Abstract
Aim
The objective of our study was to investigate nerve conduction in normoglycemic obese children.
Methods
A total of 60 children with obesity (30 female and 30 male) and 30 healthy children (15 female and 15 male) were enrolled in the study. Insulin resistance (IR) and other metabolic disturbances were investigated and nerve conduction was measured in all participants. Obese children were divided into groups according to the presence of IR. All results were compared between these subgroups.
Results
The nerve conduction velocity (NCV) of motor median nerves in the IR+ group was significantly higher than that in the IR− group and lower than that in the control group. The NCV of the motor peroneal nerve in the IR+ group was significantly lower than that in the IR− group. The sensory nerve action potential (SNAP) of the sensory median nerve was significantly lower in the IR+ group compared to that in the IR− group. The sensory sural nerve’s SNAP was significantly lower in the IR+ group than that in the control group.
Conclusion
Nerve conduction tests may help to detect early pathologies in peripheral nerves and to decrease morbidities in obese children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity, one of the most important public health problems in children, leads to abnormalities in the endocrine, cardiovascular, gastrointestinal, neurological, and other systems [1]. The worldwide increasing prevalence of childhood obesity has caused an increased prevalence of associated comorbidities [2].
Insulin has a critical role in regulating and providing neuronal function during the lifetime, starting in the intrauterine period. It has many important functions in neuronal development and differentiation, migration, synapse formation, myelin and neurotransmitter production, neuronal plasticity, and gene expression [3–6].
Earlier development of insulin resistance and type 2 diabetes mellitus (T2DM), which are the most important complications associated with obesity, leads to an earlier onset of progressive neuropathy [7]. Recent studies have shown peripheral nerve impairment, determined by electrophysiological studies, in both adult and childhood obese patients with impaired glucose tolerance. Hyperglycemia, insulin resistance, and/or other complications of obesity may contribute to the pathophysiology of peripheral neuropathy [8, 9]. The objective of this study was to investigate nerve conduction and to determine the relationship with insulin resistance in normoglycemic obese children.
Methods
A total of 60 children with obesity (30 female and 30 male) between the ages of 8 and 18 years who were admitted to the pediatric endocrinology department for obesity evaluation, and 30 healthy age-matched children (15 female and 15 male), as a control group, participated in the study. Obesity was defined as body mass index (BMI) above the 95th percentile [10]. Healthy controls were selected from voluntary children with BMI between the 10th and 85th percentiles who were admitted outpatient department for various symptoms not related to obesity complications. A detailed physical examination including the evaluation of systemic, endocrinologic, and neurologic diseases were performed. All patients were pubertal. Patients diagnosed with syndromes or diseases which may lead to neuropathy including renal and hepatic failure, endocrine disorders such as thyroid dysfunction, vitamin deficiencies were excluded. Neurotoxic drugs and vitamin preparations using toxin exposure story in the last 6 months were another exclusion criteria. Anthropometric measurements were performed by the same physician, with the patients wearing only underclothes and without shoes. Weight was measured using a digital weighing scale (SECA 841, Hamburg, Germany) to the nearest 100 g, and height was measured using a stadiometer to the nearest 0.1 cm. BMI was calculated as weight/height 2 and expressed as kilogram per square meter. BMI standard deviation score (BMI-SDS) was also calculated [10, 11]. Children defined as prepubertal according to Tanner staging and those with any neurological and systemic disorders such as neuromuscular disease or diabetes were excluded. A detailed systemic and neurological examination including the evaluation of motor functions, muscle power, and senses was performed.
Measurements of fasting plasma glucose, serum triglyceride (TG), total cholesterol (TC), and high-density lipoprotein cholesterol (HDL-C) levels were performed enzymatically using an autoanalyzer (Olympus 2700, Olympus Medical Systems Corp. Tokyo, Japan). Low-density lipoprotein cholesterol (LDL-C) level was calculated using the Friedewald equation. Fasting plasma insulin level was measured by the ELISA method using an automated immunoassay analyzer (E170; Roche Diagnostics, USA). Insulin resistance (IR) was calculated by the formulation of homeostasis model of assessment (HOMA): fasting glucose (mg/dL) × fasting insulin (IU/mL)/405. A HOMA value >4 was considered as positive IR [12, 13].
