Abstract
Purpose
Foetal ventriculomegaly (VM) is one of the most commonly diagnosed brain abnormalities. The aims of this study were to assess cases with isolated VM, describe the prenatal course and assess short- and long-term follow-up at the age of 2 years.
Methods
We performed a retrospective analysis from our prenatal data base and included all children that were prenatally diagnosed with VM in our unit between 2008 and 2013 (n = 250). Prenatal management, postnatal outcome and neurologic development at the age of 2 years were evaluated.
Results
A total of 106 children were born at our institution and were diagnosed prenatally with isolated borderline VM. A total of 1.9% (n = 2/106) was transferred to the neonatal unit. A total of 0.9% (n = 1/106) showed abnormal findings in postnatal brain ultrasound. A total of 1.9% (n = 2/106) showed mild neurologic abnormalities after birth, but none had to be seen by a neuropediatrician. At the follow-up at 2 years, 2.5% (n = 1/40) had an insertion of a shunt.
Conclusion
Based on our analysis, the majority of isolated borderline VM do not show short- or long-term neurological abnormalities. However, all cases of VM should be referred to a detailed prenatal ultrasound exam by a specialist.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ventriculomegaly (VM) is one of the most frequently diagnosed antenatal brain anomalies with a prevalence from 1.48 up to 22 per 1000 births [1, 2]. It is defined by a dilatation of the posterior foetal lateral ventricles and is commonly evaluated during the assessment of the foetal anatomy between 20 and 22 weeks of pregnancy. Even though there is no determined description of VM, the widely accepted definition is a dilatation of > 10 mm [1]. The leading reasons for a foetal VM are spina bifida, agenesis of the corpus callosum, Dandy-Walker malformation, stenosis of the aqueduct and Chiari II malformation [2]. Furthermore, it is associated with foetal infections, as well as with chromosomal and structural anomalies [3]. Severe VM is related with a poor prognosis [4, 5]. Moreover, a positive correlation was found between the degree of neurodevelopmental delay and the width of the lateral ventricles [6]. Some studies indicate that the prognosis mainly depends on the aetiology and the existence of associated anomalies [4, 7, 8]. If the foetus has no other abnormalities detected by prenatal ultrasound, the VM is generally considered as “isolated” ventriculomegly. The mortality rate is lower, prognosis is better and neurodevelopmental outcome is superior in isolated VM than in presence of associated malformations [6, 9, 10].
There are many foetuses diagnosed with an extension of the cerebral posterior lateral ventricle of 8–10 mm, which is often referred to as prominent or borderline VM. The significance of this finding, however, is not well known. Borderline VM can be interpreted as an abnormal finding and can be associated with chromosomal or structural cerebral anomalies or can just be interpreted as a powerless discovery without any pathological significance [11]. Counselling of the parents therefore is very challenging. The aim of this study was to assess cases with VM between 8 and 15 mm, with a main focus on cases with borderline VM between 8 and 10 mm that were isolated on prenatal ultrasound. We aimed to describe the prenatal course and management and assess short- and long-term development at the age of 2 years.
Methods
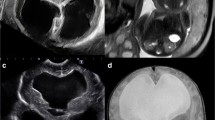
This is a 5-year retrospective, single-centre data analysis. The study was evaluated and approved by the local ethics committee (EKNZ 2015-447). We performed a Viewpoint data base search (GE healthcare, Version 5.6.22.30). According to local regulations, informed consent was not required for this retrospective study. All children were included, who were prenatally diagnosed by ultrasound with a ventriculomegaly (VM) at the University Hospital in Basel and were born between June 2008 and August 2013. The lateral ventricles were evaluated with an axial perspective on the foetal head, on the transventricular level, at the position of the glomus of the atrium and by measuring the ventricular cavity between the echoes produced by the lateral walls. The ultrasounds were conducted by experienced certified senior ultrasound specialists, with Voluson E8 and Voluson Expert, GE US machines. Borderline VM was defined as 8.0–10 mm, mild VM 10.1–12.0 mm, moderate VM 12.1–15.0 mm and severe VM from 15.1 mm. The prenatal management as well as data after birth was collected from the patient’s files. In the time period from June 2008 to August 2013, 159 children with apparently isolated borderline VM were included, from which the following information was collected: foetal MRI conducted (yes/no), a test for toxoplasmosis, rubella, cytomegalovirus and herpes simplex virus (TORCH)—testing (yes/no), progression of the VM during pregnancy (yes/no), delivery outcome and karyotyping (yes/no). A progression of the VM was defined as an increase of the ventricle width of ≥ 5 mm during the pregnancy and a regression was determined ≤ 5 mm.
