Abstract
Iliac artery angioplasty with stenting is an effective alternative treatment modality for aortoiliac occlusive diseases. Few randomized controlled trials have compared the efficacy and safety between self-expandable stent (SES) and balloon-expandable stent (BES) in atherosclerotic iliac artery disease. In this randomized, multicenter study, patients with common or external iliac artery occlusive disease were randomly assigned in a 1:1 ratio to either BES or SES. The primary end point was the 1-year clinical patency, defined as freedom from any surgical or percutaneous intervention due to restenosis of the target lesion after the index procedure. The secondary end point was a composite event from major adverse clinical events at 1 year. A total of 201 patients were enrolled from 17 major cardiovascular intervention centers in South Korea. The mean age of the enrolled patients was 66.8 ± 8.5 years and 86.2% of the participants were male. The frequency of critical limb ischemia was 15.4%, and the most common target lesion was in the common iliac artery (75.1%). As the primary end point, the 1-year clinical patency as primary end point was 99% in the BES group and 99% in the SES group (p > 0.99). The rate of repeat revascularization at 1 year was 7.8% in the BES group and 7.0% in the SES group (p = 0.985; confidence interval, 1.011 [0.341—2.995]). In our randomized study, the treatment of iliac artery occlusive disease with self-expandable versus balloon-expandable stent was comparable in 12-month clinical outcomes without differences in the procedural success or geographic miss rate regardless of the deployment method in the distal aortoiliac occlusive lesion (ClinicalTrials.gov, NCT01834495).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iliac artery angioplasty with stenting is a good alternative treatment for aortoiliac occlusive disease [1,2,3,4,5]. With the development of stenting and angioplasty techniques, more extensive and multifocal iliac lesions have been treated with endovascular procedures [6].
Low morbidity and mortality, along with a technical success rate up to 90%, support the use of endovascular-first approach. The patency rates achieved with iliac arteries stenting are comparable to those of surgical revascularization and show favorable outcomes. In experienced centers, Trans-Atlantic Inter-Society Consensus Document (TASC) D lesions may be considered [7,8,9].
Stents for iliac artery disease are classified as self-expandable stents (SES) and balloon-expandable stents (BES) according to the mechanics of stent deployment and as nitinol, stainless steel and others according to the stent material. Currently, the choice of balloons versus self-expandable stents is mainly determined by the operator’s preferences. Some indirect comparative studies and one randomized controlled trial (RCT) compared balloon-expandable or self-expandable stents [10,11,12]. In the above RCT, SES was better than BES in the 12-month restenosis rate and target lesion revascularization. However, most indirect comparative studies have shown similar patency between BES and SES.
Therefore, in this study, we compared the 1-year safety and efficacy between SES and BES in real-world clinical practice from expert Korean multicenter endovascular intervention centers using randomized clinical trials for a fair comparison [13]. In addition, we aimed to ascertain whether there were differences in the incidence of geographic misses, complications and procedural success rates between the two different stenting groups in aortoiliac steno-occlusive lesions.
Materials and methods
Study design
This was a prospective, multicenter, single blind, randomized, controlled trial to assess the efficacy and safety of iliac artery stents and previously published study protocol [13]. Consecutive patients with common or external iliac artery stenosis or occlusion were allocated in a 1:1 ratio to either SES (COMPLETE-SE™, Medtronic, USA) or BES (SCUBA™ Medtronic, USA). The trial was approved by the ethics committee. Written informed consent was obtained from all patients. This study complied with the Declaration of Helsinki and was registered at ClinicalTrials.gov (SENSE-ILIAC trial; NCT01834495). Patients were enrolled and followed up between March 2013 and January 2019. A brief flowchart of the study is shown in Fig. 1.
