Abstract
Purpose
For selected children with medically intractable epilepsy, hemispherectomy can be an excellent treatment option and its efficacy in achieving seizure freedom or reduction in seizure frequency has been shown in several studies, but patients’ selection could not be straightforward and often it is taken on subjective basis. We described a multimodal approach to assess patient eligible for hemispherectomy and possibly predicting post-surgical outcomes.
Methods
We describe pre- and post-surgical clinical features along with neuroradiological results by magnetic resonance imaging (MRI), functional magnetic resonance imaging (fMRI), MR-tractography (MRT), and neurophysiological study by single and paired pulses transcranial magnetic stimulation (TMS) in a child with cerebral palsy with epileptic encephalopathy, eligible for epilepsy surgery.
Results
Presurgical TMS evaluation showed a lateralization of motor function on the left motor cortex for both arms, and results were confirmed by MRI studies. Interestingly, after surgery, both epilepsy and motor performances improved and TMS showed enhancement of intracortical inhibition and facilitation activity.
Conclusion
Functional hemispherectomy is an effective treatment for drug-resistant epilepsy, and multimodal presurgical assessment may be a useful approach to guide surgeons in selecting patients. Moreover, pre- and post-surgical evaluation of these patients may enhance our understanding of brain plasticity phenomena.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Brain injury during gestation or early childhood that leads to atypical brain development may have deep and long-lasting effects on motor development, skill acquisition, and subsequent independence of a child. Cerebral palsy (CP) is the name for a group of permanent disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive lesions that occurred in the developing fetal or infant brain [1]. CP is a well-recognized neurodevelopmental condition beginning in early childhood; incidence of CP varies across countries, but current incidence is estimated 2.0–2.5 per 1000 live births in developed countries [2] with unilateral motor impairments evident in 30 to 40% of patients [3]. The motor disorders of CP [4] are often accompanied by disturbances of sensation, perception, cognition, communication, and behavior [5], and often, some of these patients develop medically intractable epilepsies [6]. For selected children with medically intractable epilepsy, hemispherectomy can be an excellent treatment option [7, 8] and its efficacy in achieving seizure freedom or reduction in seizure frequency has been shown in several studies [9, 10], but patients’ selection could not be straightforward and often it is taken on subjective basis. A major concern about hemispherectomy, in patients with residual motor function, is the risk of losing or worsening motor function and the prediction of post-operative functionality may be challenging [11].
Non-invasive neurophysiological tools such as transcranial magnetic stimulation (TMS) and neuroradiological techniques such as functional magnetic resonance imaging (fMRI) and MR-tractography (MRT) allowed in vivo exploration of the brain functional anatomy, facilitating the comprehension of neuronal recovery mechanisms [12], and they may have a role in predicting post-surgical neurological outcomes in the context of medically intractable epilepsy [13].
Interestingly, motor-evoked potential (MEP) changes have been found to be predictive of motor outcomes during the first days following a stroke or even in chronic stages [14, 15]. Nonetheless, the detailed relationship between corticospinal excitability measured by TMS and the potential for motor recovery remains unclear [13, 16, 17].
We describe clinical features along with neuroradiological and neurophysiological results in a child with CP and refractory epilepsy associated with epileptic encephalopathy [18], eligible for epilepsy surgery. We report pre- and post-surgical results of a multidisciplinary approach in a CP patient with refractory epilepsy eligible for hemispherectomy that allowed the forecasting of post-surgical results.
Case description
Patient was a 6-year-old female. Familial history was negative for seizures or other neurological diseases. Mother’s pregnancy was uneventful until 34th gestational week when prenatal ultrasounds scan showed a cerebral ventriculomegaly. Delivery was at 37.5 gestational weeks by cesarean section without perinatal distress. MRI performed 10 days after delivery showed changes compatible with previous Papile grade III germinative matrix hemorrhage in the right hemisphere, characterized by ventriculomegaly and late-stage periventricular leukomalacic tissue loss involving the posterior internal capsule, centrum semiovale, and thalamus (Fig. 1).