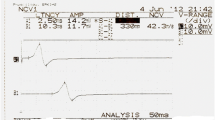
Electrophysiological examinations were performed by the same investigator in a quiet room with limb temperatures greater than 32 °C. Nerve conduction studies were performed using a Keypoint electromyography device (Dantec, Bristol, UK).
Unilateral right median nerve sensory and motor conduction, sural nerve sensory conduction, and peroneal nerve motor conduction studies were performed using supramaximal percutaneous stimulation.
Median sensory action potentials were obtained from the index finger with ring electrodes antidromically. The stimulation point was the middle of the wrist between the tendons to the flexor carpi radialis and palmaris longus. The compound muscle action potential (CMAP) of the median nerve was obtained from the abductor pollicis brevis muscle (APB) while the distal stimulation site was at the wrist and the proximal stimulation site was at the antecubital fossa, over the brachial artery pulse.
Sural nerve conduction studies were performed by stimulating slightly lateral to the midline in the lower one third of the back side of the leg and recording the sensory nerve action potential (SNAP) from the posterior to the lateral malleolus. The CMAP of the peroneal nerve was obtained from the extensor digitorum brevis muscle by stimulating the anterior ankle slightly lateral to the tibialis anterior tendon and below the fibular head.
CMAPs were measured from the baseline to the negative peak. SNAPs were measured from the initial positive peak to the negative peak, or from the isoelectric line to the negative peak in case of initial positive peak absence. Latencies of motor and sensory responses were measured from the stimulation point to the wave onset.
Sensory nerve conduction velocities were calculated by dividing the distance between stimulation and recording electrodes by the first positive peak latency of action potential. Motor conduction velocities were calculated by dividing the distance between proximal and distal stimulation points by the subtraction of proximal and distal latencies. The distance between the distal stimulation point and the recording point was equal in all patients. F latency was determined by the minimum F latency.
As descriptive statistics, number and percentage for categorical variables and mean ± standard deviation values for continuous variables were used. Obese and control groups were compared using chi-square (χ 2) test for categorical variables, and Student’s t test for continuous variables. The mean values of each group were analyzed using one-way analysis of variance (ANOVA) test. Tukey’s post hoc test was performed for two-group comparisons of significant values. The relationship between variables was evaluated by Pearson’s correlation analysis. Statistical Package for the Social Sciences (SPSS) for Windows version 15.0 was used for all analyses, and differences were considered significant at a level of significance of p < 0.05.
Parents were provided informed consent and the study was approved by the Institutional Review Board of the Gulhane Military School of Medicine.
Results
Demographic and anthropometric features of the study population were reported in Table 1. Age and sex did not show significant differences between obese and non-obese children (p > 0.05). There was also no difference between groups regarding LDL-C levels. On the other hand, fasting blood glucose, TG, HOMA-IR, fasting plasma insulin levels, body weight, BMI, and BMI-SDS were significantly higher in the obese group (p = 0.05, p = 0.01, and p < 0.001 for the others, respectively), whereas HDL-C level was significantly higher in the control group (p < 0.001).
IR was determined in 27 of 60 obese children. Clinical and laboratory findings of obese children regarding IR are indicated in Table 1. In addition to HOMA-IR values, fasting plasma glucose and fasting plasma insulin were significantly higher in the IR+ group. There was no statistically significant difference between IR+ and IR− groups with respect to other metabolic and anthropometric variables.
Nerve conduction velocity (NCV) of the median nerve and SNAP of the sural nerve were significantly lower in obese children than that in non-obese children.
Obese children with IR and those without IR were compared according to electrophysiological parameters (Table 2 and Table 3). The NCV of motor peroneal nerve of the IR+ group was significantly lower than that in the IR– group and control group. The NCV of the motor median nerve was significantly lower in the IR+ group than that in the control group. The SNAP of the sensory median nerve was significantly lower in the IR+ group compared to that in the IR− group. In addition, the sensory sural nerve’s SNAP was significantly lower in the IR+ group than that in the control group.
Correlation analysis between the electrophysiological parameters was statistically different in the IR+ and IR− groups, and HOMA-IR, fasting blood glucose, BMI-SDS, and insulin levels were also compared (Table 4). There was a statistically significant negative correlation between the NCV of the motor peroneal nerve and HOMA-IR, insulin and BMI-SDS. The SNAP of the sensory median nerve was also negatively correlated with HOMA-IR and insulin.
