Abstract
Introduction
We report the case of a 2-year-old boy who showed a huge midline mass in the brain at prenatal assessment.
Case report
After birth, magnetic resonance imaging (MRI) revealed a conglomerate mass with an infolded microgyrus at the midline, which was suspected as a midline brain-in-brain malformation. MRI also showed incomplete cleavage of his frontal cortex and thalamus, consistent with lobar holoprosencephaly. The patient underwent an incisional biopsy of the mass on the second day of life. The mass consisted of normal central nervous tissue with gray and white matter, representing a heterotopic brain. The malformation was considered to be a subcortical heterotopia. With maturity, focal signal changes and decreased cerebral perfusion became clear on brain imaging, suggesting secondary glial degeneration. Coincident with these MRI abnormalities, the child developed psychomotor retardation and severe epilepsy focused on the side of the intracranial mass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Holoprosencephaly (HPE) is a rare but very important disorder involving a complex congenital brain malformation characterized by failure of the forebrain to separate into two cerebral hemispheres, a process normally completed by the fifth week of gestation [1]. Affected children often have severe mental retardation, spastic quadriparesis, athetosis, endocrinologic disorders, and epilepsy. There are currently four generally accepted subtypes of HPE as follows: alobar, semilobar, lobar, and middle interhemispheric variant [1].
A midline brain-in-brain malformation is a rare complication of HPE, with only five cases previously reported [2–4] and no histopathological reports. Herein, we present a 2-year-old boy with lobar HPE who had a huge midline mass in the brain suggestive of a midline brain-in-brain malformation. The histological, physiological, and imaging data demonstrated that the mass was a subcortical heterotopia. The developmental origin of this malformation is discussed in association with the origin of HPE coexisting as a background anomaly.
Patient
The patient was a 2-year-old boy, the first child of a healthy Japanese mother. There was no family history of epilepsy or developmental delay. A fetal ultrasound at 30 weeks disclosed a clear cerebral mass that deviated from the midline and caused lateral ventriculomegaly. As the mass and ventricle progressively enlarged, an elective Cesarean section was performed at 36 weeks. Apgar scores were 5, 7, and 8 at 1, 5, and 10 min, respectively. Birth weight was 3056 g and head circumference 36.4 cm (90th percentile). The anterior fontanelle was normal in size (1.5 × 1.5 cm), tension free, and not pulsatile. He had no craniofacial dysmorphisms.
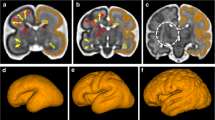
The first magnetic resonance imaging (MRI) scan at 0 days of age showed a huge midline mass composed of a conglomerated and infolded irregular microgyric cortex and white matter (Fig. 1). The mass extended from the left to the right hemisphere across the central part of the fissure and was continuous with the hemispheric cortex and thalamus, bilaterally. Inferiorly, the lesion protruded into the third ventricle. These findings suggested that the mass was a midline brain-in-brain malformation. MRI also revealed an azygos anterior cerebral artery and incomplete cleavage of the frontal cortex and thalamus, consistent with a diagnosis of lobar HPE. The lateral ventricles were enlarged, and the left posterior cortex was lined by a malformed cerebral mantle. Single voxel magnetic resonance spectroscopy acquired from the parenchyma of the abnormal midline mass demonstrated normal spectra for the N-acetyl group, choline, and creatine.
At 1 day of age, the patient underwent Ommaya reservoir implantation for hydrocephalus and the mass was biopsied. Total surgical treatment was not considered because of the mass location. Pathological examination of the specimen revealed normal neuroglial tissue representing heterotopic brain tissue. Cortical neurons lacked any apparent lamination. There was no cellular atypia or mitotic activity. Immunohistochemistry confirmed that the neurons moderately expressed neurofilament protein, whereas there was strong expression of glial fibrillary acidic protein in astrocytes (Fig. 2a–c). As a result, the malformation, which was thought to be a midline brain-in-brain malformation on imaging data, was considered to be a subcortical heterotopia.
Histopathological features on the second day of life. a Neurofilament high-power view. b Neurofilament low-power view. c Glial fibrillary acidic protein low-power view. Neurofilament immunostaining revealed normal appearance of the cortex and white matter. There are some negative glial fibrillary acidic protein cells suggestive of neurons
At 51 days of age, he underwent ventricular shunting for hydrocephalus. At age 4 months, the patient developed a seizure disorder characterized by predominant right clonic seizures. On interictal electroencephalographic (EEG) studies, frequent focal spikes were seen in the left parasagittal and temporal areas (Fig. 3a). The seizures were refractory to phenobarbital, zonisamide, valproic acid, clobazam, and levetiracetam. Subsequently, the patient never became seizure-free for more than a month. Repeated brain MRI studies at 4, 7, 14, and 24 months of age showed no enlargement of the mass and no progression of myelination in the mass. However, with maturity, focal signal changes and decreased cerebral perfusion became clear on brain imaging, suggestive of secondary glial degeneration. The EEG findings at 24 months of age became progressively more severe (Fig. 3b). The onset of myelination in the mass occurred around the same time as that of the white matter of the frontal lobe.
At 24 months of age, neurological examination confirmed severe global developmental delay, poor visual fixation and tracking, a mild right facial asymmetry, generalized hypotonia, and brisk deep tendon reflexes with sustained left ankle clonus. His head circumference was 44.7 cm, at the 95th percentile for age. His developmental quotient was 19 at 24 months of age according to the Enjoji method (analytical development test for infants by Enjoji).