Study population
Patients at least 20 years of age with moderate or severe intermittent claudication or critical limb ischemia (CLI) or atypical symptom such as paresthesia, numbness, coldness, or Rutherford score of 0–6 were screened for study enrollment. Patients who had undergone or were planning to undergo major amputation were excluded. Before inclusion in the study, morphological examination, such as CT and MRI, was unnecessary. However, we usually recommend CT angiography prior to intervention. Patients were enrolled if they met all inclusion criteria and none of the exclusion criteria. The inclusion criteria were clinical and anatomical characteristics.
The clinical inclusion criteria were as follows: (1) symptomatic peripheral artery disease with moderate-to-severe claudication (Rutherford score of 2–3); (2) chronic CLI with resting ischemic pain (Rutherford score of 4); (3) chronic CLI with ischemic ulcers (Rutherford score of 5–6); and (4) patient must provide written informed consent. The anatomical inclusion criteria were as follows: (1) > 70% stenosis; (2) occlusion of the ipsilateral iliac artery; (3) patent (≤ 50% stenosis) ipsilateral femoropopliteal artery or concomitantly treatable ipsilateral femoropopliteal lesions (≤ 30% residual stenosis); and at least one patent (less than 50% stenosis) tibioperoneal runoff vessel. We did not exclude patients who underwent femoral endarterectomy. Patients were enrolled if inflow and outflow diseases were to be treated (except for bypass surgery).
The pre-defined study exclusion criteria are as follows: (1) failure to provide written informed consent; (2) a history of major bleeding within the prior 2 months; (3) known hypersensitivity or contraindication to any of the following medications: heparin, aspirin, clopidogrel, cilostazol, or contrast agent; (4) acute limb ischemia; (5) previous bypass surgery or stenting of the ipsilateral iliac artery; (6) untreated inflow disease of the distal aorta (> 50% stenosis or occlusion); (7) patients who have undergone major amputation (amputation of above the ankle) or major amputation is planned or required; (8) patients with a life expectancy of less than one year due to comorbidities.
Randomization and endovascular interventions
Aspirin and clopidogrel were administered at least 12 h before the procedure. Prior to endovascular treatment (EVT), 70–100 units/kg of unfractionated heparin was administered. EVT was performed percutaneously by placing a 6–8 Fr sheath in the femoral artery via an ipsilateral retrograde femoral approach or a contralateral crossover technique. A distal retrograde approach (from the distal superficial femoral artery, popliteal artery, or pedal arteries) and/or brachial approach was allowed in selected cases. Diagnostic angiography was performed in two different views at least 30–45° apart, to evaluate the structure of the target lesion. The femoro-popliteal and tibial arteries were examined visually for distal lesions. In cases of total occlusion, both intraluminal and subintimal recanalizations were allowed. After successful passing of the 018″ or 035″ guidewires, the target lesion was predilated with an optimally sized balloon before stent implantation. The balloon angioplasty results were considered suboptimal if there was a residual pressure gradient of ≥ 10 mmHg, or residual stenosis of ≥ 30%, or flow-limiting dissection. Subsequently, web-based randomization was performed for stent selection. According to the stent deployment method. Patients were randomly allocated to one of two groups, BES or SES. Patients were randomly allocated using a web-based computerized program separately managed at the Cardiovascular Intervention Research Institute (CIRI), Korea University Guro Hospital, Seoul, Republic of Korea. Patients were randomized in a 1:1 manner according to the two different stents (BES versus SES). The stents were implanted to extend 10 mm proximally and distally from the margins of the target lesion with a luminal narrowing of ≥ 50%. An appropriate stent size was selected after reviewing the baseline angiography results. If the stent was randomized to SES, a stent with a diameter 1–2 mm larger than that of the true vessel lumen was selected. However, if the stent was randomized to the BES group, a stent of equal size to the reference vessel diameter was selected to prevent iliac artery injury. Spot stenting or full lesion coverage was performed at the physician’s discretion. When multiple stents were required, the margins should overlap by at least 10 mm. Adjuvant post-dilation after stenting was performed strictly within the stented segment, with up to 10% oversizing of the post-dilation balloon.
