Abstract
Elevation of the head and expiratory negative airway pressure (ENAP) ventilation can both significantly alter cardiovascular hemodynamics. The impact of head-up tilt (HUT) position on mechanically regulated ENAP ventilation-induced hemodynamics was assessed in microminipigs under halothane anesthesia (n = 4) in the absence and presence of adrenergic blockade. Supine ENAP ventilation increased cardiac output, but decreased mean right atrial, systolic pulmonary arterial, and mean left atrial pressures without significantly altering heart rate or aortic pressure. With HUT, the magnitude of ENAP ventilation-induced reduction in right and left atrial pressures was attenuated. HUT minimally altered ENAP ventilation-induced increase in cardiac output and reduction in pulmonary arterial systolic pressure. In addition, with up to 10 cm of HUT there was a significant increase in mean right atrial pressure with and without the ENAP ventilation, whereas HUT did not alter the other hemodynamic variables irrespective of ENAP ventilation. These observations suggest that head elevation augments venous return from the brain irrespective of the ENAP ventilation. Additional studies with pharmacological adrenergic blockade revealed that ENAP ventilation-induced increases in cardiac output and decreases in pulmonary systolic pressure were minimally altered by sympathetic nerve activity, irrespective of the head position. However, the observed ENAP ventilation-induced decreases in right and left atrial pressures were largely dependent upon adrenergic activity. These experimental findings may provide insight into future clinical application of HUT and ENAP for patients with head injury and hypotension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The impact of mechanically regulated, expiratory negative airway pressure (ENAP) ventilation has been studied in different pathologic states in porcine models including cardiac arrest [1,2,3], hemorrhagic hypovolemic shock [4, 5], and head injury [6], as well as in patients [7,8,9,10,11,12]. In a recent study using anesthetized microminipigs [13], ENAP ventilation significantly increased the heart rate and cardiac output, but decreased the mean right atrial pressure (RAP), systolic pulmonary arterial pressure (PAP) and mean pulmonary capillary wedge pressure (PCWP), partly through an interaction with the sympathetic nervous system. These findings suggested a potential mechanical means to normalize ventricular filling pressures and to restore adequate tissue perfusion during acute heart failure. Indeed, in a pilot study using microminipigs, ENAP ventilation fully restored the cardio-hemodynamic collapse induced by an excessive dose of selective serotonin reuptake inhibitor fluvoxamine [13], which has negative chronotropic, inotropic and dromotropic effects and can cause hypotension [14].
Cardiopulmonary resuscitation (CPR) with head-up tilt (HUT) position can improve the outcomes of patients with out-of-hospital cardiac arrest, since it can enhance the venous return from cerebral circulation and decrease intracranial pressure, thereby increasing cerebral forward blood flow and improving neurological intact survival [15,16,17,18,19]. Similar hemodynamic benefits to those observed with HUT during CPR may accrue in patients with acute heart failure presenting with orthopnea. The efficacy of the orthopneic position in acute heart failure is generally considered to depend on the decrease in venous return from the lower extremities when patients sleep propped up in bed or sit in a chair [20]. In addition to those putative hemodynamic mechanisms, the HUT procedure by itself could be expected to reduce the stretch of arterial vessel wall around the carotid baroreceptor, which might trigger the autonomic baroreflex and disinhibit the sympathetic discharge [21].
Both the ENAP ventilation and the HUT position can be used as therapeutic interventions as mechanical provocateurs. The combination of these interventions may become an efficacious strategy for treating patients with acute heart failure; however, it is not known how the HUT procedure may affect the impact of ENAP ventilation-induced hemodynamic responses. Thus, the purpose of this study was to assess the effects of the HUT position on the pulmonary and systemic circulation, with and without ENAP ventilation under the physiologically controlled conditions. Further assessment was performed after the pharmacological adrenoceptor blockade to examine if the potential effects of these two mechanical interventions were altered by sympathetic nerve activity [13]. Studies were performed with anesthetized microminipigs that are non-rodent experimental animals optimized for life science research [22].
Methods
Experiments were performed in four male microminipigs (Fuji Micra Inc., Shizuoka, Japan) weighing approximately 10 kg. The animals were individually housed in stainless steel cages on a 12 h light (6:00–18:00)–dark (18:00–6:00) cycle, and were given 200 g/day of standard pellet diet (MMP pellets, Marubeni Nisshin Feed Co. Ltd., Tokyo, Japan) and free access to tap water. The animal rooms were maintained at a temperature of 23 ± 2 °C and a relative humidity of 50 ± 20%. All experiments were approved by the Toho University Animal Care and User Committee (No. 18-51-394) and performed in accordance with the Guidelines for the Care and Use of Laboratory Animals of Toho University.
