Abstract
Patient-reported quality of life (PRQL) is a primary therapeutic target for patients with chronic heart failure (HF) and is associated with long-term prognosis. However, its utility in hospitalized HF (HHF) patients in the acute setting remains unclear. We aimed to assess the utility of PRQL (the Kansas City Cardiomyopathy Questionnaire [KCCQ]) in HHF patients and its association with long-term prognosis as well as with the clinical risk score (Get With The Guidelines-Heart Failure [GWTG-HF] risk score). PRQL was evaluated using the KCCQ in consecutive 114 HHF patients. Its association with the composite outcome of all-cause mortality or HF readmission within the first year after discharge was analyzed. Furthermore, its distribution by the clinical risk score (GWTG-HF) was evaluated using Pearson’s correlation coefficient. The median KCCQ was 34.9, but was widely distributed (interquartile range 23.7–56.8). After adjustment for known prognostic indicators, the KCCQ was not an independent predictor of the composite outcome within the first year (group with high vs. low KCCQ scores: hazard ratio, 0.67; 95% confidence interval 0.26–1.71). There was no significant correlation between the KCCQ and the GWTG-HF risk score. In conclusion, PRQL during the acute phase of HF was significantly impaired and also varied widely, irrespective of patient characteristics or severity. PRQL assessment and risk prediction for HHF patients in the acute setting seemed to provide two distinct types of information for health care providers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is a major health problem worldwide and is associated with high morbidity and mortality [1,2,3]. In addition, patient-reported quality of life (PRQL) is also an important topic for HF patients because findings about patient’s function and well-being will help inform how clinicians manage patients hospitalized for HF (HHF) [4]. As health care strives to become more patient-centered and as payers increasingly demand evidence for optimization of PRQL, PRQL parameters are becoming important considerations for treating physicians, both at the time of admission and during follow-up after discharge for HF patients [5, 6].
The Kansas City Cardiomyopathy Questionnaire (KCCQ) is an extensively validated instrument for measuring PRQL in HF that is commonly used in clinical trials and routine care for chronic HF patients [4]. Part of its utility in clinical care stems from its strong association with long-term prognosis [7, 8]. As a crucial endorsement of the validity and reliability of the KCCQ, the US Food and Drug Administration has qualified the KCCQ to be used by medical device companies to support regulatory submissions for HF medical devices (http://cvoutcomes.org/entries/3052). However, its prognostic utility in acutely decompensated HF remains unclear. Although there are some promising findings of PRQL during the acute phase of HHF [9,10,11], few data exist about its association with long-term prognosis. Prediction of longitudinal health status at the time of baseline admission is important to tailor the individual management of HHF patients. We aimed to elucidate the distribution of the KCCQ based on patient characteristics and to investigate its associations with long-term clinical outcomes (e.g., mortality or HF readmission) in HHF patients in the acute setting. Furthermore, we focused our attention on evaluating the association between PRQL and HF severity, as assessed by another prognostic risk score.
Materials and methods
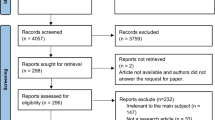
Between June 2014 and May 2016, 114 consecutive patients with HHF in a single university-based institution were included in the analysis. HHF was defined as rapid-onset HF or a change in the signs and symptoms of HF requiring urgent therapy and hospitalization based on the Framingham criteria [12]. Patients presenting with acute coronary syndrome were not included. This research was part of the West Tokyo Heart Failure Registry (WET-HF) [13], which is a large, prospective, multicenter registry designed to collect clinical data on clinical backgrounds and outcomes of HHF patients. To obtain a robust assessment of the care and patient outcomes, the baseline data and outcomes were collected via individual medical reviews by trained clinical research coordinators. Of these patients, we excluded four (3.5%) who had severe respiratory conditions requiring mechanical support and were not able to complete the questionnaire, eight (7.0%) who died during hospitalization and thus whose long-term prognosis could not be evaluated, and 15 (13.2%) who did not agree with answering the questionnaire. The remaining 87 patients with HHF who answered the KCCQ were included in the analysis. A linguistically translated KCCQ was administered by trained cardiologists (Y.S. and T.K.) within 2 days after hospital admission. We read each question aloud and recorded the patient’s responses, and all patients were able to complete the questionnaire. The KCCQ asks for “the worst situation within the last 2 weeks (including pre-admission phase of the illness),” and this was specified in our questionnaire. We believe that this would minimize the difference and prevent patients’ recall bias. Exclusive on-site auditing by the investigators (Y.S. and S.K.) ensured proper registration of each patient. The study protocol was approved by the Keio University institutional review boards, and the research was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from each subject before the study.
