neurocutanea de Touraine. In: Pascual-Castroviejo I (ed) Neurologıa infantil, I edn. Editorial Cientıfico Medica, Barcelona, pp 681–682
Pascual-Castroviejo I (1987) Neurocutaneous melanosis. In: Gomez M (ed) Neurocutaneous diseases. Butterworth, Boston, pp 329–334
Pavlidou E, Hagel C, Papavasilliou A, Giouroukos S, Panteliadis C (2008) Neurocutaneous melanosis: report of three cases and up-to-date review. J Child Neurol 23:1382–1391. https://doi.org/10.1177/0883073808319069
Pavlova O, Fraitag S, Hohl D (2016) 5-Hydroxymethylcytosine expression in proliferative nodules arising within congenital nevi allows differentiation from malignant melanoma. J Invest Dermatol 136:2453–2461. https://doi.org/10.1016/j.jid.2016.07.015
Pavone P, Falsaperla R, Marino S, Ruggieri M, Praticò AD, Nardone B (2019) Giant melanocytic nevi and soft tissue undergrowth in the left leg: pathogenetic hypothesis. Pediatr Rep 11:8184. https://doi.org/10.4081/pr.2019.8184
Pawlikowski JS, Brock C, Chen SC, Al-Olabi L, Nixon C, McGregor F, Paine S, Chanudet E, Lambie W, Holmes WM, Mullin JM, Richmond A, Wu H, Blyth K, King A, Kinsler VA, Adams PD (2015) Acute inhibition of MEK suppresses congenital melanocytic nevus syndrome in a murine model driven by activated NRAS and Wnt signaling. J Invest Dermatol 135:2093–2101
Pellino G, Gencarelli J, Bertelli S, Russo A, Fiumana E, Faggioli R (2020) Epilepsy in isolated parenchymal neurocutaneous melanosis: a systematic review. Epilepsy Behav 107:107061. https://doi.org/10.1016/j.yebeh.2020.107061
Peretti-Viton P, Gorincour G, Feuillet L, Lambot K, Brunel H, Raybaud C, Pellissier JF, Ali Chérif A (2002) Neurocutaneous melanosis: radiological pathological correlation. Eur Radiol 12:1349–1353. https://doi.org/10.1007/s00330-001-1195-z
Peters R, Jansen G, Engelbrecht V (2000) Neurocutaneous melanosis with hydrocephalus, intraspinal arachnoid collections and syringomyelia: case report and literature review. Pediatr Radiol 30:284–288
Phadke PA, Rakheja D, Le LP, Selim MA, Kapur P, Davis A, Mihm MC Jr, Hoang MP (2011) Proliferative nodules arising within congenital melanocytic nevi: a histologic, immunohistochemical, and molecular analysis of 43 cases. Am J Surg Pathol 35:856–869. https://doi.org/10.1097/PAS.0b013e31821375ea
Price HN (2016) Congenital melanocytic nevi: update in genetics and management. Curr Opin Pediatr 28:476–482
Qian M, Ren H, Qu T, Lu Z, Zou Y, He J, Zhao Y, Chen L, Guan H (2018) Spectrum of clinical, neuroimaging, and cerebrospinal fluid features of adult neurocutaneous melanocytosis. Eur Neurol 80:1–6. https://doi.org/10.1159/000488687
Ramaswamy V, Delaney H, Haque S, Marghoob A, Khakoo Y (2012) Spectrum of central nervous system abnormalities in neurocutaneous melanocytosis. Dev Med Child Neurol 54:563–568. https://doi.org/10.1111/j.1469-8749.2012.04275.x
Recio A, Sánchez-Moya AI, Félix V, Campos Y (2017) Congenital melanocytic nevus syndrome: a case series. Actas Dermosifiliogr 108:e57–e62. https://doi.org/10.1016/j.ad.2016.07.025
Reed WB, Becker SW Sr, Becker SW Jr, Nickel WR (1965) Giant pigmented nevi, melanoma, and leptomeningeal melanocytosis. Arch Dermatol 91:100–119. https://doi.org/10.1001/archderm.1965.01600080008002