Induction of general anesthesia
Microminipigs were pre-anesthetized with an intramuscular injection of ketamine (16 mg/kg) and xylazine (1.6 mg/kg) [13]. A 24G cannula was introduced into a superficial auricular vein for anesthetic injection of 1 mg/kg of propofol. Then, the animal was positioned supine. After intubation with a 6-mm cuffed endotracheal tube, anesthesia was maintained by inhalation of halothane (1% v/v) vaporized in oxygen with a volume-limited ventilator (SN-480-3; Shinano Manufacturing Co., Ltd., Tokyo, Japan). Tidal volume and respiratory rate were set at 10 mL/kg and 15 breaths/min, respectively.
Surgical preparations
Two 6 F-size catheter sheaths (FAST-CATH™ 406104; St. Jude Medical, Daig Division, Inc., Minnetonka, MN, USA) were used; one was inserted into the right femoral artery toward aorta, and the other was done into the right femoral vein toward inferior vena cava. Heparin calcium (100 IU/kg) was administered to prevent the blood clotting through a flush line of the catheter sheath placed at the right femoral vein. A 5 F-size catheter was inserted into the aorta through the catheter sheath placed at the right femoral artery, tip of which was positioned at a level of diaphragm to measure the aortic blood pressure. A triple lumen thermodilution balloon catheter (132F5; Edwards Lifesciences, Irvine, CA, USA) was inserted into the right side of the heart through the catheter sheath placed at the right femoral vein to measure the RAP, PAP, PCWP and cardiac output. The cardiac output was measured using a standard thermodilution method with a cardiac output computer (MFC-1100; Nihon Kohden Corporation, Tokyo, Japan). Pulmonary vascular resistance (PVR) was calculated using the mean pulmonary arterial pressure, cardiac output and PCWP with the following equation: PVR = (mean pulmonary arterial pressure − PCWP)/cardiac output. The electrocardiogram was obtained from the A–B lead. The electrocardiogram and cardio-hemodynamic variables were continuously monitored with a polygraph system (RM-6000; Nihon Kohden Corporation).
Preparation of ENAP circuit
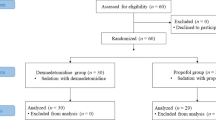
The intra-tracheal airway pressure was estimated using the pressure transducer, which was placed between the endotracheal tube and the exhaust port of the ventilator, as previously described [13]. The ENAP generation system consists of an exhaust port, a T-shaped pipe with a custom-made, one-way impedance threshold valve (ITV) with a cracking pressure of − 25 cmH2O (Resusci-valve ITV™, CPRx LLC, Minneapolis, MN, USA), and an aspirator as a vacuum source (DAS-01, AS ONE Corporation, Osaka, Japan), which were connected with plastic tubes in series as previously described [13]. When the ITV is inactivated and the ENAP is turned off (ENAP OFF), there is bidirectional airflow without resistance. Thus, the pressure within the ENAP circuit was kept at the atmospheric air pressure during both expiratory and inspiratory phases, and the standard intra-tracheal airway pressure was provided by artificial ventilation to the animals (Fig. 1, top). When the ITV was activated (ENAP ON), the negative pressure gradually increased within the ENAP circuit toward − 25 cmH2O by the aspirator, since the ITV did not bypass the airflow. When the negative pressure exceeded − 25 cmH2O (< − 25 cmH2O), the threshold valve of the ITV automatically opened, keeping the pressure in the ENAP circuit below or equal to − 25 cmH2O (≥ − 25 cmH2O). During the expiratory phase, the tidal volume of expiratory gas from the animal was drawn to the ENAP circuit. The intra-tracheal airway pressure became more negative during expiratory phase by the aspirator (Fig. 1, bottom), since the ITV functioned to impede the airflow into the ENAP circuit. During the next inspiratory phase, the exhaust port was closed, so that the generator system could create up to − 25 cmH2O of negative pressure.