All ipsilateral femoropopliteal arterial lesions should be treated concomitantly with angioplasty and/or stenting, and the residual stenosis should be less than 50%. The treatment of tibioperoneal lesions is recommended only in cases of CLI. There should exist at least one patent (< 50% stenosis) tibioperoneal runoff vessel with a good anterograde flow. Final angiography was performed after EVT in both groups, using the same angles and magnifications as the baseline angiograms. Technical success was defined as successful access, stent deployment, and less than 30% diameter residual stenosis after revascularization. For post-procedural medication, aspirin 100 mg and clopidogrel 75 mg were administered once daily for at least 12 months. Cilostazol was approved as third antiplatelet agent at the physician’s discretion. After enrollment and the index procedure, clinical follow-up was planned at 1, 6, and 12 months to evaluate the clinical outcomes and ankle–brachial index (ABI) score. In addition, all patients were recommended to undergo follow-up catheter angiography, CT angiography, or duplex ultrasound at 9–12 months, according to local clinical practice. The investigators were urged to follow up on the patients by office visits or telephone contact, as necessary. Patient’ adherence to the study drug and side effects were monitored at every outpatient visit.
Study end points
The primary end point was 1-year clinical patency, defined as freedom from any surgical or percutaneous intervention after the index procedure owing to restenosis of the target lesion on imaging modalities or worsened ischemic limb symptoms and signs. The primary end point was analyzed using imaging studies, such as invasive angiography, CT angiography, and Doppler sonography. However, the number of patients who completed the imaging study after 12 months was small. Therefore, we replaced the primary end point based on imaging studies with a clinical patency rate. The secondary end point was a major adverse limb event at one year, defined as the composite of death from any cause, any amputation, or repeat revascularization of the target lesion or target extremity. The other secondary end points were as follows: (1) geographic miss rate: geographic miss refers to stent deployment to any area of the vessel that was intended to be treat with a stent, but was not covered or protruded by stent jumping and/or elongation; (2) limb salvage rate free of above-the-ankle amputation; (3) repeated target lesion revascularization (TLR) rate; (4) repeated target extremity revascularization (TER) rate; and (5) ABI at 12 months.
Statistical analysis
For the sample size calculation, we referred to the 1-year patency rate of stents for iliac artery disease. Although patency definitions varied across trials, 1-year patency rates in aortoiliac lesions were approximately 90% on average in previous studies using SES [10, 12, 14]. In case of SCUBA stent, the 9-month patency rate for the SCUBA™ stent was 99.2% in the ACTIVE study—a prospective, multicenter, single-arm study that defines the midterm efficacy of a next-generation cobalt chromium iliac stent for the treatment of de novo and restenotic lesions in iliac arteries [15]. However, based on the other multicenter BES studies, including the MELODIE trial [11] and the European multicenter iliac stent trial [16], the one-year primary patency of the SCUBA™ stent is reasonably estimated to be 88%. Therefore, we hypothesized that the expected clinical patency rate at 1-year after stent deployment would be 90% for the SES group and 88% for BES group, respectively. The predetermined non-inferiority margin showed a δ 10% difference between the treatment groups. There is a clinical consensus that this non-inferiority margin would be acceptable if safety is maintained and patients are treated more easily, regardless of stent classification. Power analysis was based on the non-inferiority principle. The statistical significance level was 2.5% at one side, the power of the test was set at 80%, and the randomization ratio was set at 1:1. The test for proportion andChi-square method were used. Using a standard sample size formula, it was calculated that 120 patients per group were needed for a total of 288 patients, after accounting for a 20% dropout rate.
SPSS (version 20.0; SPSS Inc, Chicago, Illinois, USA was used for all analyses. Categorical variables will be expressed as delivery rates when comparing baseline features between the BES and SES groups and will be compared using the Chi-square or Fisher’s exact test. Continuous variables are expressed as mean ± standard deviation, and comparisons between groups were performed using Student’s t test. A P value < 0.025 was considered statistically significant.
