Abstract
Introduction
Pediatric head trauma is one of the commonest presentations to emergency departments. Over 90% of such head injuries are considered mild, but still present risk acute clinical deterioration and longer term morbidity. Identifying which children are at risk of clinically important brain injuries remains challenging and much of the data on minor head injuries is based on the adult population.
Challenges in pediatrics
Children, however, are different, both anatomically and in terms of mechanism of injury, to adults and, even within the pediatric group, there are differences with age and stage of development.
Imaging
CT scans have added to the repertoire of clinicians in the assessment of pediatric head injury population, but judicious use is required given radiation exposure, malignancy risk, and resource constraints. Guidelines and head injury rules have been developed, for adults and children, to support decision-making in the emergency department though whether their use is applicable to all population groups is debatable. Further challenges in mild pediatric head trauma also include appropriate recommendations for school attendance and physical activity after discharge.
Further developments
Concern remains for second-impact syndrome and, in the longer term, for post-concussive syndrome and further research in both is still needed. Furthermore, the development of clinical decision rules raises further questions on the purpose of admitting children with minor head injuries and answering this question may aid the evolution of clinical decision guidelines.
Conclusions
The next generation of catheter with homogeneous flow patterns based on parametric designs may represent a step forward for the treatment of hydrocephalus, by possibly broadening their lifespan.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction and background
Pediatric head trauma is one of the commonest presentations in emergency departments accounting for 20,000 visits per year in Canadian hospitals and close to half a million emergency department (ED) visits [1] and 35,000 hospital admissions [2] in the USA. However, less than 1% of patients require neurosurgery [3].
Pediatric head trauma can be classified, according to Glasgow Coma Score (GCS), into mild/minor (GCS 14–15), moderate (GCS 9–13), and severe (GCS <9) [4], bearing in mind the differences in pediatric and adult GCS assessments [2]. Minor head trauma accounts for the overwhelming majority (70–90%) of head injury presentation to ED [5]. Only 4–7% of children with minor head trauma have a brain injury on CT [6]. Clinically important intracranial injuries occur in less than 5% of children presenting to emergency departments with minor head injuries and those requiring neurosurgery account for less than 1% [6, 7]. The challenge lies in identifying which patients with minor head injuries are likely to have clinically important brain injuries. The risk of a fatal traumatic brain injury (TBI) is 0.5 per 1000 [8]. Given most traumatic brain injuries identified on CT imaging do not need intervention studies using abnormal CT as a primary outcome measure may promote excessive CT scanning without altering management [7, 9]. Children with mild TBI account for 40–60% of TBI’s on CT yet are the least likely to need acute surgical intervention [7].
The causes of head injury in children differ to adults. Children are not drivers and are more likely to be passengers or pedestrians in motor vehicle accidents. Alcohol typically does not contribute to head injury in children. Falls and sports-related injury are the most common cause with the risk of intracranial injury being greater if the fall is from greater than 3 ft (or twice the length of the child).
Challenges in pediatric head injury
Children are unique to adults due to their relatively larger heads compared to overall body size, thinner calvarium and softer, less myelinated brain issue all resulting in a higher propensity to develop TBI after head trauma [10]. Children are more likely to suffer with diffuse axonal injury and less likely to develop space occupying hematomas requiring evacuation when compared to adults [10]. Clinical symptoms and signs of head injury, acute concussion, and raised intracranial pressure in children are less reliable and differ according to age and stage of development requiring vigilance in emergency assessment. In older children, symptoms mirror those in adults, namely headache, nausea, vomiting, seizures, lethargy, and drowsiness. In younger children, lethargy, irritability, and anorexia may be pertinent features. Amnesia is difficult to elicit in young children. In infants, hypotonia, listlessness, bulging, tense fontanelles, and sunsetting are features to be wary of.
As yet, no single symptom or sign has been identified as a reliable predictor of the severity of intracranial injury. Children under the age of 2 years and preverbal children can present particular dilemmas. Clinical and neurological assessment is more challenging, given their stage of development and communication and imaging, which requires a static patient, may necessitate sedation. Clinicians must also be particularly vigilant for cues pertaining to non-accidental injury.
Radiation exposure from CT remains a concern given the risk of lethal malignancy, estimated to be between 1 in 5000 and 1 in 1000 cranial CT scans in children [11]. This is risk in increased in younger children, particularly those less than 2 years of age. Younger children can also be challenging to assess which, in the setting of a general, non-pediatric hospital, may lead to a higher use of CT imaging in patient assessment [12]. These children arguably have the most to gain from standardization of management protocols to guide decision-making.