From 159 children diagnosed with isolated borderline VM, 106 were born at our institution.
From all children born at our institution, we assessed the following parameters: week of pregnancy, birthweight, APGAR scores, sex, neurologic findings, transfer to the neonatal unit, postnatal cerebral ultrasound or MRI and neuropediatric consultation. In a second step, a questionnaire on the neurologic development at the age of 2 was sent out to the paediatricians in charge. The paediatrician was known in 84.9% (n = 90/106). Motor skills, cognitive behaviour, language development, social behaviour, growth charts and relevant neurologic interventions or diagnoses (cerebral palsy, shunt insertion) were evaluated.
Results
Two-hundred-fifty children with VM were included (Fig. 1). Among these, 78.8% (n = 197/250) had borderline VM.
Out of these, 19.3% (n = 38/197) showed associated anomalies and two of them (5.2%; n = 2/38) had chromosomal abnormalities (one case of trisomy 18 and one case of monosomy x).
A total of 159/197 (77.1%) were apparently isolated cases (Fig. 1). Outcome at delivery was available for 153 cases. A total of 11.1% (n = 17/153) underwent prenatal invasive diagnostic testing. All of these showed normal karyotypes. A total of 3.3% (n = 5/153) underwent a prenatal MRI confirming VM without additional findings, 15.7% (n = 24/153) had TORCH (Toxoplasmosis, rubella, cytomegalovirus, herpes simplex virus 2 and other infections) testing, 4.6% (n = 7/153) had a positive IgG and IgM for Borrelia (n = 3), HSV (n = 3) or Parvovirus B19 (n = 1) (Table 1). Two cases were diagnosed with trisomy 21 postpartum (1.3%; n = 2/153). Both of these children showed an increased risk in first trimester screening but the patient denied further testing and the foetuses showed no additional anomalies on follow-up ultrasound exams apart from borderline VM.
A total of 21.6% (n = 33/153) women presented for follow-up ultrasound exams during pregnancy. Of these, 33.3% (n = 11/33) had a progression of the VM. Actually, 12.1% (n = 4/33) developed mild VM. The lateral ventricles width decreased in 21.2% (n = 7/33) but all of the cases remained above 8 mm. In 45.4% (n = 15/33), the width of the lateral ventricles was stable (Fig. 2).
All but one of the 153 children with an isolated borderline VM were born alive. There was one early induction in 23 gestational weeks because of maternal complications (preeclampsia). A total of 20.9% (n = 32/153) had a premature delivery (< 37 weeks of pregnancy), from which 40.6% (n = 13/32) were twins and 12.5% (n = 4/32) had intrauterine growth restriction (IUGR).
Hundred-six children had a follow-up after delivery (Table 2). Sixty-nine percent (n = 74/106) were boys.
The median gestational week at delivery was 38 (27–41 weeks). Median birth weight was 3270 g (860–4660 g). The median APGAR after 1, 5 and 10 min was 8 (1–10), 9 (4–10) and 10 (6–10) respectively. 1.9% (n = 2/106) were transferred to the neonatal unit due to VM. A total of 21.7% (n = 23/106) had a postnatal brain ultrasound and one (0.9%) showed abnormal findings, i.e. haemorrhagic hydrocephalus after a delivery at 29 weeks.
A total of 2.8% (n = 3/106) had a postnatal MRI. A total of 1.9% (n = 2/106) showed mild neurologic abnormalities such as a reduced neonatal muscular tonus with the haemorrhagic hydrocephalus and another child showed a pseudo microcephaly most likely due to a forced intrauterine position. None of them was referred to or initially evaluated by a neuropediatric specialist.
Follow-up at 2 years was available for 40 children (Table 3). The questionnaire response rate was 44.4% (n = 40/90). A total of 27.5% (n = 11/40) had abnormal findings in the four categories of motoric skills, cognitive behaviour, language development and social behaviour. In our study, 15.0% (n = 6/40) of the children had slight motoric delays and 15% (n = 6/40) of them had social behavioural problems, such as, for example aggressions in nursery school. A total of 2.5% (n = 1/40) had cognitive behaviour difficulties such as attention deficit disorders and 20% (n = 8/40) of them had speaking troubles in form of delays.