Results
A total of 230 patients were enrolled at 17 cardiovascular intervention centers in South Korea and randomly assigned to undergo iliac artery angioplasty with either an SES or a BES stent (Fig. 1). Due to the stent supply problem of the manufacturer, the number of included patients fell slightly below the target sample size. Ultimately, 201 patients were included in the study.
The two stent groups were well matched at baseline concerning coexisting conditions and morbidities (Table 1). The most enrolled patients were male (89.1% in the BES vs. 87.0% in the SES, p = 0.645), and the mean age was 69.8 ± 9.3, 68.3 ± 9.4 in both groups, respectively. Hypertension and diabetes mellitus were observed in approximately 70% and 54% of the study population, respectively. In addition, there were no differences in laboratory findings or medications, including antiplatelet drugs, between the two groups.
The baseline lesions and procedural characteristics of the patients are listed in Table 2. The clinical presentations of the study participants were well balanced. The most prevalent Rutherford classification was severe claudication (31.8 vs 35.6%, respectively). The baseline mean ABI in the target limb was 0.65 ± 0.15 vs 0.68 ± 0.16 in both groups (p = 0.250). The lesion characteristics, including limb side, target lesion, and mean lumen stenosis, were similar.
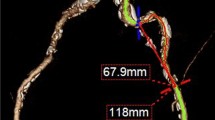
In the procedure, the mean stent diameter was 7.77 ± 0.94 mm in the BES group and 8.33 ± 0.96 mm in the SES group (p < 0.001) and the mean stent length was longer in the SES than in BES (78.4 ± 46.7 vs 56.6 ± 34.7 mm; p < 0.001), as expected. The two groups did not differ in the use of stents, use of drug coating balloon, and subintimal approach. However, additional balloons were used more frequently in the SES group than in the BES group for stent optimization (70.0 vs 27.7%, p < 0.001). The incidence of ‘geographic miss’ for the iliac ostial lesion was one of the interesting focuses of this study because it is known to be the main reason for using BES for the iliac ostial disease to minimize this geographic miss chance. Geographic miss occurred in only two patients (2.0%) in the BES group, but there was no significant difference between the groups (p = 0.498). The overall procedural success rates were 98.0% and 99.0%, respectively.
The incidences of the primary and secondary end points are shown in Table 3.
In short-term clinical outcomes at 7 days after EVT, there were no significant differences in the incidence of bleeding, death, or repeat revascularization between the groups.
The 1-year clinical patency were 99.0% and 99.0% in the BES and SES groups, respectively (p = > 0.999) (Table 3). There were no differences in the incidence of death, amputation, or major adverse cardiac events between the groups (Table 3). For the secondary end points, there was no difference in the incidence of limb salvage, repeat TLR, or repeat TER (Table 3). Ankle–brachial index at 12 months was similar between the two groups and improved compared with that measured at baseline (0.94 ± 0.16 vs 0.96 ± 0.17, p = 0.616) (Fig. 2, Table 4).
Discussion
Different strategies and types of stents are required when performing endovascular repair of iliac artery lesion. However, there is no general consensus on which balloon-expandable or self-expandable stents are the most appropriate for specific iliac artery lesions.
This randomized trial demonstrated that BES was non-inferior to SES for iliac artery occlusive disease in terms of any re-intervention or major adverse limb event rates. In addition, it is possible to deploy stents without geographic misses for aortoiliac bifurcation lesions irrespective of the stent deployment mechanism.
Previous studies have consistently demonstrated primary patency rates exceeding 90% at 12 months. Specifically, the primary patency rates for BES were found to be comparable to those of SES, with rates of 92.1% at 6 months and 87.8% at 2 years [11]. The previously mentioned randomized ICE trial that showed the cumulative incidence of binary restenosis at 12 months was 6.1% in the SES group and 14.9% in the BES group, as assessed by Doppler ultrasound, and the rates were similar [12]. We affirmed that clinical patency and major adverse limb events, including effectiveness and safety, could be accepted as primary end points in iliac artery disease interventions.