Initial assessment and the use of CT
There is no debate that children presenting with moderate or severe head injuries require computed tomography (CT) brain scans [7] as well as imaging of other body regions according to ATLS guidelines. Less well defined are the indications for brain imaging in those presenting with mild head injuries. The use of CT scans for head injury assessment has risen significantly in recent years [3] and now more than a third of children with minor head injury undergo CT in North America [13]. The concerns regarding sedation, radiation exposure [14], and low pick-up rate of positive findings [11] must be balanced against the unreliability of clinical signs as predictors of brain injury, particularly in preverbal children, and the potential for late deterioration due to missed pathology [15]. Historically, there has been wide variation in the use of CT, up to fourfold in some studies [16]. The trend of rising CT use is not evident in Australian emergency departments where the rate has remained static for a decade, at around 10% [3]. The considerable debate and need for management standardization has, over the past two decades, led to several clinical decision-making tools being devised to determine which patients need CT scans as part of their head injury workup. Many studies highlighting different clinical variables’ predictive values for CT findings are small and unvalidated. None of the initial studies were validated for children and early pediatric guidelines were based on adult data.
The Canadian CT rule group developed a sensitive clinical decision rule for CT in minor head injury, but for adults only [17]. The Children’s Head Injury Algorithm for the Prediction of Important Clinical Events (CHALICE) group in the UK were among the first to derive such a rule specifically for children in order to answer question who should have a CT scan and who can go home [18]. This was based on 23,000 children of all ages and was the first large-scale study of this type. They supported the discontinuation of skull X-rays in children with acute head injury (other than for NAI).
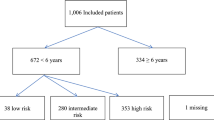
In 2009, the Pediatric Emergency Care Applied Research Network (PECARN) group took this one step further and derived validated rules separately for children younger than and older than 2 years of age on the premise that children under two have a different brain injury risk profile and are more sensitive to the effects of radiation from CT [7]. They concluded that using their six clinical variables 20–25% of CT scans could be avoided.
The Canadian Assessment of Tomography for Childhood Head Injury (CATCH) group prospectively devised a clinical decision rule to identify two levels of risk in children with minor head injury—the risk of requiring neurosurgical intervention and the risk of sustaining a brain injury on CT scan [6].
There are subtle differences between these three studies. CHALICE derived its rules from children of all ages presenting at any time point after the injury and, therefore, more compatible with real-world practice. CATCH and PECARN included patients presenting within 24 h of injury. In Australia and New Zealand, no such clinical rules have been devised [19] and this may contribute to the significantly lower scan rate compared to North America [3].
The three are not directly comparable as they addressed different clinical questions (and hence used different outcomes) assessing different ages of patients and injury severities [19]. Nonetheless, in the first prospective comparison of the three protocols [20], the PECARN guidelines demonstrated 100% sensitivity in identifying patients with clinically important brain injuries. CATCH and CHALICE missed one clinically important brain injury each and five and 14 clinically non-important injuries, respectively. CHALICE provided the greatest specificity of the rules followed by physician judgment. The same study also compared the guidelines to two measures of physician practice and suggested that a combination of PECARN rules and physician judgment provides an adequate combination of sensitivity and specificity though may depend on the experience of the physician. A later comparison with over 20,000 patients [21], a multicenter validation study, showed all three rules to perform well in identifying children with clinically important brain injury. However, it confirmed the findings of Easter et al. [20] that PECARN showed the highest sensitivity in identifying important brain injury and CHALICE demonstrated the highest specificity. Applying PECARN rules strictly would significantly increase the number of CT scans performed to unacceptable levels [22, 23]. The ideal rules must have high sensitivities, i.e., must be able to detect injury, and high negative predictive values, i.e., patients deemed to be low risk should not have significant brain injury. However, given the morbidity associated with missing a significant intracranial lesion, it is difficult to justify a high specificity at the cost of lower sensitivity [19].
Skull X-ray
Fractures on skull X-rays have previously been thought to predict an intracranial injury [24, 25] and, therefore, the need for CT imaging. However, this is less predictable in children, in whom severe intracranial injury can occur in the absence of a fracture, notwithstanding the propensity for inexperienced doctors to miss fractures on X-ray [26]. In 1998, the Society of British Neurological Surgeons recommended skull X-rays be performed in patients with mild or moderate, but not severe, head injuries [27] and this was restricted further in 2003, in the UK by the National Institute of Clinical Excellence, to infants at risk of non-accidental injury and to children in remote areas where access to was problematic [28]. The use of X-rays has continued to decline as the indications for CT have broadened [28]. The more restricted use of X-rays has not been detrimental to children, has not increased admission rates and, although it has increased the use of CT, it has slightly reduced the radiation dose per head injury [29]. Nonetheless, there may remain a role for the use of skull X-rays in the setting of minor head injury in children under 2 years of age [30, 31]. In keeping with this, the Canadian Paediatric Society supports the use of skull X-rays in children in this group with large boggy scalp hematomas [2]. Confirmed or suspected abusive head trauma is a further indication for skull X-ray in children.