Rhodes RE, Friedman HS, Hatten HP, Hockenberger B, Oakes WJ, Tomita T (1991) Contrast-enhanced MR imaging of neurocutaneous melanosis. AJNR Am J Neuroradiol 12:380–382
Roca de Vinals R, Elizalde Armendariz C, Coma-Fabres (1954) Tumores melanicos del SNC. A propo ́sito de tres casos cl ́ınicos. Med Clin (Barcelona) 22:304–311
Rokitansky J (1861) Ein ausgezeineter Fall von Pigment-Mal mit ausgebreiteter Pigmentirung der inneren Hirn und Ru€ckenmarksha ̈ute. Allg Wien Med Ztg 6:113–116
Ruan Y, Kovalchuk A, Jayanthan A, Lun X, Nagashima Y, Kovalchuk O, Wright JR Jr, Pinto A, Kirton A, Anderson R, Narendran A (2015) Druggable targets in pediatric neurocutaneous melanocytosis: molecular and drug sensitivity studies in xenograft and ex vivo tumor cell culture to identify agents for therapy. Neuro-Oncology 17:822–831. https://doi.org/10.1093/neuonc/nou310
Rufo Campos M, Castro Mendez E, Ruiz del Portal L (1998) Neurocutaneous melanosis and Dandy Walker syndrome. [Spanish]. An Esp Pediatr 48:318–320
Ruggieri M (2000) Cutis tricolor: congenital hyper- and hypopigmented lesions in a background of normal skin with and without associated systemic features: further expansion of the phenotype. Eur J Pediatr 159:745–749. https://doi.org/10.1007/pl00008339
Ruggieri M, Huson SM (1999) The neurofibromatoses. An overview. Ital J Neurol Sci 20:89–108. https://doi.org/10.1007/s100720050017
Ruggieri M, Polizzi A (2000) Segmental neurofibromatosis. J Neurosurg 93:530–532. https://doi.org/10.3171/jns.2000.93.3.0530
Ruggieri M, Praticò AD (2015) Mosaic neurocutaneous disorders and their causes. Semin Pediatr Neurol 22:207–233. https://doi.org/10.1016/j.spen.2015.11.001
Ruggieri M, Pavone V, De Luca D, Franzò A, Tiné A, Pavone L (1999) Congenital bone malformations in patients with neurofibromatosis type 1 (Nf1). J Pediatr Orthop 19:301–305
Ruggieri M, Pavone P, Polizzi A, Di Pietro M, Scuderi A, Gabriele A, Spalice A, Iannetti P (2004) Ophthalmological manifestations in segmental (localised) neurofibromatosis type 1 (NF1). Br J Ophthalmol 88:1429–1433. https://doi.org/10.1136/bjo.2004.043802
Ruggieri M, Gabriele AL, Polizzi A, Salpietro V, Nicita F, Pavone P, Platania N, Milone P, Distefano A, Privitera G, Belfiore G, Granata F, Caltabiano R, Albanese V, Pavone L, Quattrone A (2013) Natural history of neurofibromatosis type 2 with onset before the age of 1 year. Neurogenetics 14:89–98. https://doi.org/10.1007/s10048-013-0354-0
Ruggieri M, Polizzi A, Spalice A, Salpietro V, Caltabiano R, D’Orazi V, Pavone P, Pirrone C, Magro G, Platania N, Cavallaro S, Muglia M, Nicita F (2015) The natural history of spinal neurofibromatosis: a critical review of clinical and genetic features. Clin Genet 87:401–410. https://doi.org/10.1111/cge.12498
Ruggieri M, Micali G, Praticò AD (2018) Rare neurocutaneous disorders: state of the art and update. J Pediatr Neurol 16:253.378
Ruggieri M, Praticò AD, Caltabiano R, Polizzi A (2018) Early history of the differebnt forms of neurofibromatosis from the ancient Egypt to the British empire and beyond: first descriptions, medical curisioties, misconceptions, landmarks and the persons behind the syndromes. Am J Med Genet A 176:515–550. https://doi.org/10.1002/ajmg.a.38486