MRI examination obtained 10 days after delivery, showed findings compatible with previous Papile grade III germinal matrix hemorrhage and periventricular leukomalacia. Axial (A1) and coronal (A2) T2-weighted turbo-spin-eco images show dilated lateral ventricles and malacic changes of the right periventricular (arrowheads), posterior limb of internal capsule (PLIC), and thalamus (arrow). Post-hemorrhage hemosiderin deposition is demonstrated by T2*-weighted sequence (B) at the level of the thalamo-caudate groove (thin arrow), PLIC, and ventricle walls (arrowheads). Tiny methemoglobin deposits were also present at the level of the PLIC on T1-weighted (C) image (thin arrow)
During the first months of life, neurological examination revealed an asymmetry in spontaneous motility with best performances in the right side. Electroencephalography (EEG) study revealed a progressive increase of the paroxysmal activity with continuous spike-waves during slow sleep (CSWS), involving up to 85% of slow sleep (Fig. 2a, b). Despite antiepileptic multi-drug therapy, seizures and CSWS persisted and a progressive deterioration of cognitive functions and behavior was observed (Table 1). At the age of 6 years, neurological examination showed a mild left hemiparesis, left-hand mirror movements, with functional use of both hands, left hypoesthesia, homonymous hemianopia, and behavioral disorders such as disinhibition, emotional dependence, irritability, and attention deficit with dramatic effects on school and daily activities. Because of untreatable refractory epilepsy associated with epileptic encephalopathy, epilepsy surgery was taken into consideration.
A presurgical multimodal assessment was performed by an extensive neurological, neuroradiological, and neurophysiological assessment in order to demonstrate a possible ipsilateral motor function control of the left limbs that could prevent a motor deterioration after functional hemispherectomy.
Neurophysiological study
Neurophysiological study was performed 6 months before and 6 months after surgery using standard TMS protocols by single and paired pulses as previously described [13, 14], and the scalp was mapped systematically to explore the cortical representation of both FDI muscles, using a standard protocol [19, 20].
Stimulation points eliciting contra- or ipsilateral motor evoked potentials were searched in both hemispheres. To investigate the presence of contralateral and ipsilateral responses, we stimulated the optimal scalp position in the affected and unaffected hemisphere using a figure-of-eight coil at stimulus intensity of 100% of maximum stimulator output (MSO) during tonic activation at about 20% of maximum voluntary contraction (MVC) and at rest. We evaluated contralateral resting motor threshold (cRMT), contralateral active motor threshold (cAMT), ipsilateral short-latency intracortical inhibition (iSICI), contralateral short-latency intracortical inhibition (cSICI), ipsilateral intracortical facilitation (iICF), and contralateral intracortical facilitation (cICF). Also, ipsilateral cortical silent periods (iCSPs) and contralateral cortical silent periods (cCSPs) were recorded. Intracortical inhibition and facilitation was studied using the protocol of Kujirai et al. [21]. Facilitatory interstimulus intervals of 10, 15, and 25 ms were studied [22]. Amplitude of the conditioned MEPs was expressed as percentage of the amplitude of the test MEPs. To evaluate CSP, five stimuli at an intensity of 150% RMT were delivered.
Neuroradiological study
A presurgical multimodal structural, functional, and microstructural evaluation of the sensori-motor cortical areas and pathways was performed by using MRI. Data were acquired on a 1.5-T scanner (Philips Medical Systems, Best, The Netherlands) equipped with 8-channel head coil, during deep sedation using Propofol. Structural images consisted of a magnetization-prepared-rapid-acquisition-gradient-echo (MPRAGE) T1-weighted sequence (matrix 256 × 256, FOV 256 mm, slice thickness 1 mm, in-plane voxel size 1 mm × 1 mm, flip angle 12°, TR = 9.7 ms and TE = 4 ms).
