Abstract
Questions/purposes
Adolescent idiopathic scoliosis is a 3D spine deformity that worsens during the whole growth. New methods for spinal growth modulation with flexible spinal implants have been described to avoid progression of the deformity during growth spurt. The main limitations are that no specific ancillaries and devices are available, which makes the surgery technically demanding.
Methods
We have developed a new method of spinal growth tethering using minimal invasive videothoracoscopic approach. Fixation is performed with staples and synthetic ligament on the lateral aspect of vertebral bodies on main curvature convexity. Patients with progressive thoracic idiopathic scoliosis despite the brace treatment were included. The clinical and radiological examinations were compared before and 2 years after surgery.
Results
Six patients with flexible thoracic curves with a mean age 11.2 ± 1.2 years and a mean Cobb angle 45° ± 10° (35–60) were operated. All were skeletally immature. At last follow-up, the Cobb angle was stable. None of the patient underwent fusion.
Conclusions
The procedure allowed a stabilization of the deformity during growth spurt. Validated devices and further studies with longer term follow-up are needed to confirm the efficiency of this technique. This small cohort of patients is a source of reflection for further medical devices developments.
Level of Evidence
Level 4 case series comparing to not randomized studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a 3D spine deformity that worsens during the whole growth. The aim of bracing is to avoid progression of the deformity and surgical fusion of the spine at skeletal maturity [1–3]. However, in many cases, brace does not stop the curve progression. Several factors are responsible: scoliosis virulence, poor brace tolerance, and brace inefficiency.
A novel method for spinal growth modulation with a flexible spinal implant has been recently described to avoid progression of the deformity during growth spurt [4–6]. The concept is to stop the vertebral growth on the convex side. This dynamic epiphysiodesis of the convex side aims to equilibrate the height of both concave and convex sides of the vertebra without fusion [7]. For the first time, it is possible to obtain correction of the scoliosis without fusion through mini-invasive approach.
This technique is still at its debuts. But no specific medical device has been developed for this technique. The actual devices used are off-label in the US and non-EC marked for this indication. Thus, we have no prospective data and long-term outcomes of this technique. Moreover, there is no specific ancillary, which makes the surgery technically demanding with the current device. For these reasons, we tried to develop a simpler method of spinal growth tethering using minimally invasive video-thoracoscopic approach.
The aim of this study is to present clinical and radiological outcome at 2-year follow-up of the first patients treated with this technique.
Materials and methods
Patients with an AIS with failure of conservative treatment were selected for the study. Only patients with severe thoracic curves (Cobb angle >40°) with significant growth remaining (Risser 0, premenarchal) were informed of this novel technique. The prerequisite was also a flexible curve with a Cobb angle reduction of more than 50% on the right side bending tests. The patients included had already in our hands an indication of conventional surgical treatment, if they were at skeletal maturity. In these cases, the novel technique was performed as an alternative to fusion in order to avoid further curve progression and fusion ultimately. Oral and written information was given to patients and their parents about the novel medical device, the off-label indication and the surgical strategy. Informed consent was retrieved for all patients. In case of disagreement the brace treatment was pursued until the proper timing for conventional fusion (arthrodesis).
The device implanted is a combination of chrome-cobalt staples and a synthetic ligament. The staples (Orengo 5 – Orthomed) have a width of 8 mm and a length of 25 mm. We use two superimposed polyethylene terephthalate (PET) bands (Universal clamp – Zimmer Spine). Biomechanical studies available on the tensile strength to failure of the band are freely available. It reaches 830 ± 70 N. We have performed biomechanical studies by ourselves to test the strength to failure of the band fixed to porc vertebra with the staples. It reaches at least 704 N and its deformation reaches 25% (unpublished data).
Surgery was performed under general anesthesia with selective intubation of the left lung. It allowed a better visibility and made the surgery technically easier. The patient position was lateral decubitus on a radiolucent table. The whole procedure was performed through anterolateral approach of the thoracic spine with video-assisted thoracoscopy [8, 9]. Reduction of the curve as complete as possible was achieved by the patient position on the table (Fig. 1). Logs were positioned under the pelvis and shoulders so as to achieve the best correction of the curve (Fig. 2). The upper and the lower vertebrae of the main curve were identified with the help of fluoroscopy.