Typical tracings of intra-tracheal pressure at a supine position without (top) and with (bottom) the expiratory negative airway pressure (ENAP) ventilation. Note that the airway pressure was kept at zero during the expiratory phase when the ENAP ventilation was not used (ENAP OFF), whereas it became negative during the expiratory phase when the ENAP ventilation was used (ENAP ON)
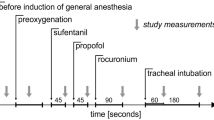
Head-up tilt
Microminipigs were positioned supine. As shown in Fig. 2, the upper half of the body, including the head and thorax, was positioned in three different angles; namely, the upper half of the body was kept in the horizontal recumbent position with head-up tilt of 0 cm (HUT0, 0°), and that was raised up from the operating table by inserting the blocks of styrofoam behind the head attaining head-up tilt of 5 cm (HUT5, about 15°) and head-up tilt of 10 cm (HUT10, about 30°) based on a previous report [15], which was different from reverse-Trendelenburg position.
Schematic diagram of surgical preparations and head-up tilt (HUT) procedure. Hemodynamic variables were measured in three HUT positions, in which head of the animal was kept at 0 cm level (HUT0, top), and raised up to 5 cm level (HUT5, bottom left) and to 10 cm level (HUT10, bottom right) from the operating table. ENAP expiratory negative airway pressure, ECG electrocardiogram, AoP aortic blood pressure, RAP mean right atrial pressure, PAP systolic pulmonary arterial pressure, PCWP mean pulmonary capillary wedge pressure, CO cardiac output
Experimental protocol
Effects of HUT procedure on the ENAP ventilation-induced hemodynamic responses were assessed in the absence and presence of the adrenergic blockade. After confirming the stability of the hemodynamic condition with the animal in the HUT0 position, the intra-tracheal airway pressure was measured without the ENAP ventilation at the end of the expiratory phases during successive three respiratory cycles. Also, to minimize scattering in each of the hemodynamic values, we measured the heart rate, systolic/diastolic aortic blood pressure, RAP, PAP and PCWP using the last beat during the expiratory phase in a similar manner to that of intra-tracheal airway pressure. The cardiac output was measured three times irrespective of the respiratory phases, since about 10 s were needed to calculate the cardiac output, which was 2.5 times longer than the 4 s respiratory cycle. Next, the ENAP ventilation was started, and after 1 min to allow for its full mechanical effect, measurements similar to those made with ENAP OFF were performed. Next, the same set of measurements, without and with the ENAP ON ventilation, was repeated in the HUT5 and HUT10 positions. Then, 1 mg/kg of phentolamine and 0.3 mg/kg of propranolol were intravenously administered to pharmacologically block the sympathetic nerve. After 1 min to allow for their full pharmacological effect, noradrenaline (0.3 μg/kg) and isoproterenol (0.03 μg/kg) were intravenously administered to confirm α- and β-adrenoceptor blockade, respectively, as previously described [13]. After confirming that the maximum elevations of the mean blood pressure and heart rate by noradrenaline and isoproterenol were < 10 mmHg and < 10 bpm, respectively, each hemodynamic variable was recorded without and with the ENAP ventilation in the same manner in the HUT0, HUT5 and HUT10 positions, respectively, as those before the adrenergic blockade. After the termination of experiment, the catheter sheaths were removed, the animals were allowed to recover, and a physical examination of the animals was performed daily for 1 week thereafter.
Drugs
Phentolamine (Regitin® inj, Novartis Pharma K.K., Tokyo, Japan) was diluted with saline to a concentration of 3.33 mg/mL. Propranolol (Inderal® inj, AstraZeneca K.K., Osaka, Japan), isoproterenol (Proternol-L inj, Kowa Company, Ltd., Nagoya, Japan), noradrenaline (Nor-adrenalin inj, Daiichi Sankyo Co., Ltd., Tokyo, Japan), ketamine (Ketalar®, Daiichi Sankyo Co., Ltd.), xylazine (Celactal®, Bayer Healthcare Co., Tokyo, Japan), propofol (propofol inj [FK], Fresenius Kabi Japan K.K., Tokyo, Japan), halothane (Fluothane®, Takeda Pharmaceutical Co., Ltd., Osaka, Japan) and heparin calcium (Caprocin®, Sawai Pharmaceutical Co., Ltd., Osaka, Japan) were purchased.