The microstructural cortico-spinal tracts assessment was performed using diffusion tensor imaging (DTI) echo-planar spin-echo sequences with the following parameters: (TR/TE = 13,200/63 ms, slice thickness = 2 mm with no gap; 32 diffusion-sensitive non-colinear gradient directions). Data was preprocessed by using FDT, part of FSL software library (version 4.1-http://www.fmrib.ox.ac.uk/fsl) [23], by correcting for movement and eddy current. Then, by using DTK and TrackVis version 0.5.2 (http://trackvis.org), parametric FA maps of the brain fractional anisotropy were calculated, and the average FA values within regions of interest (ROIs) placed at the level of the posterior limb of the internal capsule (PLIC) were calculated in order to obtain an estimate of the cortico-spinal tracts microstructural integrity. Finally, deterministic tractography of the cortico-spinal tracts was performed for each side, by placing seeds on the FA direction-encoded color map at the level of the cerebral peduncle and the posterior limb of the internal capsule. A FA value of 0.18 with a maximum tensor reconstruction angle of 45 degrees threshold were used for tensor trajectory reconstruction. Localization of the cortical regions for sensorimotor functions was achieved by acquiring blood-oxygen-level-dependent (BOLD) fMRI examinations performed during (1) passive hands motor movements (fingers flexion) and (2) hands tactile brush stimulation [24]. The echo-planar BOLD T2* images parameters were TR = 2000 ms, TE = 60 ms, matrix size 64 × 64, FOV 256 mm, in-plane voxel size 4 mm × 4 mm, flip angle 90°, slice thickness 4 mm, and no gap. Four task (30s each) and five rest periods (20s each) block-paradigms were used for each passive motor and tactile examination, separately for the left and right hand. fMRI data analysis was performed with Brain Voyager QX version 1.10.4 (Brain Innovation, Maastricht, The Netherlands). After movement and slice timing correction, images were co-registered with the corresponding anatomical scans and smoothed using an isotropic Gaussian kernel (4-mm FWHM). The general linear model (GLM) was used to detect clusters with significant correlation between the BOLD signal and functional paradigms course, for each volume cluster.
Surgery
The young girl underwent a right peri-insular hemispherectomy at the age of 6 years. The operation was carried out under general anesthesia with the patient lying in supine position and left tilting of the head. The position of the ventricular cavities was assessed by intraoperative ultrasounds. A further confirmation of the position of the anatomical landmarks during the main surgical steps was obtained by intraoperative neuro-navigation (although the neural structures showed a grossly normal anatomy and were well recognizable). Accordingly, a small cortical incision was performed in the suprasylvian region (frontal lobe) to enter the body of the right lateral ventricle under magnification. The callosotomy, the section of the fibers of the corona radiata, and the commissurotomy were carried out from inside the lateral ventricle to disconnect the frontal, posterior temporal and parieto-occipital lobes. A second small corticectomy was realized at level of the temporal lobe (between T1 and T2) to enter the temporal horn of the right lateral ventricle (Fig. 3). This approach was used to disconnect the remaining temporal lobe and to perform the amigdalo-hippocampectomy.
Post-operative MRI follow-up demonstrates surgical right peri-insular functional disconnection changes. Asterisks in (a)–(c) indicate peri-insular dissection with superior and middle temporal gyri resection. Arrow in (a) shows internal capsule transection until the ventricular atrium. See main text for more details regarding the surgical procedure
Results
Post-operative clinical assessment
Few days after surgery, a full control of seizures with an immediate disappearance of CSWS was observed, without motor function worsening (Fig. 2c, d). Four months after surgery, Melbourne assessment showed an improvement of upper limb function (total score 72%), especially in finger dexterity, pronation/supination, and grasping and a progressive and significant improvement of cognitive functions was observed (Table 1).
Neurophysiological study
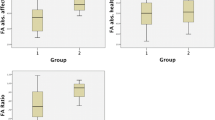
Stimulation at 100% of MSO of right motor cortex was not able to evoke MEPs from left and right FDI muscles even at intensity of 100% MSO at rest and during MVC. On the other hand, after single pulse at 100% MSO of left motor cortex, MEPs were recorded on both FDI. After, a single-pulse TMS on left motor cortex MEPs elicited and recorded from both FDI muscles had a similar latency (cMEPs: 20.5 vs. iMEPs: 21.2 ms). Neurophysiological results are shown in Fig. 4.