Discharge and advice
Canadian Paediatric Society guidelines suggest asymptomatic patients can be discharged home under the supervision of reliable parents or guardians with clearly written instructions describing yellow and red flag signs which warrant further medical attention [2].
Failure to improve warrants admission and a brain CT is recommended after 18–24 h of symptoms. Those less than 2 years old require greater caution with longer observation periods and more frequent clinical assessments.
A further challenge in minor pediatric head trauma is the discharge advice to offer parents, in particular relating to participation in contact sports. The key concern centers on the prevention of second-impact syndrome. Controversial in its existence [32], it occurs when a symptomatic head injury is followed by a second impact while symptoms from the first injury persist [33]. There is debate surrounding the required severity of the second impact (and, indeed, whether or not a direct blow to the head is even necessary), the required time lag between the two impacts and the mechanism(s) involved. Although rare, it can result in catastrophic cerebral edema, disability, and death [33]. One proposed mechanism is a hyperemia leading to vascular engorgement on a background of dysregulation of the parasympathetic system from the first injury. This leads to failure of autoregulation [34], vasodilation, malignant cerebral edema, and critically raised intracranial pressure [35]. Alternative mechanisms include metabolic disturbances secondary to multiple blows, resulting in free radical formation, neuronal damage, and susceptibility to further injury [36]. A recent review identified 17 cases in the literature [33] though up to 36 cases were identified with less strict definitions of the syndrome. Most commonly reported in adolescents and young adults between the ages of 16 and 19 years of age, it is most likely to occur within the first couple of weeks after the first injury. Nonetheless, patients may be at risk as long they are experiencing post-concussive symptoms which guide expert recommendations to avoid contact sports until symptoms have cleared [23]. Risk factors for second-impact syndrome appear to be male gender and younger age and playing American football, but further work is required to clarify this rare, but catastrophic phenomenon [33].
The American Academy of Neurology has published return to play guidelines [37] incorporating these risk factors into their guidance strategies. Similarly, the Canadian Paediatric Society has developed its own guidelines on the management of sports-related concussion including advice on returning to school and sports participation in children after minor head injury [38]. A five stage Graduated Return to Learn protocol is commenced with cognitive rest and absence from school. Gradually increasing cognitive tasks and school attendance ends with the fifth and final stage of the protocol marking the start of the Graduated Return to Play protocol. Thomas et al. argue, in a randomized study, that extended rest (5 days) offers no benefit over shorter (1 to 2 days) rest periods [39]. However, their follow-up was only 10 days and excluded children under 11 years old, those who did not speak English and those who lived several hours away from the study center [39]. Its applicability, therefore, to real-world practice is limited. The Return to Play Protocol is a six-stage process starting with no activity and incremental increases until full, normal play is resumed [38]. The principles include that full academic activity should be resumed prior to commencing exercise and although cognitive exertion can commence before symptom-resolution, it is recommended that sporting activity begins only after all signs and symptoms of concussion have been resolved for 7 to 10 days [38]. Each stage should last a minimum of 24 h and should symptoms recur, the child should rest and recommence the same stage once symptoms have resolved again. These guidelines are based on expert opinion rather than prospective, randomized studies [40] and advocate caution and conservatism in its approach.
Conclusions
Head trauma is a frequent occurrence in childhood and adolescence, with most injuries being minor and without sequelae. A systematic approach to the clinical assessment of the patient presenting with head trauma is recommended, with investigations being conducted according to the symptoms, signs, and estimated likelihood of intracranial pathology. Most patients can be either discharged or observed in hospital for a short period. Prospectively validated clinical decision rules are a useful adjunct in the physician’s armory and should be used to form standardized protocols for head injury management. Given initial management and investigation of children with minor head injuries and the fact that most never need intervention, it raises the question why do we actually admit children after minor injury? Is it mechanism of injury, is it symptom management, is it imaging findings or the likelihood of deterioration and requiring neurosurgery? Only once we really answer this question will we be able to design robust decision trees for all aspects of managing minor head injury in children.
Change history
07 October 2017
The published version of this article unfortunately contained an error.