Statistical analysis
Data are presented as mean ± SEM (n = 4). We used three data points for each pig to compare the hemodynamics between the HUT interventions. The statistical significances within a parameter were evaluated by two-way, repeated measures analysis of variance (ANOVA) followed by Fisher’s LSD test. Hemodynamic parameters with the HUT0 position, between before and after the pharmacological adrenoceptor blockade, were assessed by paired t test. A p value < 0.05 was considered to be statistically significant.
Results
During this study, there were no cases of hemodynamic collapse leading to death. Furthermore, there was no evidence of respiratory distress, obvious lung pathology or neurological deficit up to 1 week after the experiment.
Effects of HUT positioning on the ENAP ventilation-induced hemodynamic responses before the adrenergic denervation
Typical tracings of intra-tracheal pressure without and with the ENAP ventilation in the HUT0 position before the adrenergic denervation are depicted in Fig. 1. The intra-tracheal pressure at the end-expiratory phase in the HUT0, HUT5 and HUT10 positions, without the ENAP ventilation were − 0.2 ± 0.3, − 0.1 ± 0.5 and − 0.1 ± 0.7 cmH2O, respectively, and with the ENAP ventilation, they were − 14.9 ± 3.4, − 12.4 ± 1.0 and − 13.9 ± 2.2 cmH2O, respectively (not shown in the figure). No significant difference was observed in these intra-tracheal pressures among the HUT0, HUT5 and HUT10 positioning, indicating that the HUT procedure did not affect the intra-tracheal pressure during the end-expiratory phase, without or with the ENAP ventilation. In addition, the PVR in the absence and presence of ENAP ventilation was 4.8 ± 0.6 and 5.0 ± 0.5 mmHg/L/min in the HUT0, 4.7 ± 0.8 and 5.0 ± 0.7 mmHg/L/min in the HUT5, and 5.1 ± 0.9 and 3.8 ± 0.6 mmHg/L/min in the HUT10, respectively (not shown in the figure). No significant difference was detected in these PVR values with ENAP OFF versus ENAP ON ventilation, indicating that the ENAP ventilation hardly altered the PVR.
The effect of the different HUT positions on the ENAP ventilation-induced hemodynamic responses are summarized in Fig. 3. The heart rate, systolic/diastolic aortic blood pressure, cardiac output, RAP, PAP and PCWP at the HUT0 position without the ENAP ventilation were 54 ± 2 bpm, 95 ± 3/62 ± 3 mmHg, 1.22 ± 0.10 L/min, 8.7 ± 0.8 mmHg, 22.3 ± 0.9 mmHg, and 11.0 ± 0.9 mmHg (Fig. 3, blue circles), respectively, whereas those with the ENAP ventilation were 56 ± 2 bpm, 98 ± 4/65 ± 3 mmHg, 1.41 ± 0.10 L/min, 7.4 ± 0.8 mmHg, 20.4 ± 0.8 mmHg and 8.7 ± 1.2 mmHg (Fig. 3, red squares), respectively. The HUT procedure increased the RAP with the HUT10 position compared with that at HUT0 in the absence and presence of the ENAP ventilation. There were no significant changes observed in the other hemodynamic variables with the HUT10 positioning. Significant differences with ENAP OFF versus ENAP ON ventilation were observed in cardiac output with the HUT0, HUT5 and HUT10 positions, RAP with the HUT0 and HUT5 positions, PAP at the HUT0, HUT5 and HUT10 positions, and PCWP at the HUT0 and HUT5 positions. No other significant differences were observed.