MRI at 31 months of age showed more evidence of periventricular nodular heterotopia in the right lateral ventricle, and that a part of this lesion was emphasized with T2-weighted image suggesting gliosis (Fig. 4a). MR spectroscopy acquired from the parenchyma of the abnormal midline mass demonstrated normal N-acetyl group, choline, and creatine spectra (Fig. 4b). This lesion also showed decreased cerebral perfusion as measured by arterial-spin labeling MRI (Fig. 4c).
MRI analysis at 31 months of age. a Axial T2 weighted imaging. The mass showed no change in size. Other periventricular nodular heterotopias were present in the right lateral ventricle (arrow). b Magnetic resonance spectroscopy acquired from the parenchyma of the abnormal midline mass demonstrated normal N-acetyl group, choline, and creatine spectra. c The same lesion demonstrated a decrease of cerebral perfusion as measured by arterial-spin labeling MRI
Discussion
In the present case, we initially considered that the huge midline mass in the brain was a midline brain-in-brain malformation, as proposed by Widjaja et al. [2]. The diagnostic characteristics of a midline brain-in-brain malformation were a huge mass and location in the midline, complicated by HPE, and what looked like real brain tissue by MRI. Our case met all these features. However, histological evidence showed that this malformation was consistent with subcortical heterotopia.
Subcortical heterotopia is generally characterized by the presence of displaced islands of gray matter mislocated in the white matter beneath the cerebral cortex [5]. The neurons and glia cells are normal and not dysplastic. In the present case, the pathology obtained at birth showed normal and no dysplastic neurons and glial cells. Considering its location, this condition reflected a massive migration defect of cortical tissue, which caused huge islands of cortical brain tissue inside and underneath the normal cortical tissue of normal brain. Our MR spectroscopy findings of normal spectra for the N-acetyl group, choline, and creatine were also identical to that for subcortical heterotopia [6].
Our case also exhibited evidences of periventricular nodular heterotopia, which are malformations of cortical development that may result from premature arrest of neuronal migration from the germinal matrix in the wall of the lateral ventricle to the developing cerebral cortex [7]. Periventricular nodular heterotopia occurs in a small percentage of patients with HPE [8]. The comorbidity of both subcortical heterotopia and periventricular nodular heterotopia in our case suggests the potential for a common origin.
This malformation likely had its own focal epileptogenesis. Our patient developed severe epilepsy with the epileptic focus on the side of the mass where there were no dysplastic cells on histology at birth, while with maturity, MRI revealed the appearance of gliosis in the mass and decreased blood perfusion in the same region as the gliosis. Recurrent epilepsy has been reported to be associated with secondary reactive gliosis [9]. As a result of migration defect, the migrated tissue might begin to behave as a focus of epileptic activity and cause reactive gliosis.
In conclusion, our patient exhibited a huge subcortical heterotopia as a midline mass at birth, which required discrimination from a midline brain-in-brain malformation.
This study was approved by the institutional review board of Hokkaido Medical Center for Child Health and Rehabilitation.
References
Golden JA (1999) Towards a greater understanding of the pathogenesis of holoprosencephaly. Brain Dev 21:513–521
Widjaja E, Massimi L, Blaser S, Di Rocco C, Raybaud C (2007) Midline “brain in brain”: an unusual variant of holoprosencephaly with anterior prosomeric cortical dysplasia. Childs Nerv Syst 23:437–442
Valsecchi L, Cavoretto P, Di Piazza L, Smid M, Pontesilli S, Scotti R, Spagnolo D, Baldoli C (2009) Prenatal diagnosis by 3D ultrasound and MRI of an unusual malformation of cortical development with brain-in-brain appearance. J Clin Ultrasound 37:354–359
da Rocha AJ, Santana PJ, Maia AC (2012) Midline brain-in-brain malformation associated with bilateral perirolandic cortical abnormalities: an image review of this rare disorder. Pediatr Radiol 42:1523–1526
Meroni A, Galli C, Bramerio M, Tassi L, Colombo N, Cossu M, Lo Russo G, Garbelli R, Spreafico R (2009) Nodular heterotopia: a neuropathological study of 24 patients undergoing surgery for drug-resistant epilepsy. Epilepsia 50:116–124
Widjaja E, Griffiths PD, Wilkinson ID (2003) Proton MR spectroscopy of polymicrogyria and heterotopia. AJNR Am J Neuroradiol 24:2077–2081
Barth PG (1987) Disorders of neuronal migration. Can J Neurol Sci 14:1–16
Hahn JS, Barnes PD (2010) Neuroimaging advances in holoprosencephaly: refining the spectrum of the midline malformation. Am J Med Genet C Semin Med Genet 154c:120–132
Estrada FS, Hernandez VS, Lopez-Hernandez E, Corona-Morales AA, Solis H, Escobar A, Zhang L (2012) Glial activation in a pilocarpine rat model for epileptogenesis: a morphometric and quantitative analysis. Neurosci Lett 514:51–56
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukumura, S., Watanabe, T., Kimura, S. et al. Subcortical heterotopia appearing as huge midline mass in the newborn brain. Childs Nerv Syst 32, 377–380 (2016). https://doi.org/10.1007/s00381-015-2841-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2841-0