References
Gordon KE (2006) Pediatric minor traumatic brain injury. Semin Pediatr Neurol 13:243–255
Farrell CA (2013) Canadian Paediatric Society acute care committee position statement: management of the paediatric patient with acute head trauma. Paediatr Child Health 18:253–258
Oakley E, May R, Hoeppner T, Sinn K, Furyk J, Craig S, Rosengarten P, Kochar A, Krieser D, Dalton S, Dalziel S, Neutze J, Cain T, Jachno K, Babl FE, Paediatric Research in Emergency Departments International C (2017) Computed tomography for head injuries in children: change in Australian usage rates over time. Emergency medicine Australasia : EMA 29:192–197
Holmes JF, Palchak MJ, MacFarlane T, Kuppermann N (2005) Performance of the pediatric glasgow coma scale in children with blunt head trauma. Acad Emerg Med Off J Soc Acad Emerg Med 12:814–819
Roberts RM, Bunting J, Pertini M (2017) Factors that predict discharge recommendations following paediatric mild traumatic brain injury. Brain Inj:1–7
Osmond MH, Klassen TP, Wells GA, Correll R, Jarvis A, Joubert G, Bailey B, Chauvin-Kimoff L, Pusic M, McConnell D, Nijssen-Jordan C, Silver N, Taylor B, Stiell IG, Pediatric Emergency Research Canada Head Injury Study G (2010) CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne 182:341–348
Kuppermann N, Holmes JF, Dayan PS, Hoyle JD Jr, Atabaki SM, Holubkov R, Nadel FM, Monroe D, Stanley RM, Borgialli DA, Badawy MK, Schunk JE, Quayle KS, Mahajan P, Lichenstein R, Lillis KA, Tunik MG, Jacobs ES, Callahan JM, Gorelick MH, Glass TF, Lee LK, Bachman MC, Cooper A, Powell EC, Gerardi MJ, Melville KA, Muizelaar JP, Wisner DH, Zuspan SJ, Dean JM, Wootton-Gorges SL, Pediatric Emergency Care Applied Research N (2009) Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 374:1160–1170
Da Dalt L, Marchi AG, Laudizi L, Crichiutti G, Messi G, Pavanello L, Valent F, Barbone F (2006) Predictors of intracranial injuries in children after blunt head trauma. Eur J Pediatr 165:142–148
Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM (2000) Indications for computed tomography in patients with minor head injury. N Engl J Med 343:100–105
Sookplung P, Vavilala MS (2009) What is new in pediatric traumatic brain injury? Curr Opin Anaesthesiol 22:572–578
Brenner DJ, Hall EJ (2007) Computed tomography—an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Blackwell CD, Gorelick M, Holmes JF, Bandyopadhyay S, Kuppermann N (2007) Pediatric head trauma: changes in use of computed tomography in emergency departments in the United States over time. Ann Emerg Med 49:320–324
Mannix R, Meehan WP, Monuteaux MC, Bachur RG (2012) Computed tomography for minor head injury: variation and trends in major United States pediatric emergency departments. J Pediatr 160(136–139):e131
Hennelly KE, Mannix R, Nigrovic LE, Lee LK, Thompson KM, Monuteaux MC, Proctor M, Schutzman S (2013) Pediatric traumatic brain injury and radiation risks: a clinical decision analysis. J Pediatr 162:392–397
Thiessen ML, Woolridge DP (2006) Pediatric minor closed head injury. Pediatric clinics of North America 53: 1–26, v
Stiell IG, Wells GA, Vandemheen K, Laupacis A, Brison R, Eisenhauer MA, Greenberg GH, MacPhail I, McKnight RD, Reardon M, Verbeek R, Worthington J, Lesiuk H (1997) Variation in ED use of computed tomography for patients with minor head injury. Ann Emerg Med 30:14–22
Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, McKnight RD, Verbeek R, Brison R, Cass D, Eisenhauer ME, Greenberg G, Worthington J (2001) The Canadian CT head rule for patients with minor head injury. Lancet 357:1391–1396
Dunning J, Daly JP, Lomas JP, Lecky F, Batchelor J, Mackway-Jones K, Children’s head injury algorithm for the prediction of important clinical events study g (2006) Derivation of the children's head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Arch Dis Child 91:885–891
Babl FE, Borland ML, Phillips N, Kochar A, Dalton S, McCaskill M, Cheek JA, Gilhotra Y, Furyk J, Neutze J, Lyttle MD, Bressan S, Donath S, Molesworth C, Jachno K, Ward B, Williams A, Baylis A, Crowe L, Oakley E, Dalziel SR, Paediatric Research in Emergency Departments International C (2017) Accuracy of PECARN, CATCH, and CHALICE head injury decision rules in children: a prospective cohort study. Lancet