Three to four incisions are required for placement of all of the staples.
The incisions must be located on the middle of the vertebral bodies on the lateral view. Indeed, the positioning of the incisions highly impacts the position of the staples in the vertebral body. In our practice, we make a first posterior incision in the chest located at the apex of the convexity to put the camera and have an overview of the thorax cavity. Then, we put a pin percutaneously under video-assisted thoracoscopic control to optimize the position of the incisions. Three to four incisions are necessary to instrument up to seven levels. Through an incision, it is possible to instrument up to three vertebrae. To date, this procedure was performed only on thoracic curves.
Conventional coelioscopic trocars of 11 mm are positioned in the incisions. The exposure of the lateral aspect of the vertebral body is carried out after coagulation of segmental vessels.
The upper staple is positioned but not impacted on the most cranial vertebral body. The staples do not need to be perfectly perpendicular to the vertebra (Fig. 2). They ideally need to converge toward the virtual center of the curve. The position of each staple is controlled under fluoroscopy with AP and lateral views.
The synthetic band is then driven under the staple which is then fully impacted, and the ligament is held in tension at the distal end of the curve with a specific device according to the principle of the “sardine box” (Fig. 3). The tension of the ligaments is not yet monitored. But the tension has no corrective virtue. It is the positioning of the patient which reduces the curvature. The device must allow the partial maintenance of the correction obtained during surgery. Loss of correction is inevitable in standing position as the system is flexible. All of the staples are then impacted from top to bottom. The tension of the ligament can be readapted at each stage (Fig. 4). A fluoroscopic control with AP and lateral views is performed before the section of the proximal and distal ends of the ligament. A chest tube is introduced through one of the incisions. Operative time is usually 120–180 min.
Postoperative care
Stand up position is authorized at day 1 or 2 according to pain. The chest tube is removed at day 1. We put a brace for 45 days to prevent the failure of the staples during osteointegration. The resumption of sporting activities is authorized empirically from the fourth postoperative month.
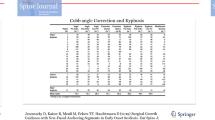
Clinical and radiological data of patients such as sex, age, state of the Y cartilage, Risser score, main thoracic and lumbar Cobb angles, and the Lenke classification were recorded. The thoracic and lumbar Cobb angles were recorded postoperatively at 7 days, 3 months, 6 months, 1 year and 2 years follow-up (Fig. 5). Complications during surgery and during follow-up were recorded such as blood loss, loss of correction, failure of the staple, or the synthetic ligament. Main clinical data are shown in Table 1.
Statistical analysis was performed using Statview 5.5 (SAS Institute, Cary, NC, USA).
Results
Six patients, five girls and one boy, with a mean age of 11.2 ± 1.2 (9–12) were included. The mean follow-up was 21.6 months (18–24). The description of the series is shown in Table 1.
Three patients had Lenke 1C AIS, two patients had Lenke 1A AIS, and one patient had Lenke 2A AIS.
The mean main thoracic curvature before surgery was 45° ± 10° (35–60), and the mean lumbar curvature was 33° ± 5° (30–40).
Seven days after spinal growth tethering, the mean thoracic curvature was 38° ± 7° (30–50), p = 0.21. Seven days after spinal growth tethering, the mean lumbar curvature was 23° ± 6° (15–30).
The correction remained constant over the time at last follow-up with a mean thoracic curvature of 38° ± 7° (30–50) and a mean lumbar curvature of 25° ± 9° (15–40). All patients were well-balanced in the frontal plan and the sagital plan on full spine X-rays.
No spinal growth tethering was performed on the lumbar curve. The main results are summarized in Table 2.
No complications were recorded. No postoperative neurologic defects were noted. The mean blood loss was 100 cm3 (50–150). The mean operative time was 120 min (100–150). No loss of correction was seen and no failure of staple or the synthetic ligament was recorded at last follow-up. No overcorrection was noted.