Ruggieri M, Praticò AD, Lacarrubba F, Micali G, Schepis C, Polizzi A (2018c) Archetypical patterns of skin manifestations in neurocutaneous disorders. J Pediatr Neurol 16:255–264
Ruiz-Maldonado R (2004) Measuring congenital melanocytic nevi. Pediatr Dermatol 21:178–179. https://doi.org/10.1111/j.0736-8046.2004.21222.x
Ruiz-Maldonado R, Tamayo L, Laterza AM, Durán C (1992) Giant pigmented nevi: clinical, histopathologic, and therapeutic considerations. J Pediatr 120:906–911. https://doi.org/10.1016/s0022-3476(05)81958-4
Ruiz-Maldonado R, del Rosario B-MM, Hidalgo-Galvan LR, Medina-Crespo V, Duràn-Mckinster C, Tamayo-Sánchez L, Mora-Tizcareño MA, Zuloaga A, de la Luz O-CM (1997) Giant congenital melanocytic nevi: neurocutaneous melanosis and neurological alterations. Dermatology 195:125–128. https://doi.org/10.1159/000245713
Salgado CM, Silver RB, Bauer BS, Basu D, Schmitt L, Khakoo Y, Reyes-Múgica M (2014) Skin of patients with large/giant congenital melanocytic nevi shows increased mast cells. Pediatr Dev Pathol 17:198–203. https://doi.org/10.2350/14-02-1444-OA.1
Salgado CM, Basu D, Nikiforova M, Hamilton RL, Gehris R, Jakacki R, Panigrahy A, Yatsenko S, Reyes-Múgica M (2015) Amplification of mutated NRAS leading to congenital melanoma in neurocutaneous melanocytosis. Melanoma Res 25:453–460. https://doi.org/10.3171/ped.2004.100.5.0501
Salisbury JR, Rose PE (1989) Primary central nervous malignant melanoma in the bathing trunk naevus syndrome. Postgrad Med J 65:387–389
Salpietro V, Polizzi A, Bertè LF, Chimenz R, Chirico V, Manti S, Ferraù V, Salpietro A, Arrigo T, Ruggieri M (2012) Idiopathic intracranial hypertension: a unifying neuroendocrine hypothesis through the adrenal-brain axis. Neuro Endocrinol Lett 33:569–573
Salpietro V, Polizzi A, Di Rosa G, Romeo AC, Dipasquale V, Morabito P, Chirico V, Arrigo T, Ruggieri M (2014) Adrenal disorders and the pediatric brain: pathophysiological considerations and clinical implications. https://www.scopus.com/record/display.uri?eid=2-s2.0-84931291890&origin=AuthorEval&zone=hIndex-DocumentListInt. J Endocrinol 2014:282489. https://doi.org/10.1155/2014/282489.
Sawicka E, Szczygielski O, Żak K, Pęczkowski P, Michalak E, Bekiesińska-Figatowska M (2015) Giant congenital melanocytic nevi: selected aspects of diagnostics and treatment. Med Sci Monit 21:123–132. https://doi.org/10.12659/MSM.891279
Schaffer JV, McNiff JM, Bolognia JL (2001) Cerebral mass due to neurocutaneous melanosis: eight years later. Pediatr Dermatol 18(5):369–377
Schreml S, Gruendobler B, Schreml J, Bayer M, Ladoyanni E, Prantl L, Eichelberg G (2008) Neurocutaneous melanosis in association with Dandy-Walker malformation: case report and literature review. Clin Exp Dermatol 33:611–614. https://doi.org/10.1111/j.1365-2230.2008.02745.x
Schwartz RA, Cohen-Addad N, Lambert MW, Lambert WC (1986) Congenital melanocytosis with myelomeningocele and hydrocephalus. Cutis 37:37–39
Shain AH, Yeh I, Kovalyshyn I, Sriharan A, Talevich E, Gagnon A, Dummer R, North J, Pincus L, Ruben B, Rickaby W, D'Arrigo C, Robson A, Bastian BC (2015) The Genetic evolution of melanoma from precursor lesions. N Engl J Med 373:1926–1936. https://doi.org/10.1056/NEJMoa1502583
Sharouf F, Zaben M, Lammie A, Leach P, Bhatti MI (2018) Neurocutaneous melanosis presenting with hydrocephalus and malignant transformation: case-based update. Childs Nerv Syst 34:1471–1477. https://doi.org/10.1007/s00381-018-3851-5