Considering the height, 30.0% (n = 12/40) were above the 90 percentile and 5.0% (n = 2/40) were below the 10 percentile. Infant weight was above the 90 percentile in 30.0% (n = 12/40). A total of 27.5% (n = 11/40) had head circumferences above the 90 percentile and 5.0% (n = 2/40) had head circumferences under the 10 percentile. There was no case of cerebral palsy, but one child had an insertion of a shunt (2.5%). In the prenatal period, this child had no associated anomalies, the borderline VM increased, but stayed below 10 mm. After delivery at 29 weeks, it showed neurological abnormalities and had cerebral haemorrhage, most likely due to premature delivery. After 2 years, the child showed a retardation in language development.
A total of 7.5% (n = 3/40) of the children had other neurological diagnoses (familial megalocephalia and seizures with status post-meningitis) and 7.5% (n = 3/40) had additional different diagnoses (exotropia and hyperopia, recurrent bronchitis and recurrent otitis, supraventricular extra systoles with an atrioventricular block).
Discussion
This is a large retrospective population-based study of borderline VM over a 5-year period. Borderline VM was defined as a width of the lateral ventricles of 8.0–10.0 mm. Although the common definition of mild VM is considered from a width of 10 mm, we commonly have referrals with borderline cases below 10 mm. Data in the literature regarding this situation is scarce. We here present data on the progress of this type of VM during pregnancy, data directly after birth and unique long-term information on the outcome of the children at the age of 2 years.
A total of 250 children were diagnosed by prenatal ultrasound with VM during a 5-year period. Of these, 78.8% were identified with borderline VM. Almost one fifth of the children diagnosed with borderline VM had associated malformations and around 5% were diagnosed with chromosomal abnormalities. This is in line with data from recent meta-analyses on mild VM 10–12 mm which reported 4.7% abnormal karyotypes [12]. The rate of associated anomalies was higher at 33.5% [12] which would correlate with the findings that moderate VM has a significantly higher association with anomalies than mild VM [7, 8, 13]. Prenatal therapies have been described for the in utero-treatment of menigomyelocele and have shown that prenatal surgery can be of benefit for selected patients [14]. In utero-treatment for hypertensive-hydrocephalus by ventriculo-amniotic, shunting has been described in the literature with a benefit in selected cases, but the technique is challenging and prospective clinical trials are lacking [15]. From our data, we can support referral for a detailed prenatal ultrasound for ruling out other abnormalities and to find the cause of VM, which could have therapeutic consequences for selected foetuses.
Foetal infections such as TORCH may cause ventricular dilatation. Numerous studies demonstrate that a single manifestation of prenatal cytomegalovirus (CMV) infection may be a mild VM [16, 17].
In our study, 16% had TORCH testing, whereas 4.7% showed positive IgMs for different types of infections. There was no case of CMV infection. None of the mothers had clinical signs of infection and IgG or IgM levels did not increase on follow-up. So, most likely, these were not cases with an acute infection. In our study, TORCH testing leads to follow-up serologic exams and no proof of maternal infection. Our data does not support TORCH testing for cases of isolated borderline VM in the absence of clinical symptoms.
This is supported by other data recommending targeted CMV testing instead of TORCH screening [18, 19]. However, it might be discussed in individual cases in patients which are at risk for these infections or in foetuses with associated anomalies [18, 19].
Concerning singleton pregnancies with normal intrauterine growth, 10% of our cohort had a premature delivery, which is in line with data from the World Health Organisation (WHO) showing premature delivery rate of 9.0% in higher-income countries [20].
Prenatal MRI was not conducted in the majority of the cases as it was not used systematically. Depending on the study, the rate of newly discovered diagnoses through prenatal MRI is varying between 5 and 66% [19,20,21,22,23,24,25,26]. The increased amount of other findings after a specialist sonography, however, has been shown to be low and does not recommended MRI as a standard [25,26,27,28,29].
Of the women presenting for follow-up exams, 21.1% had an increase of the width of the lateral ventricles and developed mild VM (> 10.1 mm). None of them developed severe VM. which has been also shown in other studies [30, 31]. The exclusion of progression by periodical follow-up seems reasonable.
Two cases were diagnosed with trisomy 21 postpartum (1.3%; n = 2/153). Both of these children showed an increased risk in the first trimester screening but denied further testing and the foetuses showed no additional anomalies on follow-up ultrasound exams apart from borderline VM. This shows the importance of offering a karyotyping even to isolated cases of borderline VM at presentation if first trimester screening was not performed.