The KCCQ is a validated disease-specific questionnaire that measures the following health status domains: physical and social limitations, symptoms, and quality of life (QoL). These domains can be combined to generate an overall summary score that ranges from 0 to 100, with higher scores representing better health status [4]. We used the KCCQ-12, a short version of the original 23-item instrument, which is highly correlated with the original score and preserves the validity, reliability, responsiveness, prognostic importance, and interpretability of the original instrument [14]. The objective severity of HHF patients was evaluated via the Get With The Guidelines-Heart Failure (GWTG-HF) risk score, which is associated with the risk of in-hospital mortality for acute HF patients with the range of 0–100 [15]. This risk score was calculated using the seven variables on admission: race, age, systolic blood pressure, heart rate, blood urea nitrogen level, sodium concentration, and the presence of chronic obstructive pulmonary disease. This risk score has already been validated with good discrimination and calibration for Japanese HHF patients [13].
We first described the distribution of the KCCQ overall score for the entire population and within the following subgroups: female versus male, age younger than 80 years versus older than 80 years, left ventricular ejection fraction (LVEF) (cutoff, 40%), or HF status (de novo vs. readmission). Normality of continuous variables was tested with the Shapiro–Wilk test and/or Q–Q plot visual assessment, and continuous variables with normal distributions were expressed as mean ± standard deviations, and other variables were expressed as median [25th and 75th percentiles]. Differences were compared using Student’s t tests or Mann–Whitney U tests for continuous variables. Then, we divided the patients into the following three easy-to-interpret groups depending on the KCCQ score based on the intention of instrument developer [8, 16]: low KCCQ group (0 to < 25); intermediate KCCQ group (25 to < 50); and high KCCQ group (50–100). Originally, the 50 to < 75 and 75–100 groups were separated, but the number of patients in the 75–100 group was small (n = 5); thus, we combined these two groups. Accordingly, we evaluated its association with a composite outcome of mortality and readmission for worsening HF within 1 year after discharge (primary outcome). We also evaluated its association with each outcome individually (secondary outcome). We compared group differences using the Kruskal–Wallis test for continuous variables and Chi-squared tests for categorical variables. We used the log-rank test to evaluate differences in the composite outcome and Cox proportional hazard analysis to compare patient outcomes according to the KCCQ groups and adjusted for important confounders, using one-year mortality risk prediction score for HF patients (Seattle Heart Failure Model) and brain natriuretic peptide (BNP) on admission [17]. The Seattle Heart Failure Model included many predictors associated with long-term survival in patients with HF: age, New York Heart Association (NYHA), LVEF, ischemic etiology, systolic blood pressure, hemoglobin, sodium, cholesterol, percentage of lymphocytes, uric acid, medications (angiotensin-converting enzyme inhibitors, angiotensin II receptor blocker, beta-blocker, mineralocorticoid receptors antagonist, loop diuretics, statins, allopurinol), cardiac resynchronization therapy, implantable cardioverter-defibrillator, and cardiac resynchronization therapy-defibrillator. The Seattle Heart Failure Model also has been validated and recalibrated in Japanese HHF patients [18].
Finally, we investigated the association between the KCCQ and the GWTG-HF risk score using the Pearson’s correlation coefficient. We also evaluated the association between the GWTG-HF risk score and the primary outcome using Cox proportional hazard analysis. All probability values were two-tailed; P < 0.05 was considered statistically significant. All statistical analyses were performed with R 3.4.1.