Discussion
Preliminary results from this small cohort of patients show a stabilization of the Cobb angle with well-balanced spines at 2 years follow-up: mean Cobb angle 38° ± 7° (30–50), p = 0.21. The main interest of the procedure is the stabilization of the deformity during growth spurt to avoid arthrodesis in patients who are skeletally immature. In this report, the procedure was safe without complications such as infection, neurologic defects, or blood loss.
Some limitations can be pointed out. First of all, we have included a small number of patients in the study. Because this technique is not fully established and consensual, we only selected patients with severe curves that already had an indication of surgery. This novel technique was accepted by the parents has the last chance to avoid fusion. The inclusion criteria were established on the basis of the previous published results [4, 5].
Like the Dynesys system, the medical device used in this study is not FDA or CE approved for spinal growth tethering. This is the main limitation for the use of this device. However, we need to work on this and motivate the industry to develop these kinds of devices. Work is in progress to obtain a CE marked device for this indication. It is consensual that fusion is not the ideal treatment for the patient and the surgeon. We think that spinal growth tethering devices could be a novel generation of scoliosis treatments within the next decade. The regulation is however actually in the USA against the use of dynamic devices without associated fusion even for posterior approach. Conversely, in Europe, dynamic devices can be implanted solely without fusion through posterior approach. A big step must be done before we have a dynamic device FDA approved through anterior approach in pediatrics, in the USA. Maybe, the development will come from Europe.
Biomechanical evaluation of flexible is lacking in the literature. We have used the Dynesys system as a predicate for the device we have used in this study. The prerequisite was to obtain, in theory, similar mechanical characteristics between the Dynesys and our device before implantation. This is the reason why we used two superimposed bands. However, we do not have sufficient follow-up to assess the fatigue resistance of all flexible tethers. In fact, we do not actually know the fatigue resistance needed at the bone/anchor and anchor/tether interfaces required to achieve the best possible correction. Moreover, we do not know the tension needed to maintain the correction immediately after the surgery and then “hold” the convex-side growth [7]. But after 2-year follow-up, we did not observe any modification of the curve despite the growth and any staple dislodgment or breakage. This gives an idea of the tolerance of the device for future developments. On the other side, we did not observe curve correction.
Spinal growth tethering was performed by Samdani et al. with 2-year follow-up using the Dynesis system (Zimmer Spine) [4, 5]. They have reported the 1- and 2-year follow-up experience of this technique in, respectively, 32 and 11 skeletally immature patients with idiopathic scoliosis [4, 5]. The mean preoperative Cobb angle was 43° ± 8°. After 1 year of follow-up, the curves improved to 18° ± 11°. After 2 years of evolution, the curves continued to improve to 13.5° ± 11°. With the current technique, the curves did not improve but we found a stabilization of the deformity. We only observed a “brace effect” but no “epiphysiodesis effect” [7]. We can suppose that the tension of the band was not sufficient to maintain correction of the curve immediately after the surgery. We indeed observed a loss of correction between our preoperative radiographs and first erect X-rays.
But the procedure is easier than Dynesys implantation through thoracoscopic approach. Our experience with these both devices is clearly, from a technical point of view, in favor of the staples and ligament. Maybe both of these devices need to be optimized to reach all the objectives. Like brace treatment, fusion is still possible in case of failure or curve progression [10]. And more interestingly, it does not impair the possibility of selective fusion. Techniques like growing rods need an anchorage in the lumbar spine which supposes a fusion of the same levels at skeletal maturity. From a more philosophical point of view, it is questionable to ultimately fuse a stable spine of 40° with a flexible tether on. If the patient is well balanced, it is certainly preferable to have a stable flexible spine of 40° than a straight and rigid one [11–15].
Conclusion
Spinal growth tethering is an interesting alternative technique to fusion to stabilize progressive scoliotic patients who are skeletally immature. We need validated devices and further studies with longer term follow-up to confirm the efficiency of this technique. This small cohort of patients is a source of reflection for further medical devices developments. We have to keep in mind that the final objective is to reach the possibility of decreasing the rate of fusion in our patients with progressive curves.