Shih F, Yip S, McDonald PJ, Chudley AE, Del Bigio MR (2014) Oncogenic codon 13 NRAS mutation in a primary mesenchymal brain neoplasm and nevus of a child with neurocutaneous melanosis. Acta Neuropathol Commun 2:140. https://doi.org/10.1186/s40478-014-0140-8
Shinno K, Nagashiro S, Uno M (2003) Neurocutaneous melano- sis associated with malignant leptomeningeal melanoma in an adult: clinical significance of 5-S-cysteinyldopa in the cerebrospinal fluid: case report. Neurol Med Chir (Tokyo) 43:619–625
Sievers J, von Knebel DC, Pehlemann FW et al (1986) Meningeal cells influence cerebellar development over a critical period. Anat Embryol 175:91–100
Simons EA, Huang JT, Schmidt B (2017) Congenital melanocytic nevi in young children: Histopathologic features and clinical outcomes. J Am Acad Dermatol 76:941–947. https://doi.org/10.1016/j.jaad.2016.12.026
Smith AB, Rushing EJ, Smirniotopoulos JG (2009) Pigmented lesions of the central nervous system: radiologic-pathologic correlation. Radiographics 29:1503–1524
Sobajima Y, Uchiyama T, Kudo H (1971) An autopsy case of melanose neuro-cutannee (Touraine). Acta Pathol Jpn 21:553–562
Stefanaki C, Chardalias L, Soura E, Katsarou A, Stratigos A (2017) Paediatric melanoma. J Eur Acad Dermatol Venereol 31:1604–1615. https://doi.org/10.1111/jdv.14299
Stefanaki C, Soura E, Stergiopoulou A, Kontochristopoulos G, Katsarou A, Potouridou I, Rigopoulos D, Antoniou C, Stratigos A (2018) Clinical and dermoscopic characteristics of congenital melanocytic naevi. J Eur Acad Dermatol Venereol 32:1674–1680
Subbiah V, Wolff JEA (2010) Rapid response to therapy of neurocutaneous melanosis with leptomeningeal melanoma. Pediatr Blood Cancer 54:180–181 (Letter)
Symmers W (1905) Pigmentation of the pia mater, with special reference to the brain of modern Egyptians. J Anat Physiol 40:25–27
Takahashi C, Ewen ME (2006) Genetic interaction between Rb and N-ras: differentiation control and metastasis. Cancer Res 66:9345–9348. https://doi.org/10.1158/0008-5472.CAN-06-1250
Takahashi C, Contreras B, Iwanaga T, Takegami Y, Bakker A, Bronson RT, Noda M, Loda M, Hunt JL, Ewen ME (2006) Nras loss induces metastatic conversion of Rb1-deficient neuroendocrine thyroid tumor. Nat Genet 38:118–123. https://doi.org/10.1038/ng1703
Toberer F, Happle R, Schneiderbauer R, Hausser I, Kröhl V, Epple A, Moog U, Enk AH, Lonsdorf AS (2017) At first sight or second glance: clinical presentation of mosaicmanifestations of autosomal dominant skin disorders - a case series. J Eur Acad Dermatol Venereol 31:1912–1915. https://doi.org/10.1111/jdv.14242
Touraine A (1941) La melanoblastose neuro-cutanee. La Presse Med 87–88:1087–1088
Touraine A (1949) Les me ́ lanoses neuro-cutane ́ es. Ann Dermatol Syphiligr (Paris) 9:489–524
Van Bogaert ML (1948) La me ́ lanose neurocutane ́ e diffuse he ́re ́dofamiliale. Bull Acad R Med. Belg 6th series 13:397–427
Van Heuzen EP, Kaiser MC, Slegte RGM (1989) Neurocutaneous melanosis associated with intraspinal lipomas. Neuroradiology 31:349–351
van Houten AH, van Dijk MCRF, Schuttelaar MLA (2010) Proliferative nodules in a giant congenital melanocytic nevus: case report and review of the literature. J Cutan Pathol 37:764–776. https://doi.org/10.1111/j.1600-0560.2009.01431.x