Easter JS, Bakes K, Dhaliwal J, Miller M, Caruso E, Haukoos JS (2014) Comparison of PECARN, CATCH, and CHALICE rules for children with minor head injury: a prospective cohort study. Annals of emergency medicine 64: 145–152, 152 e141-145
Babl FE, Lyttle MD, Bressan S, Borland M, Phillips N, Kochar A, Dalziel SR, Dalton S, Cheek JA, Furyk J, Gilhotra Y, Neutze J, Ward B, Donath S, Jachno K, Crowe L, Williams A, Oakley E, network Pr (2014) A prospective observational study to assess the diagnostic accuracy of clinical decision rules for children presenting to emergency departments after head injuries (protocol): the Australasian Paediatric Head Injury Rules Study (APHIRST). BMC Pediatr 14: 148
Mower WR (2017) Paediatric head imaging decisions are not child's play. Lancet
Pickering A, Harnan S, Fitzgerald P, Pandor A, Goodacre S (2011) Clinical decision rules for children with minor head injury: a systematic review. Arch Dis Child 96:414–421
Erlichman DB, Blumfield E, Rajpathak S, Weiss A (2010) Association between linear skull fractures and intracranial hemorrhage in children with minor head trauma. Pediatr Radiol 40:1375–1379
Teasdale GM, Murray G, Anderson E, Mendelow AD, MacMillan R, Jennett B, Brookes M (1990) Risks of acute traumatic intracranial haematoma in children and adults: implications for managing head injuries. BMJ 300:363–367
Lloyd DA, Carty H, Patterson M, Butcher CK, Roe D (1997) Predictive value of skull radiography for intracranial injury in children with blunt head injury. Lancet 349:821–824
Bartlett J, Kett-White R, Mendelow AD, Miller JD, Pickard J, Teasdale G (1998) Recommendations from the Society of British Neurological Surgeons. Br J Neurosurg 12:349–352
Royal College of Surgeons of England Trauma C (2005) The Royal College of Surgeons of England: a position paper on the acute management of patients with head injury (2005). Ann R Coll Surg Engl 87:323–325
Reed MJ, Browning JG, Wilkinson AG, Beattie T (2005) Can we abolish skull x rays for head injury? Arch Dis Child 90:859–864
Greenes DS, Schutzman SA (2001) Clinical significance of scalp abnormalities in asymptomatic head-injured infants. Pediatr Emerg Care 17:88–92
Schutzman SA, Barnes P, Duhaime AC, Greenes D, Homer C, Jaffe D, Lewis RJ, Luerssen TG, Schunk J (2001) Evaluation and management of children younger than two years old with apparently minor head trauma: proposed guidelines. Pediatrics 107:983–993
McCrory P (2001) Does second impact syndrome exist? Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine 11:144–149
McLendon LA, Kralik SF, Grayson PA, Golomb MR (2016) The controversial second impact syndrome: a review of the literature. Pediatr Neurol 62:9–17
Bey T, Ostick B (2009) Second impact syndrome. West J Emerg Med 10:6–10
Squier W, Mack J, Green A, Aziz T (2012) The pathophysiology of brain swelling associated with subdural hemorrhage: the role of the trigeminovascular system. Child’s nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery 28:2005–2015
Signoretti S, Lazzarino G, Tavazzi B, Vagnozzi R (2011) The pathophysiology of concussion. PM & R : the journal of injury, function, and rehabilitation 3:S359–S368
Giza CC, Kutcher JS, Ashwal S, Barth J, Getchius TS, Gioia GA, Gronseth GS, Guskiewicz K, Mandel S, Manley G, McKeag DB, Thurman DJ, Zafonte R (2013) Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the guideline development Subcommittee of the American Academy of Neurology. Neurology 80:2250–2257
Purcell LK, Canadian Paediatric Society HAL, Sports Medicine C (2014) Sport-related concussion: evaluation and management. Paediatr Child Health 19:153–165
Thomas DG, Apps JN, Hoffmann RG, McCrea M, Hammeke T (2015) Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics 135:213–223
Purcell L (2009) What are the most appropriate return-to-play guidelines for concussed child athletes? Br J Sports Med 43(Suppl 1):i51–i55
Author information
Authors and Affiliations
Corresponding author
Additional information
A correction to this article is available online at https://doi.org/10.1007/s00381-017-3608-6.
Rights and permissions
About this article
Cite this article
Singh, N., Singhal, A. Challenges in minor TBI and indications for head CT in pediatric TBI—an update. Childs Nerv Syst 33, 1677–1681 (2017). https://doi.org/10.1007/s00381-017-3535-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3535-6