Histograms show pre- and post-surgical neurophysiological examination by single and paired TMS of left motor cortex and recordings from both sides. Contralateral SICI (cSICI) and ipsilateral ICF (iICF) were increased after surgery. Both contra- and ipsilateral Cortical Silent Periods (cCSP and iCSP) were reduced after surgery. *p < 0.05, level of significance
Neuroradiological findings
MRI examination showed findings compatible with previous Papile grade III germinal matrix hemorrhage and periventricular leukomalacia (Fig. 5A1 and A2).
Multimodal MRI assessment of patient’s sensori-motor structural damage and functional reorganization. Axial T1-MPRAGE images (A1 and A2) show malacic changes of the right periventricular white matter, extensively involving the pre- and post-central giri (arrowheads in A1), as well as the posterior thalamus and PLIC (empty arrow in A2). At the microstructural DTI analysis, there is poor visualization of the right CST fibers (B1, arrow on the FA color map at the level of the pons) with respect to the contralateral unaffected side (same image, empty arrow). The tractography reconstruction of the CSTs (B2) demonstrates clear asymmetry due to reduced number and length of the right CST (red tract) with respect to the left (blue tract). The functional assessment results (p < 0.05, Bonferroni-corrected) overlaid on the anatomical MPRAGE images (C). The left central sulcus is indicated by dashed lines. The right hand passive motor and sensory tasks elicited significant activations in the left pre- and post-central gyri, respectively. The left-hand passive motor task elicited activations ipsilaterally at the level of the left precentral gyrus, while no significant activations were found for the sensory task. Importantly, no significant activations were detected in the right hemisphere by any task. Images are presented in radiological convention
At the microstructural analysis, the average fractional anisotropy (FA) value at the level of the right (affected hemisphere) posterior limb of the internal capsule (PLIC) was lower (0.40) than the contralateral (0.62), indicating abnormal fibers organization/integrity. Consistently, the right corticospinal tract (CST) representation on the color-encoded FA maps was reduced as compared with the normal side (Fig. 5 (B1)). The CST tractography analysis demonstrated a clear asymmetry characterized by severely reduced representation of the reconstructed right fibers, which failed to reach the sensori-motor cortex (Fig. 5 (B2)).
At the functional examinations, both the right- and paretic left-hand passive motor tasks elicited statistically significant activations in the left precentral gyrus cortex only, at slightly different locations (Fig. 5 (C)). As expected, the sensitive tactile stimulation of the right hand elicited statistically significant activations in the left post-central cortex; however, no statistically significant activations were obtained for the paretic left hand. Remarkably, no significant activation was detected in the right (affected) hemisphere by any of the motor and/or sensory tasks. Altogether, the patient neuroradiological workup indicated severe structural and microstructural damage to the right sensory-motor pathways, with reorganization of the paretic left hand motor function in the ipsilateral hemisphere.
Discussion
In our case, the indication to hemispherectomy was the presence of drug-resistant epilepsy but surgical decision was challenging because of a good functional residual motor activity of the affected hand and because of a potential harmful effect on the residual functionality.
TMS revealed that right motor cortex stimulation did not evoke MEPs and along with DTI analyses demonstrated a severe damage of the right CST. On the other hand, presurgical evaluation revealed left motor cortex integrity and bilateral representation of hand motor functions on the left motor cortex. The passive motor fMRI study was able to localize the sensory-motor function of the left (paretic) hand in the ipsilateral hemisphere, and—most remarkably—revealed no activation on the more affected right hemisphere. Non-invasive presurgical studies suggested a bilateral control of motor function by the unaffected hemisphere due to both contra- and ipsilateral motor pathways, and it was confirmed by motor assessment on post-surgical evaluation.
Taken together, above findings suggest that plasticity changes after early extensive brain injury had occurred during subsequent development, and motor function of the left limbs had most likely been entirely reorganized in the ipsilateral hemisphere by preservation and reinforcement of ipsilateral descending fetal motor pathways [25]. On the other hand, a focal injury early in life, in an otherwise healthy brain represents an ideal model of human developmental motor plasticity and intracortical reorganization [26]. Neurophysiological measures seem to be useful biomarkers of brain plasticity during development [27] and may provide insights in brain plasticity process.