Summary of effects of head-up tilt (HUT) procedure on the hemodynamic variables without (ENAP OFF) and with (ENAP ON) the expiratory negative airway pressure (ENAP) ventilation before the pharmacological adrenergic denervation. Note that the ENAP ventilation-induced decrease in the RAP and PCWP was observed at HUT0 and HUT5, but not at HUT10. Heart rate (HR), systolic/diastolic (SBP/DBP) aortic blood pressure (AoP), cardiac output (CO), mean right atrial pressure (RAP), systolic pulmonary arterial pressure (PAP) and mean pulmonary capillary wedge pressure (PCWP) without (blue circles) and with (red squares) the ENAP ventilation were shown along with actual values. Data are presented as mean ± SEM (n = 4). *p < 0.05, and **p < 0.01
Effects of HUT positioning on the ENAP ventilation-induced hemodynamic responses after the adrenergic denervation
After administration of phentolamine and propranolol, the maximum increases in the mean arterial pressure and heart rate with noradrenaline and isoproterenol were < 10 mmHg and < 10 bpm, respectively. The intra-tracheal pressures at the end-expiratory phase of the HUT0, HUT5 and HUT10 positions, without the ENAP ventilation, were − 0.3 ± 0.5, − 0.2 ± 0.5 and − 0.6 ± 0.4 cmH2O, and with the ENAP ventilation they were − 15.5 ± 3.2, − 15.0 ± 3.3 and − 15.7 ± 3.6 cmH2O, respectively (not shown in the figure). No significant difference was observed in these intra-tracheal pressures among the HUT0, HUT5 and HUT10 positioning, indicating that the HUT procedure did not affect the intra-tracheal pressures during the end-expiratory phase, without or with the ENAP ventilation in the absence of the sympathetic nerve activity. In addition, the PVR in the absence and presence of ENAP ventilation was 7.1 ± 2.0 and 5.9 ± 1.3 mmHg/L/min in the HUT0, 6.0 ± 1.0 and 4.6 ± 0.7 mmHg/L/min in the HUT5, and 5.3 ± 0.8 and 4.2 ± 0.8 mmHg/L/min in the HUT10, respectively (not shown in the figure). No significant difference was detected in these PVR values with ENAP OFF versus ENAP ON ventilation, indicating that the ENAP ventilation hardly altered the PVR.
The effects of the different HUT positions on the ENAP ventilation-induced hemodynamic responses are summarized in Fig. 4. The heart rate, systolic/diastolic aortic blood pressure, cardiac output, RAP, PAP and PCWP at the HUT0 position without the ENAP ventilation were 59 ± 3 bpm, 91 ± 3/63 ± 2 mmHg, 1.26 ± 0.07 L/min, 7.8 ± 0.5 mmHg, 24.7 ± 2.5 mmHg, and 10.7 ± 1.0 mmHg (Fig. 4, blue circles), respectively, whereas those with the ENAP ventilation were 58 ± 2 bpm, 95 ± 2/63 ± 2 mmHg, 1.40 ± 0.09 L/min, 7.1 ± 0.9 mmHg, 22.7 ± 2.2 mmHg, and 9.7 ± 0.5 mmHg (Fig. 4, red squares), respectively. No significant differences were observed in any of the hemodynamic parameter assessed with the HUT 0 position between before and after the pharmacological adrenoceptor blockade. RAP was higher in the HUT5 and HUT10 positions compared with the HUT0 position, without and with the ENAP ventilation, whereas no significant changes were detected in the other hemodynamic variables. Significant differences between without and with the ENAP ventilation were detected in the cardiac output and PAP in the HUT0, HUT5 and HUT10 positions, whereas no significant differences were detected in the other variables.
Summary of effects of head-up tilt (HUT) procedure on the hemodynamic variables without (ENAP OFF) and with (ENAP ON) the expiratory negative airway pressure (ENAP) ventilation after the pharmacological adrenergic denervation. Note that the ENAP ventilation-induced decrease in the RAP or PCWP was not observed at any HUT position. Heart rate (HR), systolic/diastolic (SBP/DBP) aortic blood pressure (AoP), cardiac output (CO), mean right atrial pressure (RAP), systolic pulmonary arterial pressure (PAP), and mean pulmonary capillary wedge pressure (PCWP) without (blue circles) and with (red squares) the ENAP ventilation were shown along with actual values. Data are presented as mean ± SEM (n = 4). **p < 0.01
Discussion
Similar to taking a deep breath, the ENAP ventilation enhances venous blood flow back to the heart, lowers the RAP and PAP and increases the cardiac output as well as arterial pressures [23]. This study assessed how the cardiovascular effects of ENAP ventilation [13] might be modified by the HUT position, which also lowers intracranial pressure and increases venous blood flow from the brain to the heart. The results demonstrated that placement of the heart in the HUT position attenuated the magnitude of the ENAP ventilation-induced reduction in the RAP and PCWP, but had no significant effect on ENAP ventilation-induced changes in the cardiac output or PAP. In addition, the potential role of the autonomic nervous system in helping to modulate ENAP-induced changes in hemodynamics was also investigated.