Discussion
In the current study, subclinical peripheral nerve abnormalities, including decelerations in NCV of the motor nerves and decreases in SNAP of sensory nerves, were found in obese children compared to healthy subjects. These abnormalities were more significant in obese children with IR. Nerve conduction abnormalities in obese children may arise from metabolic disorders or an entrapment effect of subcutaneous fat tissue. Decreases in amplitudes and slowing of velocities in nerve conduction studies are findings of chronic axonal neuropathies. Metabolic deteriorations, mainly diabetes mellitus, are the most frequent etiologic factors for axonal neuropathies [14].
Neuropathy has also been detected in patients with impaired glucose tolerance. It was suggested that episodic hyperglycemia is the most important reason for neuropathy in patients with prediabetes [8, 15]. However, nerve abnormalities in normoglycemic patients with hyperinsulinism were also reported [16]. In the current study, glycemic levels of all participants were normal. However, we found lower SNAP values in patients with IR compared to the IR− group. There was also a difference between the IR+ group and the IR− group in terms of sural nerve SNAP, but this was not statistically significant. The sural motor nerve conduction velocity was also decreased in the IR+ group compared to that in the control group. However, there was no difference between the IR− group and healthy subjects. In addition, significant correlations between HOMA-IR, plasma insulin level, and electrophysiological parameters were detected. All these results suggest that hyperinsulinism and IR may affect nerve function regardless of glycemic levels.
Previous evoked potential studies of obese patients in which superficial cutaneous electrodes were used suggested that decreased amplitudes and subcutaneous fat tissue were reasons for decelerations in amplitudes [17–19]. In the present study, superficial cutaneous electrodes were used; however, apart from the sural nerve, none of the nerves indicated low SNAP in obese patients compared to healthy subjects. The sural nerve was previously reported to be affected by metabolic disorders [20]. Therefore, we can speculate that a decrease in sural nerve SNAP is the result of metabolic complications of obesity rather than subcutaneous fat tissue. Moreover, there was no difference between the control group and obese children without IR. Therefore, the difference in SNAP results could be associated with IR.
Miscio et al. [19] reported nerve conduction abnormalities in non-diabetic obese adults related to IR. Another study including 2035 adult subjects with metabolic syndrome suggested that IR might play an important role in the development of peripheral neuropathy [21]. In another study comparing patients with carpal tunnel syndrome and healthy control subjects, a relation between idiopathic carpal tunnel syndrome and IR was indicated [22]. Lee et al. [23] found an independent association between IR and peripheral neuropathy in subjects with type 2 diabetes. Several animal studies also reported a relationship between peripheral neuropathies and IR [24, 25]. Due to application difficulties, studies of peripheral neuropathies in children are rare. İnce et al. [9] revealed that the amplitude of the medial plantar nerve was significantly lower in obese children with impaired glucose tolerance and insulin resistance. Our study did not examine the medial plantar nerve. In another study performed in children, an association between IR and BAEP abnormalities was shown, and it was also detected that abnormalities originated mainly from the peripheral part of the auditory nerve. Therefore, it was suggested that the effects of insulin resistance on neural transmission may be starting from peripheral tissues [26].
Insulin receptors have been detected on peripheral nerves. It is thought that these receptors act in nerve regeneration [27]. High insulin levels in patients with IR may lead to downregulation of insulin receptors [28]. Therefore, the regenerative function of nerves could be impaired [16]. In addition, hyperinsulinism and IR may increase basal membrane thickness and cause vascular endothelial dysfunction. Over time, these changes may lead to vasa nervorum ischemia, endoneuronal perfusion disturbances, and eventually axonal degeneration. A study performed in mice proposed the reduction in peripheral nervous system (PNS) insulin signaling as a mechanism that may contribute to sensory neuron dysfunction [25]. All these pathologies can result in decreased nerve conduction velocities in obese patients with insulin resistance [14, 29]. Obese children have increased risk for insulin resistance and T2DM [30]. Earlier development of insulin resistance and T2DM lead to an earlier onset of neuropathy.
Glucotoxicity was stated as a major factor in the pathogenesis of neuropathy in diabetic patients [20, 31, 32]. However, it may be suggested that not only glucotoxicity but also insulin deficiency may play a role in the development of neuropathy. Indeed, in the current study, insulin resistance was found to be related to nerve conduction abnormalities in normoglycemic obese children. Therefore, we can speculate that IR and insulin deficiency may lead to these subclinical early abnormalities, and later on hyperglycemia then accelerates the process of neuropathy in diabetic patients (Fig. 1).