It is important to compare the geographic miss rate between the BES and SES in iliac artery lesions, particularly aortoiliac bifurcation lesions. In real-world clinical practice, physicians tend to use SES in the mid-iliac area due to severe angulation and tortuosity, to avoid potential iliac artery injury such as extravasation, dissection or rupture that could occur with high-pressure balloon inflation when using a longer BES. However, BES is recommended for accurate stent deployment, especially in bifurcation lesions involving the common iliac artery ostium, to minimize the risk of geographic miss that could lead to stent elongation or jumping during stent deployment. Such issue may contribute to stent fracture, in-stent restenosis, and contralateral artery flow limitation in contralateral artery flow [8]. In our study, > 15% of iliac ostial lesions were considered, and both stents were safely deployed in the bifurcation and the iliac artery ostium. Therefore, our results suggest that stents can be used for iliac artery disease irrespective of the stent deployment method.
This study had some limitations. First, patients were not enrolled as planned because of the manufacturer’s stent supply problem. However, the enrolled patient population achieved 87% of the target number, comparable to previous studies. Anyway, the overall study population was relatively small. So the results statistically showed wide confidence interval. Further randomized investigation with a larger population is required in the future. Second, imaging studies, such as invasive angiography, CT angiography, or Doppler ultrasound were not used as primary outcome, potentially contributing to bias. Imaging remains the gold standard for assessing primary patency after PTA. Instead, we used the ABI, which was powered to detect a difference in patency at 12 months, although it had limited power to detect differences in the precise restenosis rate. Third, none of the operators were blinded to the angiographic findings. Therefore, some complex lesions were not included in this study. However, this is not helpful in most randomized percutaneous interventional trials. Fourth, the clinical follow-up duration was only 1 year. We need to observe and analyze the results over a longer follow-up period.
In conclusion, the SENSE-ILIAC trial showed that treating iliac artery occlusive disease with either self- or balloon-expandable stents was similar in 12-month clinical outcomes without a difference in the incidence of geographic miss. Regardless of the deployment method and stent type, the current endovascular treatment for iliac artery disease showed good 12-month safety and efficacy.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Kudo T, Chandra FA, Ahn SS (2005) The effectiveness of percutaneous transluminal angioplasty for the treatment of critical limb ischemia: a 10-year experience. J Vasc Surg 41:423–435
Timaran CH, Prault TL, Stevens SL, Freeman MB, Goldman MH (2003) Iliac artery stenting versus surgical reconstruction for TASC (TransAtlantic Inter-Society Consensus) type B and type C iliac lesions. J Vasc Surg 38:272–278
Schürmann K, Mahnken A, Meyer J, Haage P, Chalabi K, Peters I, Günther RW, Vorwerk D (2002) Long-term results 10 years after iliac arterial stent placement. Radiology 224:731–738
Murphy TP, Ariaratnam NS, Carney WI Jr, Marcaccio EJ, Slaiby JM, Soares GM, Kim HM (2004) Aortoiliac insufficiency: long-term experience with stent placement for treatment. Radiology 231:243–249
Klein WM, van der Graaf Y, Seegers J, Spithoven JH, Buskens E, van Baal JG, Buth J, Moll FL, Overtoom TT, van Sambeek MR, Mali WP (2006) Dutch iliac stent trial: long-term results in patients randomized for primary or selective stent placement. Radiology 238:734–744