After delivery, two children were transferred to the neonatal unit due to the VM. One child had asymmetric ventricles and the other one was diagnosed with hydrocephalus after premature delivery. Only one MRI showed abnormal findings: a child with a haemorrhagic hydrocephalus. Two showed mild neurologic abnormalities after birth, which included a child with pseudo microcephaly due to false position intrauterine and again the child with the increasing haemorrhagic hydrocephalus who showed reduced tonus. The increasing hydrocephalus was caused by the bleeding due to premature delivery rather than the VM being the underlying cause. None of the children was referred to a neuropediatrician. So, apart from one child, none of the children had clinically relevant findings.
Long-term follow-up after 2 years was available for 40 children. A total of 27.5% had head circumferences above the 90 percentile and 5.0% had head circumferences under the 10 percentile, explaining that large ventricles correlate with a large head.
A total of 27.5% had findings in the four categories of motor skills, cognitive behaviour, language development and social behaviour as rated by the paediatrician in charge.
According to the KiGGS study (“Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland”), 19.3% of the children at the age of 3–6 showed values above the normal range in the categories: emotionality, behaviour, hyperactivity, contacting and prosocial behaviour [32, 33]. There are additional studies investigating of early childhood development.
In Great Britain, the prevalence of psychological disorders was illustrated to be 22.3% at the age of 3 and in Germany 18.4% at the age of 3–14 years [32,33,34,35,36,37,38]. Since the number of patients in our study populations are comparatively small and the findings described by the paediatricians are not considered as diagnoses that need interventions, we assume that our findings are the reflection of the normal limits of early development and rather not findings that are linked to borderline VM. Here, there are some limitations to this study, which would be necessary for a definite interpretation such as the retrospective study design and the limited number of patients in the follow-up at 2 years.
Mostly important, there was only one case of shunt insertion and no case of cerebral palsy. This concludes that only 0.6% of the children had evident consequences at the age of 2 in cases of isolated borderline VM and the reason for that most likely was premature delivery. Our data would support the data from Signorelli who propose that an atrial width of 10–12 mm without abnormalities can be interpreted as a normal finding, since all children in their study (n = 38) with a width of 10–12 mm had a normal neurodevelopment up until 10 years after birth [11]. This leads us to the hypothesis that in the absence of anomalies, a width of the lateral ventricles of 8.0–10.0 mm is a variation of the norm.
Parental reassurance seems to be advisable in cases of borderline VM when a detailed ultrasound reveals no additional anomalies and first trimester screening showed low risk for chromosomal abnormalities. However, due to the two cases of trisomy 21 in our cohort, an isolated VM at 20 weeks in the absence of first trimester screening should prompt counselling on invasive testing or NIPT.
Based on our analysis, we suggest to set a cut-off for ventriculomegaly at the width of 10 mm or more and to describe a posterior lateral ventricle under 10 mm as a variation of the norm in the absence of associated anomalies. We therefore suggest that ventricles between 8 and 10 mm are evaluated by an ultrasound specialist to check for associated findings. Posterior lateral ventricles between 8 and 10 mm without associated abnormalities in the second or third trimester should lead to parental reassurance. Additional work up such as MRI and TORCH testing did not lead to clinical relevant additional information in our cohort of borderline VM but should be discussed with the parents as an option.
Even though isolated borderline VM showed favourable outcome in most of the patients, we nevertheless would recommend follow-up with ultrasound on a monthly basis for in utero progression to exclude the development of severe hypertensive hydrocephalus (≥ 15 mm) which would require interdisciplinary evaluation with prenatal specialists, obstetricians, neonatologist and paediatric neurosurgeons to develop a management plan.