Presurgical TMS evaluation showed no response after affected hemisphere stimulation but showed bilateral activation after left hemisphere stimulation and because MR-tractography disclosed interruption of CSP on right hemisphere, preoperative work-up indicated the left motor cortex as the functioning cortex with bilateral representation. Moreover, neurophysiological evaluation before and after surgery revealed modification of intracortical connections. In particular, motor threshold and MEP latencies were unchanged while contralateral SICI and ipsilateral ICF were increased after hemispherectomy. After surgery, patient showed a better control of seizures. Because the level of SICI is related to the level of intracortical GABAA activity [28], its increase after surgery might explain the effects on seizure control. On the other hand, ICF origin is more complex and probably it may be influenced by multiple neurotransmitters systems [22]. Before surgery, patient showed an asymmetric hand motor impairment (right > left) and after surgery motor performances did not worsen but, interestingly, manual dexterity improved and this long-lasting effect may be explained by a plastic change of motor cortex [29]. It is conceivable that damaged hemisphere might exert a negative effect on the functional hemisphere. Early brain lesion causing maladaptive interhemispheric interaction due to interhemispheric rivalry and interhemispheric imbalance [30] may explain this effect. It is confirmed by positive effects of functional hemispherectomy on motor performances, and it is in accordance with previous studies involving non-invasive brain stimulation techniques [16]. Besides, improvements after functional hemispherectomy may suggest that stopping interhemispheric imbalance may be beneficial both on seizures control and motor control. Moreover, TMS evaluation demonstrated enhancement of cSICI and iICF that are effects of intracortical excitatory and inhibitory phenomena [22, 28], and these long-lasting effects, recorded 6 months after surgery, may be due to intracortical plasticity phenomena induced by functional hemispherectomy [13]. Several studies demonstrated that integrity of CST is crucial for motor recovery [31, 32]. In our patient, DTI analysis and 3D fiber-tracking demonstrated extensive loss of the right CST trajectories and FA reduction across the remaining pathways suggesting severe CST structural damage; this finding may explain the unresponsiveness of LFDI to right motor cortex stimulation by TMS. Moreover, several studies tried to find reliable prognostic biomarkers [31, 32], but conclusive results are lacking.
We are aware of the limit in drawing definite conclusions due to single case description and usefulness of this approach may be indicated only after a well-designed clinical study will address this point confirming conclusions, but we deem that above described paradigm, since involves non-invasive and techniques commonly used in clinical context, may be implemented in presurgical evaluation of patients eligible for epilepsy surgery.
Conclusion
Functional hemispherectomy is an effective treatment for drug-resistant epilepsy, but surgical outcome, in terms of residual motor functionality, may limit indications for this treatment.
Multimodal presurgical assessment, by neuroradiological and neurophysiological evaluation using fMRI, DTI, and structural MRI along with TMS may help surgeons in selecting patients for functional hemispherectomy in order to avoid or reduce the risk of post-surgical motor impairment or worsening, even if its usefulness in forecasting post-surgical motor functionality should be proven in a wide clinical trial.