Effects of HUT position on each hemodynamic variable
Before adrenergic blockade (Fig. 3), the HUT10 position increased the RAP compared with the HUT0 position, both without and with the ENAP ventilation. There were no other significant changes in the other hemodynamic variables with the combination of HUT positioning. The results suggest that the HUT position may have increased the venous return from cerebral circulation to the heart, independently of the intrathoracic pressure, resulting in the elevation of preload to the right ventricle in the intact animals. The effect of HUT positioning on the RAP was augmented after the adrenergic blockade (Fig. 4); HUT positioning further increased the RAP with HUT5 and HUT10 positions, in the presence of adrenergic blockade, without and with the ENAP ventilation. The new observations indicate that the effects of HUT positioning on the RAP are negatively regulated by the sympathetic nervous system. RAP is increased with HUT positioning, likely due to the effects of gravity on venous return to the heart. One can speculate that adrenergic blockade may have reduced α1 and ß2 receptor-mediated venous compliance [24, 25], thereby further increasing the RAP during HUT.
It is noteworthy that HUT positioning did not alter the cardiac output or systemic blood pressure, without or with the ENAP ventilation, independently of the adrenergic blockade. The results demonstrate that the HUT-induced enhancement of the venous return did not alter the magnitude of orthodromic blood flow under the experimental conditions used. This observation suggests that the increase of venous return from the cerebral circulation may be counterbalanced by other factors, perhaps a decrease of venous return from the lower extremities of the body.
Effects of HUT positioning on ENAP ventilation-induced changes in hemodynamics
In the absence of adrenergic blockade (Fig. 3), ENAP ventilation increased the cardiac output in the HUT0, HUT5 and HUT10 positions, but decreased the RAP and PCWP in the HUT0 and HUT5 positions, as well as the PAP with the HUT0, HUT5 and HUT10 positions. The heart rate and aortic blood pressure were unaltered by ENAP at any of the HUT positioning. After the adrenergic blockade, ENAP ventilation-induced hemodynamic responses were blunted at each of the HUT positioning, except for the PAP (Fig. 4). Thus, the effects of total adrenergic blockade were similar to our previous observations performed at supine and flat position [13], which support the reproducibility and validity of the current results.
ENAP ventilation-induced reductions in the RAP and PCWP were no longer observed after adrenergic blockade at any of the HUT positioning. These results can also be explained by the hypothesis that adrenergic blockade may have decreased the relaxation reserve or compliance of the central veins and potentially of the pulmonary vein and/or left ventricle as well. Importantly, these findings demonstrate for the first time the regulatory effects of the adrenergic nervous system on ENAP-induced changes in the RAP and PCWP during HUT positioning. However, these putative regulatory effects appear to be saturated at some point as ENAP ventilation-induced impact did not lead to a reduction in the RAP or PCWP with HUT10 positioning, before or after adrenergic blockade (Figs. 3 and 4). Thus, although HUT10 positioning can trigger an autonomic baroreflex response, the increase of venous return from the cerebral circulation may have overcome the reflex-mediated contractile response of the veins and depleted their potential central venous relaxation reserve, resulting in a decrease of venous compliance, which may partly explain these findings. Furthermore, HUT positioning did not alter the magnitude of the ENAP ventilation-induced increase of the cardiac output or decrease of the PAP before or after the adrenergic blockade, indicating these effects may not be significantly associated with sympathetic nerve activity.
Study limitations
First, the results were obtained with normal intact animals that might not necessarily reflect those pathological conditions where HUT and ENAP may be of clinical value, such as shock, brain injury heart failure, and cardiac arrest. In each of these disease states, cerebral circulation as well as systemic circulation can be compromised and potentially helped with ENAP and HUT positioning [1,2,3,4,5,6,7,8,9,10,11,12,13, 15,16,17,18,19,20,21]. Second, the current results obtained from four animals are suggestive, but the findings would be far from conclusive; thus, a larger sample size will be required to establish those proposed hypotheses under different pathological conditions. Third, although we measured the intra-tracheal airway pressure to estimate the intrathoracic one, we need to recognize that true intrathoracic pressure was not necessarily obtained in this study. Fourth, acute lung injury was not observed in this study; however, pulmonary safety profile with the long-term use of ENAP ventilation remains elusive. It should be noted that ENAP ventilation may not be able to be used for patients with lung injury, since the use of intrathoracic pressure regulator inducing ENAP ventilation was shown to compromise pulmonary function without significantly improving hemodynamic variables in a porcine polytrauma model of hemorrhagic shock and acute lung injury [26]. Fifth, the current study did not address the potential roles of different α and ß-adrenoceptor subtypes that might impact the effect of ENAP ventilation and HUT positioning on the RAP and PCWP. Sixth, the PVR was hardly altered by ENAP ventilation in the absence or presence of adrenergic blockade, indicating that currently applied magnitude of negative airway pressure may minimally affect the pulmonary circulation. However, safety margin of the magnitude of ENAP ventilation needs to be determined.