Addendum
The devices used in this study (band and staples) are CE marked. But we have used these devices in a different way that they are supposed to be used (if we follow the recommendations of the user notice) on our own responsibility. In fact, the staples do not have a specific destination. But the ligament (which is a part of the Zimmer U-clamp) is not supposed to be used through anterior approach. But it is a similar polyester band used everywhere else in the body for ligament reconstruction (shoulder, knee, etc.). And the staples are to be used with a synthetic or a natural ligament [16]. The technique is a kind of “spine ligamentoplasty”. But, the manufacturers do not recommend the association of these two medical devices, and their combination was performed strictly under the own responsibility of the senior surgeon (A Courvoisier). Actually, the Dynesys system which is used in the USA and Canada to perform vertebral body tethering (VBT) is also not FDA approved nor CE marked for this indication [4, 5]. The patients and their parents are aware of the situation. They understand the experimental aspect of this surgery, but they do not like the perspective of a spine fusion. We have clearly informed the patients and their parents that it is a new technique with a medical device that is not intended to be use in this situation. We have collected all the informed consents. The whole story of the development of VBT techniques and the problems of FDA and Europe regulation on such medical devices was described recently [7, 16].
References
Courvoisier A, Drevelle X, Vialle R, Dubousset J, Skalli W (2013) 3D analysis of brace treatment in idiopathic scoliosis. Eur Spine J 22:2449–2455
Nachemson AL, Peterson LE (1995) Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am 77:815–822
Charles YP, Daures JP, de Rosa V, Diméglio A (2006) Progression risk of idiopathic juvenile scoliosis during pubertal growth. Spine (Phila Pa 1976) 31:1933–1942
Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR (2015) Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J 24:1533–1539
Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR (2014) Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976) 39:1688–1693
Crawford CH 3rd, Lenke LG (2010) Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Joint Surg Am 92:202–209
Courvoisier A, Eid A, Bourgeois E, Griffet J (2015) Growth tethering devices for idiopathic scoliosis. Expert Rev Med Devices 12:449–456
Lenke LG (2003) Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 28:S36–S43
Pompeo E, Mancini F, Ippolito E, Mineo TC (2010) Videothoracoscopic approach to the spine in idiopathic scoliosis. Thorac Surg Clin 20:311–321
Weinstein SL, Dolan LA, Wright JG et al (2013) Effects of bracing in adolescents with idiopathic scoliosis. N England J Med 369:1512–1521
Green DW, Lawhorne TW, Widmann RF et al (2003) Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 28:2078–2085
Betz RR, Kim J, D'Andrea LP, Mulcahey MJ, Balsara RK, Clements DH (2003) An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: a feasibility, safety, and utility study. Spine (Phila Pa 1976) 28:S255–S265
Betz RR, Ranade A, Samdani AF, Chafetz R, D'Andrea LP, Gaughan JP, Asghar J, Grewal H, Mulcahey MJ (2010) Vertebral body stapling: a fusionless treatment option for a growing child with moderate idiopathic scoliosis. Spine (Phila Pa 1976) 35:169–176
Theologis AA, Cahill P, Auriemma M, Betz R, Diab M (2013) Vertebral body stapling in children younger than 10 years with idiopathic scoliosis with curve magnitude of 30° to 39°. Spine (Phila Pa 1976) 38:1583–1588
O'leary PT, Sturm PF, Hammerberg KW, Lubicky JP, Mardjetko SM (2011) Convex hemiepiphysiodesis: the limits of vertebral stapling. Spine (Phila Pa 1976) 36:1579–1583
Courvoisier A (2016) The future of academic innovation in the field of medical devices: is innovation still possible in orthopedics? Expert Rev Med Devices 13:807–813
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest concerning this article.
Electronic supplementary material
ESM 1
(PDF 798 kb)
Rights and permissions
About this article
Cite this article
Boudissa, M., Eid, A., Bourgeois, E. et al. Early outcomes of spinal growth tethering for idiopathic scoliosis with a novel device: a prospective study with 2 years of follow-up. Childs Nerv Syst 33, 813–818 (2017). https://doi.org/10.1007/s00381-017-3367-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3367-4