References
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B (2007) A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol 49:8–14. https://doi.org/10.1111/j.1469-8749.2007.tb12610.x
Blair E (2010) Epidemiology of the cerebral palsies. Orthop Clin North Am 41:441–455. https://doi.org/10.1016/j.ocl.2010.06.004
Bax M, Tydeman C, Flodmark O (2006) Clinical and MRI correlates of cerebral palsy: the European cerebral palsy study. JAMA 296:1602–1608. https://doi.org/10.1001/jama.296.13.1602
Riddell M, Kuo H-C, Zewdie E, Kirton A (2019) Mirror movements in children with unilateral cerebral palsy due to perinatal stroke: clinical correlates of plasticity reorganization. Dev Med Child Neurol. https://doi.org/10.1111/dmcn.14155
Rosenbaum P (2007) The natural history of gross motor development in children with cerebral palsy aged 1 to 15 years. Dev Med Child Neurol 49:724. https://doi.org/10.1111/j.1469-8749.2007.00724.x
Cross JH, Jayakar P, Nordli D, Delalande O, Duchowny M, Wieser HG, Guerrini R, Mathern GW, International League against Epilepsy, Subcommission for Paediatric Epilepsy Surgery, Commissions of Neurosurgery and Paediatrics (2006) Proposed criteria for referral and evaluation of children for epilepsy surgery: recommendations of the Subcommission for Pediatric Epilepsy Surgery. Epilepsia 47:952–959. https://doi.org/10.1111/j.1528-1167.2006.00569.x
Battaglia D, Veggiotti P, Lettori D, Tamburrini G, Tartaglione T, Graziano A, Veredice C, Sacco A, Chieffo D, Pecoraro A, Colosimo C, di Rocco C, Dravet Ch, Guzzetta F (2009) Functional hemispherectomy in children with epilepsy and CSWS due to unilateral early brain injury including thalamus: sudden recovery of CSWS. Epilepsy Res 87:290–298. https://doi.org/10.1016/j.eplepsyres.2009.09.014
Jadhav T, Cross JH (2012) Surgical approaches to treating epilepsy in children. Curr Treat Options Neurol 14:620–629. https://doi.org/10.1007/s11940-012-0203-8
Dwivedi R, Ramanujam B, Chandra PS, Sapra S, Gulati S, Kalaivani M, Garg A, Bal CS, Tripathi M, Dwivedi SN, Sagar R, Sarkar C, Tripathi M (2017) Surgery for drug-resistant epilepsy in children. N Engl J Med 377:1639–1647. https://doi.org/10.1056/NEJMoa1615335
Spencer S, Huh L (2008) Outcomes of epilepsy surgery in adults and children. Lancet Neurol 7:525–537. https://doi.org/10.1016/S1474-4422(08)70109-1
Zsoter A, Pieper T, Kudernatsch M, Staudt M (2012) Predicting hand function after hemispherotomy: TMS versus fMRI in hemispheric polymicrogyria. Epilepsia 53:e98–e101. https://doi.org/10.1111/j.1528-1167.2012.03452.x
Pilato F, Profice P, Ranieri F, Capone F, di Iorio R, Florio L, di Lazzaro V (2012) Synaptic plasticity in neurodegenerative diseases evaluated and modulated by in vivo neurophysiological techniques. Mol Neurobiol 46:563–571. https://doi.org/10.1007/s12035-012-8302-9
Pilato F, Dileone M, Capone F, Profice P, Caulo M, Battaglia D, Ranieri F, Oliviero A, Florio L, Graziano A, di Rocco C, Massimi L, di Lazzaro V (2009) Unaffected motor cortex remodeling after hemispherectomy in an epileptic cerebral palsy patient. A TMS and fMRI study. Epilepsy Res 85:243–251. https://doi.org/10.1016/j.eplepsyres.2009.03.016
Di Lazzaro V, Profice P, Pilato F et al (2012) The level of cortical afferent inhibition in acute stroke correlates with long-term functional recovery in humans. Stroke 43:250–252. https://doi.org/10.1161/STROKEAHA.111.631085
Di Lazzaro V, Profice P, Pilato F et al (2010) Motor cortex plasticity predicts recovery in acute stroke. Cereb Cortex N Y N 1991 20:1523–1528. https://doi.org/10.1093/cercor/bhp216
Di Pino G, Pellegrino G, Assenza G et al (2014) Modulation of brain plasticity in stroke: a novel model for neurorehabilitation. Nat Rev Neurol 10:597–608. https://doi.org/10.1038/nrneurol.2014.162
