Abstract
The authors present the case of a previously healthy 12-year-old male with intractable seizures localized to a right frontal area of encephalomalacia and porencephalic cyst who underwent resection of the seizure focus. The surgical resection cavity extended into the right lateral ventricle, and due to encountered hemorrhage, Gelfoam was used for optimal hemostasis. The patient did well following the procedure, but presented 5 months later with headaches and emesis and was discovered to have obstructive hydrocephalus on imaging studies. Endoscopic third ventriculostomy (ETV) was performed, where Gelfoam was encountered in the third ventricle, obstructing the cerebral aqueduct. After the completion of the ETV, the patient did well and continues to be asymptomatic 1 year following the procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
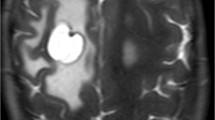
A 12-year-old previously healthy male with intractable seizures localized to a right frontal area of encephalomalacia and porencephalic cyst underwent resection of the seizure focus. The surgical resection cavity extended into the right lateral ventricle. The procedure was notable for significant venous bleeding, requiring two units of blood transfusion and packing of the resection cavity with Gelfoam (Pfizer, New York) in order to obtain hemostasis. He did well following the procedure and has had no recurrent seizures. Five months later, he returned to the emergency department (ED) with morning headaches, nausea, and vomiting for a duration of 1 week. A high-resolution MRI with sagittal FIESTA sequence revealed interval development of obstructive hydrocephalus with significant dilatation of the lateral and third ventricles (Fig. 1). There was evidence of cerebral aqueductal obstruction secondary to material of unclear etiology at the inlet of the aqueduct and further evidence of debris on the floor of the third ventricle.
a, b Initial postoperative T2 axial and T1 sagittal sequences demonstrating baseline, decompressed ventricles. c Axial T2 sequence at the time of obstruction with dilatation of the lateral and third ventricles obtained on presentation with headaches. d Sagittal FIESTA sequence demonstrating occlusion of the cerebral aqueduct and debris on the floor of the third ventricle
The decision was made to proceed with an endoscopic third ventriculostomy (ETV) for treatment of the hydrocephalus. Upon entering the lateral and third ventricles, floating debris consistent with Gelfoam was seen. Some of this material was noted on the walls of the ventricles; the material was probed with endoscopic grasper but proved to be adherent to the ependymal which otherwise appeared normal. The inferior aspect of the third ventricle was also covered by this debris, thus limiting the view of the floor of the third ventricle. The material was meticulously cleared using biopsy forceps until we were able to visualize the floor of the third ventricle, as well as the mammillary bodies posteriorly and the infundibular recess anteriorly (Fig. 2). We then proceeded with the ETV creating access into the prepontine cistern. The scope was then angled posteriorly and debris of similar consistency was also found to be plugging the cerebral aqueduct. The patient’s anatomy with respect to the foramen of Monro limited direct access to this area; therefore, the debris was not removed given the risk of forniceal retraction injury.
The patient did well after the procedure with resolution of his symptoms and was discharged home after 2 days. He presented again 1 week later with a pseudomeningocele centered around the ETV burr hole. He had no headaches or any other clinical symptoms of hydrocephalus. He underwent a tap of the pseudomeningocele and subsequent placement of a lumbar drain with a set goal of draining 10–15 mL of cerebrospinal fluid (CSF) per hour. The pseudomeningocele resolved, the lumbar drain was discontinued after 6 days, and the patient was discharged home. He has had no recurrence of the pseudomeningocele or any of his initial symptoms at 1 year follow-up.
To our knowledge, there have been no reported cases of iatrogenic, obstructive hydrocephalus caused by Gelfoam obstructing CSF flow through the cerebral aqueduct. Edwards et al. reported a case of a third ventriculostomy obstruction with Gelfoam following an ETV which was cured with removal of the obstructing Gelfoam via endoscopic exploration [1]. Our case emphasizes the need to minimize the entry of Gelfoam into the ventricular system during cranial surgery. In circumstances where violating the ventricular wall is inevitable, minimizing the size of the opening into the ventricles should be a priority to the surgeon in order to avoid access of foreign material into the ventricular system. Using minimal amounts of Gelfoam is also advisable when the ventricular wall is violated. Our patient developed obstructive symptoms 5 months after the initial craniotomy which may be explained by subacute migration of the Gelfoam products from the cortical resection cavity into the third ventricle. Neurosurgeons are ought to be mindful of this possibility in large cortical resections in which the ependymal boundary is violated.
Change history
26 April 2019
The original version of this article unfortunately contained an error. The authors apologize to have miss looked a typo of author name ���Joseph Diver���. The correct name is ���Joseph Driver���.
26 April 2019
The original version of this article unfortunately contained an error. The authors apologize to have miss looked a typo of author name ���Joseph Diver���. The correct name is ���Joseph Driver���.
26 April 2019
The original version of this article unfortunately contained an error. The authors apologize to have miss looked a typo of author name ���Joseph Diver���. The correct name is ���Joseph Driver���.
Reference
Edwards RJ, Dirks PB (2006) Gelfoam obstruction of endoscopic third ventriculostomy. J Neurosurg: Pediatrics 105:154–154. https://doi.org/10.3171/ped.2006.105.2.154
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this paper declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hazama, A., Diver, J., Grannan, B. et al. Iatrogenic obstructive hydrocephalus resulting from Gelfoam accumulation within the cerebral aqueduct: a case report. Childs Nerv Syst 34, 2333–2335 (2018). https://doi.org/10.1007/s00381-018-3874-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3874-y