Abbreviations
- VM:
-
Ventriculomegaly
- TORCH:
-
Toxoplasmosis, rubella, cytomegalovirus, herpes simplex virus 2 and other infections
- MRI:
-
Magnetic resonance imaging
- IUFD:
-
Intrauterine fetal death
- IUGR:
-
Intrauterine growth restriction
- WKS:
-
gestational week
- CMV:
-
Cytomegalovirus
- KIGGS:
-
Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland
References
Cardoza JD, Goldstein RB, Filly RA (1988) Exclusion of fetal ventriculomegaly with a single measurement: the width of the lateral ventricular atrium. Radiology 169(3):711–714
Gaglioti P, Oberto M, Todros T (2009) The significance of fetal ventriculomegaly: etiology, short- and long-term outcomes. Prenat Diagn 29(4):381–388
Kelly EN, Allen VM, Seaward G, Windrim R, Ryan G (2001) Mild ventriculomegaly in the fetus, natural history, associated findings and outcome of isolated mild ventriculomegaly: a literature review. Prenat Diagn 21(8):697–700
Breeze ACG, Alexander PMA, Murdoch EM, Missfelder-Lobos HH, Hackett GA, Lees CC (2007) Obstetric and neonatal outcomes in severe fetal ventriculomegaly. Prenat Diagn 27(2):124–129
Kennelly MM, Cooley SM, McParland PJ (2009) Natural history of apparently isolated severe fetal ventriculomegaly: perinatal survival and neurodevelopmental outcome. Prenat Diagn 29(12):1135–1140
Weichert J, Hartge D, Krapp M, Germer U, Gembruch U, Axt-Fliedner R (2010) Prevalence, characteristics and perinatal outcome of fetal ventriculomegaly in 29,000 pregnancies followed at a single institution. Fetal Diagn Ther 27(3):142–148
Gaglioti P, Danelon D, Bontempo S, Mombrò M, Cardaropoli S, Todros T (2005) Fetal cerebral ventriculomegaly: outcome in 176 cases. Ultrasound Obstet Gynecol 25(4):372–377
Joó JG, Tóth Z, Beke A, Papp C, Tóth-Pál E, Csaba A, Szigeti Z, Rab A, Papp Z (2008) Etiology, prenatal diagnostics and outcome of ventriculomegaly in 230 cases. Fetal Diagn Ther 24(3):254–263
Madazli R, Sal V, Erenel H, Gezer A, Ocak V (2011) Characteristics and outcome of 102 fetuses with fetal cerebral ventriculomegaly: experience of a university hospital in Turkey. Obstet Gynecol 31(2):142–145
Chiu T-H, Haliza G, Lin Y-H, Hung T-H, Hsu J-J, T’sang-T’ang H et al (2014) A retrospective study on the course and outcome of fetal ventriculomegaly. Taiwan J Obstet Gynecol 53(2):170–177
Signorelli M, Tiberti A, Valseriati D, Molin E, Cerri V, Groli C, Bianchi UA (2004) Width of the fetal lateral ventricular atrium between 10 and 12 mm: a simple variation of the norm? Ultrasound Obstet Gynecol 23(1):14–18
Pagani G, Thilaganathan B, Prefumo F (2014) Neurodevelopmental outcome in isolated mild fetal ventriculomegaly: systematic review and meta-analysis. Ultrasound Obstet Gynecol44(3):254–260
Larcos G, Gruenewald SM, Lui K (1994) Neonatal subependymal cysts detected by sonography: prevalence, sonographic findings, and clinical significance. AJR Am J Roentgenol 162(4):953–956
Adzick NS, Thom EA, Spong CY, Brock JW, Burrows PK, Johnson MP et al (2011) A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364(11):993–1004
Cavalheiro S, da Costa MDS, Mendonça JN, Dastoli PA, Suriano IC, Barbosa MM, Moron AF (2017) Antenatal management of fetal neurosurgical diseases. Childs Nerv Syst 33(7):1125–1141
Picone O, Simon I, Benachi A, Brunelle F, Sonigo P (2008) Comparison between ultrasound and magnetic resonance imaging in assessment of fetal cytomegalovirus infection. Prenat Diagn 28(8):753–758
Kagan KO, Hamprecht K (2017) Cytomegalovirus infection in pregnancy. Arch Gynecol Obstet 296(1):15–26
Pasquini L, Masini G, Gaini C, Franchi C, Trotta M, Dani C, di Tommaso M (2014) The utility of infection screening in isolated mild ventriculomegaly: an observational retrospective study on 141 fetuses. Prenat Diagn 34(13):1295–1300
Abdel-Fattah SA, Bhat A, Illanes S, Bartha JL, Carrington D (2005) TORCH test for fetal medicine indications: only CMV is necessary in the United Kingdom. Prenat Diagn 25(11):1028–1031
WHO | Preterm birth [Internet]. WHO. [cited 2017 Jan 8]. Available from: http://www.who.int/mediacentre/factsheets/fs363/en/. Accessed 8 Jan 2017