Conclusion
Although either ENAP ventilation or HUT positioning alone enhanced the venous return from cerebral circulation, the effects of the interventions together on the RAP and PCWP appear to be somewhat opposite. Addition of HUT positioning did not enhance the magnitude of the ENAP ventilation-induced increases in the cardiac output or decreases in the PAP in the intact animals, but ENAP ventilation-induced decreases in RAP and PCWP were attenuated by the HUT procedure. These findings suggest that the two interventions combined may have saturated the venous capacitance reserve. Pharmacological analysis suggests that the ENAP ventilation-induced increases in the cardiac output and decreases in the PAP are minimally, if at all, altered by sympathetic nerve activity. In contrast, ENAP ventilation-induced decreases in the RAP and PCWP may be largely depend on the sympathetic tone and innervation. These experimental findings may have implications related to the use of HUT positioning and ENAP ventilation in a range of potential clinical applications.
References
Yannopoulos D, Nadkarni VM, McKnite SH, Rao A, Kruger K, Metzger A, Benditt DG, Lurie KG (2005) Intrathoracic pressure regulator during continuous-chest-compression advanced cardiac resuscitation improves vital organ perfusion pressures in a porcine model of cardiac arrest. Circulation 112:803–811
Kwon Y, Debaty G, Puertas L, Metzger A, Rees J, McKnite S, Yannopoulos D, Lurie K (2015) Effect of regulating airway pressure on intrathoracic pressure and vital organ perfusion pressure during cardiopulmonary resuscitation: a non-randomized interventional cross-over study. Scand J Trauma Resusc Emerg Med 23:83
Debaty G, Metzger A, Rees J, McKnite S, Puertas L, Yannopoulos D, Lurie K (2015) Enhanced perfusion during advanced life support improves survival with favorable neurologic function in a porcine model of refractory cardiac arrest. Crit Care Med 43:1087–1095
Metzger A, Matsuura T, McKnite S, Marino BS, Nadkarni VM, Yannopoulos D (2011) Intrathoracic pressure regulation improves 24-hour survival in a pediatric porcine model of hemorrhagic shock. Pediatr Res 70:267–271
Yannopoulos D, McKnite S, Metzger A, Lurie KG (2007) Intrathoracic pressure regulation improves 24-hour survival in a porcine model of hypovolemic shock. Anesth Analg 104:157–162
Metzger A, Rees J, Kwon Y, Matsuura T, McKnite S, Lurie KG (2015) Intrathoracic pressure regulation improves cerebral perfusion and cerebral blood flow in a porcine model of brain injury. Shock 44(Suppl 1):96–102
Birch M, Kwon Y, Loushin MK, Puertas L, Prielipp R, Belani K, Beebe D (2015) Intrathoracic pressure regulation to treat intraoperative hypotension: a phase II pilot study. Eur J Anaesthesiol 32:376–380
Segal N, Parquette B, Ziehr J, Yannopoulos D, Lindstrom D (2013) Intrathoracic pressure regulation during cardiopulmonary resuscitation: a feasibility case-series. Resuscitation 84:450–453
Metzger AK, Segal N, Olson DW, Figueroa SA, Sadaka FG, Krause CA, Homuth JR, Burkhart NT, Neumann RT, Lurie KG, Convertino VA (2018) Intrathoracic pressure regulation therapy applied to ventilated patients for treatment of compromised cerebral perfusion from brain injury. J Med Case Rep 12:178
Patel N, Branson R, Salter M, Henkel S, Seeton R, Khan M, Solanki D, Koutrouvelis A, Li H, Indrikovs A, Kinsky MP (2015) Intrathoracic pressure regulation augments stroke volume and ventricular function in human hemorrhage. Shock 44(Suppl 1):55–62
Huffmyer JL, Groves DS, Scalzo DC, DeSouza DG, Littlewood KE, Thiele RH, Nemergut EC (2011) The effect of the intrathoracic pressure regulator on hemodynamics and cardiac output. Shock 35:114–116
Kiehna EN, Huffmyer JL, Thiele RH, Scalzo DC, Nemergut EC (2013) Use of the intrathoracic pressure regulator to lower intracranial pressure in patients with altered intracranial elastance: a pilot study. J Neurosurg 119:756–759