Vergier B, Laharanne E, Prochazkova-Carlotti M, de la Fouchardière A, Merlio JP, Kadlub N, Avril MF, Bodemer C, Lacoste C, Boralevi F, Taieb A, Ezzedine K, Fraitag S (2016) Proliferative nodules vs melanoma arising in giant congenital melanocytic nevi during childhood. JAMA Dermatol 152:1147–1151. https://doi.org/10.1001/jamadermatol.2016.2667
Vezina G, Barkovich AJ (2019) Neurocutaneous disorders. In: Barkovich AJ, Raybaud C (eds) Pediatric neuroradiology, 6th edn. Wolters-Kluver, Phialdelphia, pp 633–702 ISBN: 9781496337207
Waelchli R, Aylett SE, Atherton D, Thompson DJ, Chong WK, Kinsler VA (2015) Classification of neurological abnormalities in children with congenital melanocytic naevus syndrome identifies magnetic resonance imaging as the best predictor of clinical outcome. Br J Dermatol 173:739–750. https://doi.org/10.1111/bjd.13898
Walbert T, Sloan AE, Cohen ML, Koubeissi MZ (2009) Symptomatic neurocutaneous melanosis and Dandy–Walker malformation in an adult. J Clin Oncol 27:2886–2887
Wieczorek V, Waldmann KD, Teweleit HD, Hoffmeyer O (1972) Melanophakomatosis of the melanoblastose neurocutanee Touraine type with reference to cytology of cerebrospinal fluid. [German]. Dtsch Gesundheitsw 27:987–991
Wieselthaler NA, van Toorn R, Wilmshurst JM (2002) Giant congenital melanocytic nevi in a patient with brain structural malformations and multiple lipomatosis. J Child Neurol 17:289–291
Wilcox JC (1939) Melanomatosis of the skin and central nervous system in infants. A congenital neurocutaneous syndrome. Am J Dis Child 57:391–400
Williams ML, Pennella R (1994) Melanoma, melanocytic nevi, and other melanoma risk factors in children. J Pediatr 124:833–845. https://doi.org/10.1016/s0022-3476(05)83168-3
Yakovlev PI, Guthrie RH (1931) Congenital ectodermoses (neurocutaneous syndromes) in epileptic patients. Bourneville tuberous sclerosis (epiloia). Arch Neurol Psychiatr 26:1145–1194
Yang C, Gru AA, Dehner LP (2019) Common and not so Common Melanocytic Lesions in Children and Adolescents. Pediatr Dev Pathol 21:252–270. https://doi.org/10.1177/1093526617751720
Ye BS, Cho YJ, Jang SH et al (2008) Neurocutaneous melanosis presenting as chronic partial epilepsy. J Clin Neurol 4:134–137
Yu Q, Wu M, Sheng L, Li Q, Xie F (2018) Therapeutic effects of targeting RAS-ERK signaling in giant congenital melanocytic nevi. Am J Transl Res 10:1184–1194
Zhang W, Miao J, Li Q, Liu R, Li Z (2008) Neurocutaneous melanosis in an adult patient with diffuse leptomeningeal melanosis and a rapidly deteriorating course: case report and review of the literature. Clin Neurol Neurosurg 110:609–613. https://doi.org/10.1016/j.clineuro.2008.02.022
Zinatizadeh MR, Momeni SA, Zarandi PK, Chalbatani GM, Dana H, Mirzaei HR, Akbari ME, Miri SR (2019) The Role and Function of Ras-association domain family in Cancer: A Review. Genes Dis 6:378–384. https://doi.org/10.1016/j.gendis.2019.07.008
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruggieri, M., Polizzi, A., Catanzaro, S. et al. Neurocutaneous melanocytosis (melanosis). Childs Nerv Syst 36, 2571–2596 (2020). https://doi.org/10.1007/s00381-020-04770-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04770-9