Bosch JL, Hunink MG (1997) Meta-analysis of the results of percutaneous transluminal angioplasty and stent placement for aortoiliac occlusive disease. Radiology 204:87–96
Kashyap VS, Pavkov ML, Bena JF, Sarac TP, O’Hara PJ, Lyden SP, Clair DG (2008) The management of severe aortoiliac occlusive disease: endovascular therapy rivals open reconstruction. J Vasc Surg 48:1451–1457
Tendera M, Aboyans V, Bartelink ML, Baumgartner I, Clément D, Collet JP, Cremonesi A, De Carlo M, Erbel R, Fowkes FG, Heras M, Kownator S, Minar E, Ostergren J, Poldermans D, Riambau V, Roffi M, Röther J, Sievert H, van Sambeek M, Zeller T (2011) ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J 32:2851–2906
Ichihashi S, Higashiura W, Itoh H, Sakaguchi S, Nishimine K, Kichikawa K (2011) Long-term outcomes for systematic primary stent placement in complex iliac artery occlusive disease classified according to Trans-Atlantic Inter-Society Consensus (TASC)-II. J Vasc Surg 53:992–999
Ponec D, Jaff MR, Swischuk J, Feiring A, Laird J, Mehra M, Popma JJ, Donohoe D, Firth B, Keim E, Snead D (2004) The nitinol SMART stent vs Wallstent for suboptimal iliac artery angioplasty: CRISP-US trial results. J Vasc Interv Radiol 15:911–918
Stockx L, Poncyljusz W, Krzanowski M, Schroë H, Allocco DJ, Dawkins KD (2010) Express LD vascular stent in the treatment of iliac artery lesions: 24-month results from the MELODIE trial. J Endovasc Ther 17:633–641
Krankenberg H, Zeller T, Ingwersen M, Schmalstieg J, Gissler HM, Nikol S, Baumgartner I, Diehm N, Nickling E, Müller-Hülsbeck S, Schmiedel R, Torsello G, Hochholzer W, Stelzner C, Brechtel K, Ito W, Kickuth R, Blessing E, Thieme M, Nakonieczny J, Nolte T, Gareis R, Boden H, Sixt S (2017) Self-expanding versus balloon-expandable stents for iliac artery occlusive disease: the randomized ICE trial. JACC Cardiovasc Interv 10:1694–1704
Choi WG, Rha SW, Choi CU, Kim EJ, Oh DJ, Cho YH, Park SH, Lee SJ, Hur AY, Ko YG, Park SM, Kim KC, Kim JH, Kim MW, Kim SM, Bae JH, Bong JM, Kang WY, Seo JB, Jung WY, Cho JH, Kim Do H, Ahn JH, Kim SH, Jang JY (2016) Study design and rationale of the “Balloon-Expandable Cobalt Chromium SCUBA Stent versus Self-Expandable COMPLETE-SE Nitinol Stent for the Atherosclerotic ILIAC Arterial Disease (SENS-ILIAC Trial) Trial”: study protocol for a randomized controlled trial. Trials 17:302–312
Faries P, Jaff M, Peeters P, Khatib Y, Roberts D, Bosiers B, Malik R, Ravin R, Rundback J (2018) Nine-month outcomes of the DURABILITY iliac study on self-expanding stents for symptomatic peripheral artery disease. Ann Vasc Surg 51:37–47
Molnar RG, Gray WA (2013) Sustained patency and clinical improvement following treatment of atherosclerotic iliac artery disease using the Assurant cobalt iliac balloon-expandable stent system. J Endovasc Ther 20:94–103
Reekers JA, Vorwerk D, Rousseau H, Sapoval MR, Gaines PA, Stockx L, Delcour CP, Raat H, Voshage G, Biamino G, Hoogeveen YL (2002) Results of a European multicentre iliac stent trial with a flexible balloon expandable stent. Eur J Vasc Endovasc Surg 24:511–515
Funding
This study was supported by a grant from the Medtronic Company, Korea. No funder/sponsor had any role in the following: design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choi, W.G., Rha, SW., Choi, B.G. et al. Balloon-expandable cobalt chromium stent versus self-expandable nitinol stent for the Atherosclerotic Iliac Arterial Disease (SENS-ILIAC Trial) Trial: a randomized controlled trial. Heart Vessels (2024). https://doi.org/10.1007/s00380-024-02431-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00380-024-02431-4