Ouahba J, Luton D, Vuillard E, Garel C, Gressens P, Blanc N, Elmaleh M, Evrard P, Oury JF (2006) Prenatal isolated mild ventriculomegaly: outcome in 167 cases. BJOG Int J Obstet Gynaecol 113(9):1072–1079
Baffero GM, Crovetto F, Fabietti I, Boito S, Fogliani R, Fumagalli M, Triulzi F, Mosca F, Fedele L, Persico N (2015) Prenatal ultrasound predictors of postnatal major cerebral abnormalities in fetuses with apparently isolated mild ventriculomegaly. Prenat Diagn 35(8):783–788
Nicolaides KH, Berry SB, Snijders RJM, Thorpe-Beeston JG, Gosden C (1990) Fetal lateral cerebral Ventriculomegaly: associated malformations and chromosomal defects. Fetal Diagn Ther 5(1):5–14
Benacerraf BR, Shipp TD, Bromley B, Levine D (2007) What does magnetic resonance imaging add to the prenatal sonographic diagnosis of ventriculomegaly? J Ultrasound Med 26(11):1513–1522
Salomon LJ, Ouahba J, Delezoide A-L, Vuillard E, Oury J-F, Sebag G, Garel C (2006) Third-trimester fetal MRI in isolated 10- to 12-mm ventriculomegaly: is it worth it? BJOG Int J Obstet Gynaecol 113(8):942–947
Yin S, Na Q, Chen J, Li-Ling J, Liu C (2010) Contribution of MRI to detect further anomalies in fetal Ventriculomegaly. Fetal Diagn Ther 27(1):20–24
Malinger G, Ben-Sira L, Lev D, Ben-Aroya Z, Kidron D, Lerman-Sagie T (2004) Fetal brain imaging: a comparison between magnetic resonance imaging and dedicated neurosonography. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 23(4):333–340
Paladini D, Quarantelli M, Sglavo G, Pastore G, Cavallaro A, D’Armiento MR et al (2014) Accuracy of neurosonography and MRI in clinical management of fetuses referred with central nervous system abnormalities. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 44(2):188–196
Parazzini C, Righini A, Doneda C, Arrigoni F, Rustico M, Lanna M, Triulzi F (2012) Is fetal magnetic resonance imaging indicated when ultrasound isolated mild ventriculomegaly is present in pregnancies with no risk factors? Prenat Diagn 32(8):752–757
Kutuk MS, Ozgun MT, Uludag S, Dolanbay M, Poyrazoglu HG, Tas M (2013) Postnatal outcome of isolated, nonprogressive, mild borderline fetal ventriculomegaly. Childs Nerv Syst 29(5):803–808
Chu N, Zhang Y, Yan Y, Ren Y, Wang L, Zhang B (2016) Fetal ventriculomegaly: pregnancy outcomes and follow-ups in ten years. Biosci Trends 10(2):125–132
Hölling H, Erhart M, Ravens-Sieberer U, Schlack R (2007) Verhaltensauffälligkeiten bei Kindern und Jugendlichen. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz 50(5–6):784–793
Hölling H, Schlack R, Petermann F, Ravens-Sieberer U, Mauz E, Group KS (2014) Psychische Auffälligkeiten und psychosoziale Beeinträchtigungen bei Kindern und Jugendlichen im Alter von 3 bis 17 Jahren in Deutschland – Prävalenz und zeitliche Trends zu 2 Erhebungszeitpunkten (2003–2006 und 2009–2012). Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz 57(7):807–819
Ihle W, Esser G (2002) Epidemiologie psychischer Störungen im Kindes- und Jugendalter. Psychol Rundsch 53(4):159–169
Richman N (1982) Pre-school to school: a behavioural study / N. Richman, J Stevenson, PJ Graham. Behavioural development: Children, 3-8 years Behaviour Development; Child psychology. London, New York: Academic Press, p 211-216
Weyerer S, Castell R, Biener A, Artner K, Dilling H (1988) Prevalence and treatment of psychiatric disorders in 3 to 14-year-old children: results of a representative field study in the small town rural region of Traunstein, upper Bavaria. Acta Psychiatr Scand 77(3):290–296
Kadesjö B, Gillberg C (1998) Attention deficits and clumsiness in Swedish 7-year-old children. Dev Med Child Neurol 40(12):796–804
Schott N, Roncesvalles N (2004) Motorische Ungeschicklichkeit. Z Sportpsychol 11(4):147–162
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Informed consent
There was no informed consent required for this retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tomic, K., Schönberger, H., Weber, P. et al. Significance of isolated borderline ventriculomegaly. Childs Nerv Syst 36, 393–399 (2020). https://doi.org/10.1007/s00381-019-04189-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04189-x