Results
Overall, the median age was 78 [66.5–85] years; 37(42.5%) patients were female. The distribution of the KCCQ score is shown in Fig. 1a; the median score was 34.9 [23.7–56.8], and there were no differences in the KCCQ scores based on sex (female, n = 37: 31.3 [16.1–56.8]; male, n = 50: 40.1 [25.9–56.3]; P = 0.26) or age (< 80 years, n = 50: 38.2 [27.0–52.3]; ≥ 80 years, n = 37: 31.8 [19.8–58.3]; P = 0.70), or LVEF (HF with preserved ejection fraction, LVEF ≥ 40%, n = 55: 37.0 [22.9–58.3]; HF with reduced EF, LVEF < 40%, n = 31: 32.8 [27.3–50.5]; P = 0.83), or HF status (de novo, n = 75: 34.4 [23.2–56.8]; readmission, n = 12: 40.6 [29.0–51.3]; P = 0.55) (Fig. 1b).
a Distribution of the KCCQ score for HHF patients in the acute setting. b Comparison of the KCCQ score according to patient characteristics. KCCQ Kansas City Cardiomyopathy Questionnaire, HHF hospitalized heart failure, HFpEF heart failure with preserved ejection fraction, HFrEF heart failure with reduced ejection fraction
When we divided the patients into three groups according to the KCCQ scores, no significant differences were observed for almost all clinical characteristics, such as sex, history of HF hospitalization, LVEF, or BNP level among the three groups, except for the presence of diabetes mellitus (Table 1). The incidence of the composite outcome did not differ among the three groups (Fig. 2). After multivariable adjustment, the KCCQ score was not associated with the composite outcome (high vs. low KCCQ groups: hazard ratio [HR] 0.67; 95% confidence interval [CI] 0.26–1.71; P = 0.40). Similar results were noted when we focused on each outcome (mortality: HR 0.39; 95% CI 0.07–2.20; P = 0.29; HF readmission: HR 0.76; 95% CI 0.25–2.32, P = 0.63).
Finally, the distribution of the GWTG-HF risk score is shown in Fig. 3 (mean 40.7 ± 8.64). Pearson’s correlation coefficient revealed no significant association between the KCCQ and the GWTG-HF risk score (Pearson correlation coefficient 0.12; 95% CI 0.09–0.33; P = 0.25) (Fig. 4). After multivariable adjustment, the GWTG-HF risk score was associated with the primary outcome (HR 1.10; 95% CI 1.02–1.17; P = 0.01).
Discussion
PRQL is associated with the long-term prognosis of chronic HF patients [4, 8, 19, 20]; however, its impact on outcomes of acute decompensated HF patients has not been thoroughly investigated [9, 10]. How to best use and interpret these measures is unknown and is important to understand them because of their intrinsic value to providers. In our study, PRQL of HHF patients in the acute setting was significantly impaired (KCCQ score 34.9 [23.7–56.8]), and the KCCQ in the acute phase was not associated with long-term outcomes. We also found little association between PRQL and the GWTG-HF risk score, which is in line with the findings of the absence of association with long-term outcomes.
Despite the lack of association with the KCCQ scores at the time of hospitalization and subsequent clinical events, our data contribute to a growing body of literature on PRQL and outcomes in HF. A small pilot study showed that changes in the KCCQ score during hospitalization were not associated with 30-day HF readmission [9]. However, Dai et al. [10] demonstrated that the KCCQ used in the acute setting was significantly associated with 30-day HF readmission rates. Allen et al. [11] also showed that a low KCCQ score at admission was an independent predictor of the composite of persistently unfavorable PRQL (defined by a KCCQ score < 45 at weeks 1 and 24 after hospital discharge) or all-cause mortality. Based on these promising findings of PRQL during the acute phase of HHF, our study sought to further define the association between the KCCQ during the acute phase and long-term prognosis of HHF patients. Prediction of longitudinal health status at the time of baseline admission is important to tailor the individual management of HHF patients, for example implementation of cardiac rehabilitation or novel HF agents such as sacubitril/valsartan [21, 22].
Although our findings of little association between the KCCQ scores at the time of hospitalization and subsequent clinical outcomes are in contrast with those of other studies, such as those by Allen et al. [11], there are several potential explanations that should be considered. First, the KCCQ was designed to capture a patients’ health status over the prior 2 weeks, as has been supported by the prognostic value of serial KCCQ monitoring [7]. Hospitalization, by definition, represents an acute nadir in patients’ health status and may not be reflective of their condition after stabilization. Given the strong association of patients’ KCCQ scores at the time of hospitalization with subsequent health status [11], it can be important at predicting subsequent health status, even if it is not strongly associated with survival and rehospitalization in the year after discharge. Because patients’ health status can improve dramatically after hospitalization, the strength of the association between health status at the time of hospitalization and in recovery may differ dramatically [9]. Prior studies have shown a strong association with post-discharge (7 days) KCCQ scores and subsequent clinical events [23]. A similar phenomenon has been discovered by analyzing patients with advanced HF who underwent left ventricular assist device placement, where the preprocedure KCCQ was not associated with outcomes, but the posttransplant KCCQ was [24].
