Abstract
Background
Choroid plexus papilloma is a rare intracranial neoplasm derived from choroid plexus epithelium accounting for less than 1 % of all brain tumors. These tumors are highly vascularized, and tumor resection is difficult, especially in small children, due to severe intraoperative bleeding. Preoperative embolization is helpful to reduce intraoperative bleeding, but it may not be possible in small children or if the tumor has no suitable feeding vessels for embolization.
Methods
We present the case of a 2-year-old girl with a giant choroid plexus papilloma. An attempt of tumor resection was previously performed in another clinic, but the surgery was aborted due to massive intraoperative bleeding and only a biopsy was done. Angiography showed no suitable vessels for embolization. A new attempt of tumor removal was carried out, but again, severe intraoperative bleeding occurred and only a partial resection was possible. Intratumoral embolization with onyx through direct percutaneous puncture was performed.
Results
Radical tumor removal was possible after two additional surgeries. Intraoperative blood loss was 345 ml (first surgery = only partial removal), 250 ml (second procedure = 1/3 of tumor volume resected), and 250 ml (third surgery = total removal). The patient presented no additional deficits.
Conclusions
Intratumoral percutaneous embolization with onyx was very helpful in reducing intraoperative bleeding in this case. Safe radical tumor resection was possible. This technique may be useful for those surgeons dealing with highly vascularized tumors, especially in small children. No report of intratumoral embolization with onyx in cases of intracerebral tumors could be found in the literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Choroid plexus papillomas are rare intracranial tumors, more frequent in children, and derived from choroid plexus epithelium. They account for less than 1 % of all brain tumors and for 2–3 % of tumors in children under 15 years of age [4, 5, 7, 10]. Congenital choroid plexus papillomas have been reported by many authors corresponding to 7.9 % of fetal brain tumors prenatally diagnosed by ultrasound [3, 8]. Choroid plexus tumors can be primarily divided into two major categories, choroid plexus papillomas and choroid plexus carcinomas. Choroid plexus papillomas are slow-growing, benign lesions (WHO grade I) being more prevalent than choroid plexus carcinomas in a proportion of 5:1. They are predominantly located in the lateral ventricles (50 %) and in the fourth ventricle (40 %) [4, 18, 21]. The majority of patients present initial symptoms due to increased intracranial pressure and hydrocephalus caused by CSF overproduction, obstruction, or impairment in absorption [11]. These lesions are highly vascularized predominantly through the anterior and posterior choroidal arteries making surgical removal difficult, especially in small children. Radical surgical removal is curative for benign tumors with 100 % tumor-free survival in 5 years [13, 17]. Preoperative embolization and chemotherapy with vinblastine have been used to reduce intraoperative bleeding [2, 9, 18]. However, preoperative embolization is not feasible in many patients and some lesions will not respond to vinblastine. In this report, we present our experience with percutaneous intratumoral tumor embolization with onyx.
Case report
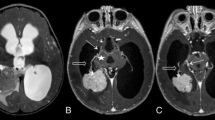
This 2-year-old girl presented with neurocognitive impairment, progressive gait disturbance, right hemiparesis, and an enlarged head circumference. Her estimated blood volume was 1020 ml. MRI showed a large contrast-enhancing tumor (132 × 107 × 99 mm) occupying the left lateral ventricle, with markedly atrophy of the left cerebral hemisphere, compression of the third ventricle, and dilatation of the right lateral ventricle (Fig. 1). Tumor removal was attempted in another clinic, but surgery was stopped due to excessive intraoperative bleeding and hemodynamic instability. A biopsy was taken and the histological examination revealed a benign choroid plexus papilloma. Angiography showed multiple small tortuous feeding vessels arising from the anterior choroidal, anterior cerebral, middle cerebral, and posterior cerebral arteries and from large draining veins. Intra-arterial embolization was not possible due to the small caliber of feeding vessels (Fig. 2).