All these results suggest that the pathological process may begin in the periphery due to IR in patients in whom diabetes has not begun. It was reported that thin unmyelinated nerve fibers are affected first in impaired glucose tolerance and early diabetic neuropathy [33]. Nerve conduction studies are used to detect the involvement of thick fibers. Therefore, it can also be suggested that thick fibers can be affected by IR, and nerve conduction tests may be helpful in early detection of neuropathy in non-diabetic obese patients with IR.
There are some limitations of our study. The present study had a cross-sectional design and a small sample of patients. Therefore, our data may represent a “snapshot” of the nerve conduction values in our patients. Longitudinal studies with larger samples of patients and including sequential measurements of anthropometric and biochemical markers related to the pathogenesis of neuropathies may elucidate the underlying relationships. HOMA-IR was used to measure IR instead of the glucose clamp technique, which is the gold standard method. Besides, studies could not be performed for all nerves and extremities because of compliance difficulties in pediatric patients. On the other hand, this study had a controlled design and a classification of obese patients according to IR that could help to explain the possible physiopathological mechanisms relating obesity to neuropathy.
In conclusion, we identified peripheral nerve pathologies present in obese children compared to healthy subjects. The pathological results were more significant in obese children with IR. Nerve conduction tests may help to detect early pathologies in peripheral nerves and to decrease morbidities in obese children.
References
Unger R, Kreeger L, Christoffel KK (1990) Childhood obesity. Medical and familial correlates and age of onset. Clin Pediatr (Phila) 29:368–373
Twarog JP, Politis MD, Woods EL, Daniel LM, Sonneville KR (2016) Is obesity becoming the new normal? Age, gender and racial/ethnic differences in parental misperception of obesity as being ‘About the Right Weight’. International journal of obesity
Mielke JG, Taghibiglou C, Wang YT (2006) Endogenous insulin signaling protects cultured neurons from oxygen-glucose deprivation-induced cell death. Neuroscience 143:165–173
Diaz B, Pimentel B, de Pablo F, de La Rosa EJ (1999) Apoptotic cell death of proliferating neuroepithelial cells in the embryonic retina is prevented by insulin. Eur J Neurosci 11:1624–1632
Plum L, Schubert M, Bruning JC (2005) The role of insulin receptor signaling in the brain. Trends Endocrinol Metab 16:59–65
Marks DR, Tucker K, Cavallin MA, Mast TG, Fadool DA (2009) Awake intranasal insulin delivery modifies protein complexes and alters memory, anxiety, and olfactory behaviors. J Neurosci 29:6734–6751
Dietz WH, Robinson TN (2005) Clinical practice. Overweight children and adolescents. N Engl J Med 352:2100–2109
Gordon Smith A, Robinson Singleton J (2006) Idiopathic neuropathy, prediabetes and the metabolic syndrome. J Neurol Sci 242:9–14
Ince H, Tasdemir HA, Aydin M, Ozyurek H, Tilki HE (2015) Evaluation of nerve conduction studies in obese children with insulin resistance or impaired glucose tolerance. J Child Neurol 30:989–999
Neyzi O, Bundak R, Gokcay G, Gunoz H, Furman A, Darendeliler F, Bas F (2015) Reference values for weight, height, head circumference, and body mass index in Turkish children. Journal of clinical research in pediatric endocrinology 7:280–293
Neyzi O, Gunoz H, Furman A, Bundak R, Gökçay G, Darendeliler F, Baş F (2008) Weight, height, head circumference and body mass index references for Turkish children. Cocuk Saglıgı ve Hastalıkları Dergisi 51:1–14
Valerio G, Licenziati MR, Iannuzzi A, Franzese A, Siani P, Riccardi G, Rubba P (2006) Insulin resistance and impaired glucose tolerance in obese children and adolescents from Southern Italy. Nutr Metab Cardiovasc Dis 16:279–284