Stinear CM, Barber AP, Smale PR et al (2007) Functional potential in chronic stroke patients depends on corticospinal tract integrity. Brain 130:170–180. https://doi.org/10.1093/brain/awl333
Tassinari CA, Rubboli G (2019) Encephalopathy related to status epilepticus during slow sleep: current concepts and future directions. Epileptic Disord Int Epilepsy J Videotape 21:82–87. https://doi.org/10.1684/epd.2019.1062
Bourke-Taylor H (2003) Melbourne assessment of unilateral upper limb function: construct validity and correlation with the pediatric evaluation of disability inventory. Dev Med Child Neurol 45:92–96
Maegaki Y, Maeoka Y, Seki A et al (1997) Facilitation of ipsilateral motor pathways during recovery from hemiplegia in two adolescent patients. Eur J Paediatr Neurol EJPN Off J Eur Paediatr Neurol Soc 1:79–84
Kujirai T, Caramia MD, Rothwell JC, Day BL, Thompson PD, Ferbert A, Wroe S, Asselman P, Marsden CD (1993) Corticocortical inhibition in human motor cortex. J Physiol 471:501–519. https://doi.org/10.1113/jphysiol.1993.sp019912
Di Lazzaro V, Pilato F, Oliviero A et al (2006) Origin of facilitation of motor-evoked potentials after paired magnetic stimulation: direct recording of epidural activity in conscious humans. J Neurophysiol 96:1765–1771. https://doi.org/10.1152/jn.00360.2006
Smith SM (2004) Overview of fMRI analysis. Br J Radiol 77(2):S167–S175. https://doi.org/10.1259/bjr/33553595
Blatow M, Reinhardt J, Riffel K, Nennig E, Wengenroth M, Stippich C (2011) Clinical functional MRI of sensorimotor cortex using passive motor and sensory stimulation at 3 tesla. J Magn Reson Imaging JMRI 34:429–437. https://doi.org/10.1002/jmri.22629
Staudt M, Grodd W, Gerloff C et al (2002) Two types of ipsilateral reorganization in congenital hemiparesis: a TMS and fMRI study. Brain J Neurol 125:2222–2237
Kirton A (2013) Modeling developmental plasticity after perinatal stroke: defining central therapeutic targets in cerebral palsy. Pediatr Neurol 48:81–94. https://doi.org/10.1016/j.pediatrneurol.2012.08.001
Zewdie E, Damji O, Ciechanski P, Seeger T, Kirton A (2017) Contralesional corticomotor neurophysiology in hemiparetic children with perinatal stroke. Neurorehabil Neural Repair 31:261–271. https://doi.org/10.1177/1545968316680485
Di Lazzaro V, Pilato F, Dileone M et al (2006) GABAA receptor subtype specific enhancement of inhibition in human motor cortex. J Physiol 575:721–726. https://doi.org/10.1113/jphysiol.2006.114694
Eyre JA (2007) Corticospinal tract development and its plasticity after perinatal injury. Neurosci Biobehav Rev 31:1136–1149. https://doi.org/10.1016/j.neubiorev.2007.05.011
Grefkes C, Nowak DA, Eickhoff SB, Dafotakis M, Küst J, Karbe H, Fink GR (2008) Cortical connectivity after subcortical stroke assessed with functional magnetic resonance imaging. Ann Neurol 63:236–246. https://doi.org/10.1002/ana.21228
Puig J, Blasco G, Schlaug G, Stinear CM, Daunis-I-Estadella P, Biarnes C, Figueras J, Serena J, Hernández-Pérez M, Alberich-Bayarri A, Castellanos M, Liebeskind DS, Demchuk AM, Menon BK, Thomalla G, Nael K, Wintermark M, Pedraza S (2017) Diffusion tensor imaging as a prognostic biomarker for motor recovery and rehabilitation after stroke. Neuroradiology 59:343–351. https://doi.org/10.1007/s00234-017-1816-0
Puig J, Blasco G, Terceño M et al (2019) Predicting motor outcome in acute intracerebral hemorrhage. AJNR Am J Neuroradiol. https://doi.org/10.3174/ajnr.A6038
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pilato, F., Pravatà, E., Battaglia, D. et al. Multimodal assessment of motor pathways and intracortical connections in functional hemispherectomy. Childs Nerv Syst 36, 3085–3093 (2020). https://doi.org/10.1007/s00381-020-04617-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04617-3