Post-gadolinium-DTPA axial T1-weighted gradient echo (FSPGR) sequence depicts a large heterogeneous intraventricular mass exceeding the limits of the lateral ventricle into the adjacent brain parenchyma. The lesion shows intense heterogeneous enhancement persisting hypointense foci in between (possibly related to cystic degeneration or necrotic foci). The brain parenchyma in the vicinity shows heterogeneous signal as well, with multiple, confluent cystic-appearing areas of predominantly peripheral contrast enhancement. There is mass effect with the midline shift to the right midbrain distortion and compression and partial third ventricle obliteration
Cerebral digital subtraction angiography (DSA) with left internal carotid artery iodinated contrast media injection shows notorious mass effect with cranial and ventral dislocation of M1 and M2 left middle cerebral artery branches. This study shows the presence of multiple small tortuous feeding vessels with “vasculopathic” appearance arising from the anterior choroidal, anterior, and middle cerebral arteries with some areas of tumoral “blush” and early draining veins, suggesting some degree of arteriovenous shunting (arrows)
A new attempt of surgical removal was indicated. The previous left temporoparietal craniotomy was skipped and a corticotomy through the gliotic area was performed. The lateral wall of the ventricle was opened and a soft reddish lesion was identified. Debulking of the tumor produced severe bleeding, difficult to control, which forced us to stop the procedure. A small sample for biopsy was taken and the histopathological examination confirmed the diagnosis of a benign choroid plexus papilloma (WHO grade 1). On the seventh postoperative day, the patient became somnolent due to worsening of the hydrocephalus and a ventricle-peritoneal shunt was inserted. She had a full recovery and was discharged from the hospital. Chemotherapy with vincristine (0.4 mg/kg) was initiated to reduce tumor vascularization [2]. This chemotherapy was maintained for a 12-week course, but no change in tumor size or vascularization was observed in the control MRI. Percutaneous navigation-guided intratumoral embolization with onyx was performed. For each 50 cm3 of the tumor volume was infused a dose of 1 ml of onyx (total of 3 ml) through a burr hole. Due to a possibility of repeat the procedure for a residual tumor, this dose was delivered in the periphery of the tumor, aiming a relevant clinical result using low dose and avoiding significant increase in intracranial pressure (Fig. 3). Reduction in tumor vascularization was expected to occur through local compression and inflammatory reaction.
A second surgery was performed 1 week after the intratumoral embolization, and a larger portion of the lesion could be removed (Fig. 4a). This time, the intraoperative bleeding was much lower; however, a total removal was not possible due to the low weight of the child, and a third procedure was planned. There was no postoperative complication and the patient was discharged some days after this second procedure.
a Post-gadolinium-DTPA axial T1-weighted gradient echo (FSPGR) sequence 1 week after the percutaneous intratumoral embolization depicts some degree of tumoral mass reduction and increment in the conspicuity and dimensions of the hypointense foci in between the tumor previously noted (possibly related to areas of necrosis). b FSPGR sequence shows the surgical result with gross resection of heterogeneous enhancing areas, previously noted
Two months after the second surgery, a new intratumoral embolization with onyx was carried out. Again, 2 ml of onyx was injected. Complete excision of the tumor was achieved with 250 ml of blood loss (Table 1) (Fig. 4b). The patient recovered from this final procedure without any new neurological deficit.
Discussion
Choroid plexus papillomas are benign, slow-growing, highly vascularized lesions that can be cured by radical tumor resection. Young children are often affected and these patients have small blood volume. Intraoperative bleeding can be life-threatening and is a major surgical difficulty [6, 12, 14]. Preoperative embolization and multiple surgeries may be required to complete removal of tumor [18]. Some surgical strategies like direct approach to the vascular pedicles (possible in small tumors) and quick tumor removal may be helpful [16].
Preoperative endovascular embolization is feasible when the feeding vessels are large enough to be catheterized to inject the embolization particle [17, 18]. Some tumors present rich vascularity from small deep vessels arising from multiple vascular trunks, which are too small and tortuous, as in our case, for endovascular catheterizing [9, 15, 20]. Chemotherapy with vincristine has been reported to reduce blood flow and tumor size [2]. In our case, no reduction of tumor vascularization or tumor size was observed with this treatment.
Intratumoral embolizations with onyx and cyanoacrylate in cases of juvenile nasoangiofibroma and in other head and neck highly vascularized tumors have been described [1, 19]. We could not find in the literature any description of onyx usage for intratumoral embolization in cases of choroid plexus papillomas or other intracerebral tumors. Onyx is a nonadhesive liquid embolic agent compound of EVOH (ethylene vinyl alcohol) co-polymer dissolved in DMSO (dimethyl sulfoxide). It is currently one of the most widely used liquid materials for embolization of intracranial arteriovenous malformations and tumors. The real mechanism of how intratumoral onyx embolization reduces tumor vascularization is not clear. Local inflammatory changes causing vascular sclerosis and local pressure may produce vascular thrombosis. Its use through percutaneous direct intratumoral injection, as performed in this case report, may help surgical removal of challenging highly vascularized tumors.