Despite the lack of a strong prognostic association with clinical events over the year after discharge, the KCCQ could provide several advantages over the NYHA classification. Most importantly, the KCCQ derives directly from patients, whereas the NYHA classification is a clinician’s interpretation of patients’ health status and is known to have substantial interoperator variability [25]. Furthermore, the KCCQ could stratify patients in more detail based on their PRQL and includes the full range of patient health (physical function, symptom frequency, social function, and QoL) compared with the NYHA functional classification. It is difficult to stratify PRQL of HHF patients with the NYHA because most patients are classified as NYHA IV. It is imperative for health care providers to evaluate PRQL from the acute phase to the chronic phase of HF patients, given the multidisciplinary nature of modern HF management and the constant need to evaluate PRQL response to various medical interventions [5, 26, 27].
The present study should be interpreted within the context of several potential limitations. Most importantly, this was a relatively small study and was likely underpowered to definitively exclude an association between the KCCQ scores at the time of hospitalization and subsequent clinical events. Second, as noted above, we investigated the KCCQ only at admission and changes in the KCCQ score during hospitalization or shortly after discharge in response to treatment may have different implications. Third, the symptoms of HF during the acute phase usually change dramatically during the first few hours, and some patients might fail to answer the symptoms during the time of administration. Fourth, this study was conducted in a single university-based institution that might affect the external validity. However, the baseline characteristics between our population and large-scale Japanese registries were almost similar, ensuring acceptable generalizability of our results across Japan [28]. Finally, because patients who died during hospitalization were not included in this analysis, this may have introduced an important selection bias, particularly if these patients had lower KCCQ scores. Further studies are warranted to establish a common way of consistently assessing PRQL of HHF patients.
In conclusion, PRQL in the acute phase of HF was significantly impaired and varied, irrespective of patient characteristics or severity. Although PRQL assessment at the time of hospitalization was not associated with traditional risk stratification methods for HHF patients, its role in predicting subsequent health status outcomes and defining when to measure patients’ health status are important goals for future research.
References
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld JA, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2017) 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure. J Am Coll Cardiol 70:776–803
Guo Y, Lip GY, Banerjee A (2013) Heart failure in East Asia. Curr Cardiol Rev 9:112–122
Sakata Y, Shimokawa H (2013) Epidemiology of heart failure in Asia. Circ J 77:2209–2217
Green CP, Porter CB, Bresnahan DR, Spertus JA (2000) Development and evaluation of the Kansas City cardiomyopathy questionnaire: a new health status measure for heart failure. J Am Coll Cardiol 35:1245–1255
Teerlink JR, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Ponikowski P, Unemori E, Voors AA, Adams KF, Dorobantu MI, Grinfeld LR, Jondeau G, Marmor A, Masip J, Pang PS, Werdan K, Teichman SL, Trapani A, Bush CA, Saini R, Schumacher C, Severin TM, Metra M (2013) Serelaxin, recombinant human relaxin-2, for treatment of acute heart failure (RELAX-AHF): a randomised placebo-controlled trial. Lancet 381:29–39
Konstam MA, Burnett JC, Maggioni AP, Swedberg K, Udelson JE, Gheorghiade M, Konstam MA, Burnett JC, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C (2007) Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST clinical status trials. JAMA 297:1332–1343
Pokharel Y, Khariton Y, Tang Y, Nassif ME, Chan PS, Arnold SV, Jones PG, Spertus JA (2017) Association of serial Kansas city cardiomyopathy questionnaire assessments with death and hospitalization in patients with heart failure with preserved and reduced ejection fraction: a secondary analysis of 2 randomized clinical trials. JAMA Cardiol 2:1315–1321