Hagiwara-Nagasawa M, Kambayashi R, Goto A, Chiba K, Wada T, Nunoi Y, Izumi-Nakaseko H, Takei Y, Matsumoto A, Lurie KG, Sugiyama A (2021) Effects of mechanical ventilation with expiratory negative airway pressure on porcine pulmonary and systemic circulation: mechano-physiology and potential application. J Physiol Sci 71:17
Yamazaki-Hashimoto Y, Nakamura Y, Ohara H, Cao X, Kitahara K, Izumi-Nakaseko H, Ando K, Yamazaki H, Ikeda T, Yamazaki J, Sugiyama A (2015) Fluvoxamine by itself has potential to directly induce long QT syndrome at supra-therapeutic concentrations. J Toxicol Sci 40:33–42
Elphinstone A, Laws S (2020) Does “heads-up” cardiopulmonary resuscitation improve outcomes for patients in out-of-hospital cardiac arrest? A systematic review. Br Paramed J 4:16–24
Pepe PE, Scheppke KA, Antevy PM, Crowe RP, Millstone D, Coyle C, Prusansky C, Garay S, Ellis R, Fowler RL, Moore JC (2019) Confirming the clinical safety and feasibility of a bundled methodology to improve cardiopulmonary resuscitation involving a head-up/torso-up chest compression technique. Crit Care Med 47:449–455
Dodd KW, Moore JC, Segal N, Lick MC, Salverda BJ, Hinke MB, Robinson AE, Debaty G, Lurie KG (2017) Elevation of the head and thorax during cardiopulmonary resuscitation improves cerebral blood flow in a swine model of prolonged cardiac arrest. Ann Emerg Med 70:S139–S140
Moore JC, Holley J, Segal N, Lick MC, Labarère J, Frascone RJ, Dodd KW, Robinson AE, Lick C, Klein L, Ashton A, McArthur A, Tsangaris A, Makaretz A, Makaretz M, Debaty G, Pepe PE, Lurie KG (2018) Consistent head up cardiopulmonary resuscitation haemodynamics are observed across porcine and human cadaver translational models. Resuscitation 132:133–139
Moore JC, Salverda B, Rojas-Salvador C, Lick M, Debaty G, Lurie GK (2021) Controlled sequential elevation of the head and thorax combined with active compression decompression cardiopulmonary resuscitation and an impedance threshold device improves neurological survival in a porcine model of cardiac arrest. Resuscitation 158:220–227
MirandaD LGD, Fifer MA (2016) Heart Failure. In: Lilly LS (ed) Pathophysiology of heart disease, 6th edn. Wolters Kluwer, Philadelphia, pp 220–248
Benowitz NL (2021) Antihypertensive agents. In: Katzung BG, Vanderah TW (eds) Basic and clinical pharmacology, 15th edn. McGraw Hill Education, New York, pp 177–198
Kaneko N, Itoh K, Sugiyama A, Izumi Y (2011) Microminipig, a non-rodent experimental animal optimized for life science research: preface. J Pharmacol Sci 115:112–114
Convertino VA (2019) Mechanisms of inspiration that modulate cardiovascular control: the other side of breathing. J Appl Physiol 127:1187–1196
Rothe CF (1993) Mean circulatory filling pressure: its meaning and measurement. J Appl Physiol 74:499–509
Gelman S (2008) Venous function and central venous pressure: a physiologic story. Anesthesiology 108:735–748
Morris MC, Niziolek GM, Blakeman TC, Stevens-Topie S, Veile R, Heh V, Zingarelli B, Rodriquez D, Branson RD, Goodman MD (2020) Intrathoracic pressure regulator performance in the setting of hemorrhage and acute lung Injury. Mil Med 185:e1083–e1090
Acknowledgements
This study was supported in part by research grants from Japan Society for the Promotion of Science (JSPS KAKENHI) grant number 20K16136 (to R.K.) and 19K16505 (to M.H-N.). The authors thank Mrs. Yuri Ichikawa for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goto, A., Kambayashi, R., Hagiwara-Nagasawa, M. et al. Impact of head-up tilt on expiratory negative airway pressure ventilation-induced cardiovascular hemodynamics in the halothane-anesthetized intact microminipigs. Heart Vessels 37, 1808–1815 (2022). https://doi.org/10.1007/s00380-022-02068-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02068-1