Reinehr T, Kiess W, Kapellen T, Andler W (2004) Insulin sensitivity among obese children and adolescents, according to degree of weight loss. Pediatrics 114:1569–1573
Polat M, Tekgul H, Kilincer A, Tosun A, Terlemez S, Serdaroglu G, Uludag B, Gokben S (2006) Electrodiagnostic pattern approach for childhood polyneuropathies. Pediatr Neurol 35:11–17
Head KA (2006) Peripheral neuropathy: pathogenic mechanisms and alternative therapies. Altern Med Rev 11:294–329
Delaney CA, Mouser JV, Westerman RA (1994) Insulin sensitivity and sensory nerve function in non-diabetic human subjects. Neurosci Lett 180:277–280
Dorfman LJ, Robinson LR (1997) AAEM minimonograph #47: normative data in electrodiagnostic medicine. ff. Muscle Nerve 20:4–14
Buschbacher RM (1998) Body mass index effect on common nerve conduction study measurements. Muscle Nerve 21:1398–1404
Miscio G, Guastamacchia G, Brunani A, Priano L, Baudo S, Mauro A (2005) Obesity and peripheral neuropathy risk: a dangerous liaison. J Peripher Nerv Syst 10:354–358
Karsidag S, Morali S, Sargin M, Salman S, Karsidag K, Us O (2005) The electrophysiological findings of subclinical neuropathy in patients with recently diagnosed type 1 diabetes mellitus. Diabetes Res Clin Pract 67:211–219
Han L, Ji L, Chang J, Wen J, Zhao W, Shi H, Zhou L, Li Y, Hu R, Hu J, Lu B (2015) Peripheral neuropathy is associated with insulin resistance independent of metabolic syndrome. Diabetol Metab Syndr 7:14
Plastino M, Fava A, Carmela C, De Bartolo M, Ermio C, Cristiano D, Ettore M, Abenavoli L, Bosco D (2011) Insulin resistance increases risk of carpal tunnel syndrome: a case-control study. J Peripher Nerv Syst 16:186–190
Lee KO, Nam JS, Ahn CW, Hong JM, Kim SM, Sunwoo IN, Moon JS, Na SJ, Choi YC (2012) Insulin resistance is independently associated with peripheral and autonomic neuropathy in Korean type 2 diabetic patients. Acta Diabetol 49:97–103
Nguyen VA, Le T, Tong M, Mellion M, Gilchrist J, de la Monte SM (2012) Experimental alcohol-related peripheral neuropathy: role of insulin/IGF resistance. Nutrients 4:1042–1057
Grote CW, Groover AL, Ryals JM, Geiger PC, Feldman EL, Wright DE (2013) Peripheral nervous system insulin resistance in ob/ob mice. Acta Neuropathol Commun 1:15
Akin O, Arslan M, Akgun H, Yavuz ST, Sari E, Tascilar ME, Ulas UH, Yesilkaya E, Unay B (2016) Visual and brainstem auditory evoked potentials in children with obesity. Brain Dev 38:310–316
Ishii DN (2001) Neurobiology of insulin and insulin-like growth factors. In: Loughlin SE, Fallon JH (eds) Neurotrophic Factors. Academic Press, New York, pp. 415–442
Okabayashi Y, Maddux BA, McDonald AR, Logsdon CD, Williams JA, Goldfine ID (1989) Mechanisms of insulin-induced insulin-receptor downregulation. Decrease of receptor biosynthesis and mRNA levels. Diabetes 38:182–187
Johnsen B, Fuglsang-Frederiksen A (2000) Electrodiagnosis of polyneuropathy. Neurophysiol Clin 30:339–351
Cali AM, Caprio S (2008) Obesity in children and adolescents. J Clin Endocrinol Metab 93:S31–S36
Gregori B, Galie E, Pro S, Clementi A, Accornero N (2006) Luminance and chromatic visual evoked potentials in type I and type II diabetes: relationships with peripheral neuropathy. Neurol Sci 27:323–327
Ziegler D, Langen KJ, Herzog H, Kuwert T, Muhlen H, Feinendegen LE, Gries FA (1994) Cerebral glucose metabolism in type 1 diabetic patients. Diabet Med 11:205–209
Sumner CJ, Sheth S, Griffin JW, Cornblath DR, Polydefkis M (2003) The spectrum of neuropathy in diabetes and impaired glucose tolerance. Neurology 60:108–111
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Akın, O., Eker, İ., Arslan, M. et al. Association of nerve conduction impairment and insulin resistance in children with obesity. Childs Nerv Syst 32, 2219–2224 (2016). https://doi.org/10.1007/s00381-016-3210-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-016-3210-3