References
Abud DG, Mounayer C, Benndorf G, Piotin M, Spelle L, Moret J (2004) Intratumoral injection of cyanoacrylate glue in head and neck paragangliomas. Am J Neuroradiol 25:1457–1462
Addo NK, Kamaly-Asl ID, Josan VA, Kelsey AM, Estlin EJ (2011) Preoperative vincristine for an inoperable choroid plexus papilloma: a case discussion and review of the literature. J Neurosurg Pediatr 8:149–153
Adra AM, Mejides AA, Salman FA, Landy HJ, Helfgott AW (1994) Prenatal sonographic diagnosis of a third ventricle choroid plexus papilloma. Prenat Diagn 14:865–867
Aguzzi A, Brandner S, Paulus W (2000) Choroid plexus tumours. In: Kleihues P, Cavenee WK (eds) World Health Organization classification of tumors. Pathology and genetics of tumours of the nervous system. IARC Press, Lyon, pp 84–86
Barbosa M, Rebelo O, Barbosa P, Lacerda A, Fernandes R (2001) Choroid plexus tumours: a surgically treated series. Neurocirugia (Astur) 12:7–16
Bohm E, Strang R (1961) Choroid plexus papillomas. J Neurosurg 18:493–500
Chow E, Reardon DA, Shah AB, Jenkins JJ, Langston J, Heideman RL, Sanford RA, Kun LE, Merchant TE (1999) Pediatric choroid plexus neoplasms. Int J Radiat Oncol Biol Phys 44:249–254
Di Rocco C, Ianelli A (1997) Poor outcome of bilateral congenital choroid plexus papillomas with extreme hydrocephalus. Eur Neurol 37:33–37
Di Rocco F, Caldarelli M, Sabatino G, Tamburrini G, Rocco CD (2004) Lateral ventricle choroid plexus papilloma extending into the third ventricle. Pediatr Neurosurg 40:314–316
Gjerris F, Agerlin N, Børgesen SE, Buhl L, Haase J, Klinken L, Mortensen AC, Olsen JH, Ovesen N, Reske-Nielsen E, Schmidt K (1998) Epidemiology and prognosis in children treated for intracranial tumours in Denmark 1960–1984. Childs Nerv Syst 14:302–311
Gudeman SK, Sullivan HG, Rosner MJ, Becker DP (1979) Surgical removal of bilateral papillomas of the choroid plexus of the lateral ventricles with resolution of hydrocephalus. Case report. J Neurosurg 50:677–681
Hawkins JC 3rd (1980) Treatment of choroid plexus papillomas in children: a brief analysis of twenty years’ experience. Neurosurgery 6:380–384
Levy ML, Goldfarb A, Hyder DJ, Gonzales-Gomez I, Nelson M, Gilles FH, McComb JG (2001) Choroid plexus tumors in children: significance of stromal invasion. Neurosurgery 48:303–309
Matson DD, Crofton FD (1960) Papilloma of the choroid plexus in childhood. J Neurosurg 17:1002–1027
McEvoy AW, Phipps KP, Ellison DW, Elsmore AJ, Thompson D, Harkness W, Hayward RD (2000) Management of choroid plexus tumours in children: 20 years experience at a single neurosurgical centre. Pediatr Neurosurg 32:192–199
McGirr SJ, Ebersold MJ, Scheithauer BW, Quast LM, Shaw EG (1988) Choroid plexus papillomas: long-term follow-up results in a surgically treated series. J Neurosurg 69:843–849
Nagib MG, O’Fallon MT (2000) Lateral ventricle choroid plexus papilloma in childhood: management and complications. Surg Neurol 54:366–372
Pencalet P, Sainte-Rose C, Lellouch-Tubiana A, Kalifa C, Brunelle F, Sgouros S, Meyer P, Cinalli G, Zerah M, Pierre-Kahn A, Renier D (1998) Papillomas and carcinomas of the choroid plexus in children. J Neurosurg 88:521–528
Piérot L, Boulin A, Castaings L, Chabolle F, Moret J (1994) Embolization by direct puncture of hypervascularized ORL tumors. [Article in French]. Ann Otolaryngol Chir Cervicofac 111:403–409
Raimondi AJ, Gutierrez FA (1975) Diagnosis and surgical treatment of choroid plexus papillomas. Childs Brain 1:81–115
Wolff JE, Sajedi M, Brant R, Coppes MJ, Egeler RM (2002) Choroid plexus tumours. Br J Cancer 87:1086–1091
Acknowledgments
We gratefully acknowledge Ronaldo Pereira Vosgerau, neuroradiologist, for providing the image data and comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jung, G.S., Ruschel, L.G., Leal, A.G. et al. Embolization of a giant hypervascularized choroid plexus papilloma with onyx by direct puncture: a case report. Childs Nerv Syst 32, 717–721 (2016). https://doi.org/10.1007/s00381-015-2915-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2915-z