Heidenreich PA, Spertus JA, Jones PG, Weintraub WS, Rumsfeld JS, Rathore SS, Peterson ED, Masoudi FA, Krumholz HM, Havranek EP, Conard MW, Williams RE (2006) Health status identifies heart failure outpatients at risk for hospitalization or death. J Am Coll Cardiol 47:752–756
Sauser K, Spertus JA, Pierchala L, Davis E, Pang PS (2014) Quality of life assessment for acute heart failure patients from emergency department presentation through 30 days after discharge: a pilot study with the Kansas City Cardiomyopathy Questionnaire. J Card Fail 20:18–22
Dai S, Manoucheri M, Gui J, Zhu X, Malhotra D, Li S, D’Souza J, Virkram F, Chada A, Jiang H (2016) Kansas City Cardiomyopathy Questionnaire utility in prediction of 30-day readmission rate in patients with chronic heart failure. Cardiol Res Pract 2016:4571201
Allen LA, Gheorghiade M, Reid KJ, Dunlay SM, Chan PS, Hauptman PJ, Zannad F, Konstam MA, Spertus JA (2011) Identifying patients hospitalized with heart failure at risk for unfavorable future quality of life. Circ Cardiovasc Qual Outcomes 4:389–398
Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D (1993) Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation 88:107–115
Shiraishi Y, Kohsaka S, Abe T, Mizuno A, Goda A, Izumi Y, Yagawa M, Akita K, Sawano M, Inohara T, Takei M, Kohno T, Higuchi S, Yamazoe M, Mahara K, Fukuda K, Yoshikawa T (2016) Validation of the Get With The Guideline-Heart Failure risk score in Japanese patients and the potential improvement of its discrimination ability by the inclusion of B-type natriuretic peptide level. Am Heart J 171:33–39
Spertus JA, Jones PG (2015) Development and validation of a short version of the Kansas City Cardiomyopathy Questionnaire. Circ Cardiovasc Qual Outcomes 8:469–476
Peterson PN, Rumsfeld JS, Liang L, Albert NM, Hernandez AF, Peterson ED, Fonarow GC, Masoudi FA (2010) A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program. Circ Cardiovasc Qual Outcomes 3:25–32
Soto GE, Jones P, Weintraub WS, Krumholz HM, Spertus JA (2004) Prognostic value of health status in patients with heart failure after acute myocardial infarction. Circulation 110:546–551
Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD, Cropp AB, Anand I, Maggioni A, Burton P, Sullivan MD, Pitt B, Poole-Wilson PA, Mann DL, Packer M (2006) The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation 113:1424–1433
Shiraishi Y, Kohsaka S, Nagai T, Goda A, Mizuno A, Nagatomo Y, Sujino Y, Fukuoka R, Sawano M, Kohno T, Fukuda K, Anzai T, Shadman R, Dardas T, Levy WC, Yoshikawa T (2018) Validation and recalibration of Seattle Heart Failure Model in Japanese acute heart failure patients. J Card Fail 00:1–7
Kelkar AA, Spertus J, Pang P, Pierson RF, Cody RJ, Pina IL, Hernandez A, Butler J (2016) Utility of patient-reported outcome instruments in heart failure. JACC Hear Fail 4:165–175
Kato N, Kinugawa K, Seki S, Shiga T, Hatano M, Yao A, Hirata Y, Kazuma K, Nagai R (2011) Quality of life as an independent predictor for cardiac events and death in patients with heart failure. Circ J 75:1661–1669
Ades PA, Keteyian SJ, Balady GJ, Houston-Miller N, Kitzman DW, Mancini DM, Rich MW (2013) Cardiac and self-care for chronic heart failure. JACC Hear Fail 1:540–547
Lewis EF, Claggett BL, McMurray JJV, Packer M, Lefkowitz MP, Rouleau JL, Liu J, Shi VC, Zile MR, Desai AS, Solomon SD, Swedberg K (2017) Health-related quality of life outcomes in PARADIGM-HF. Circ Hear Fail 10:e003430
Dunlay SM, Gheorghiade M, Reid KJ, Allen LA, Chan PS, Hauptman PJ, Zannad F, Maggioni AP, Swedberg K, Konstam MA, Spertus JA (2010) Critical elements of clinical follow-up after hospital discharge for heart failure: insights from the EVEREST trial. Eur J Heart Fail 12:367–374
Flint KM, Spertus JA, Tang F, Jones P, Fendler TJ, Allen LA (2017) Association of global and disease-specific health status with outcomes following continuous-flow left ventricular assist device implantation. BMC Cardiovasc Disord 17:78
Williams BA, Doddamani S, Troup MA, Mowery AL, Kline CM, Gerringer JA, Faillace RT (2017) Agreement between heart failure patients and providers in assessing New York Heart Association functional class. Hear Lung 46:293–299
McMurray JJV, Teerlink JR, Bourge RC, Cleland JGF, Jondeau G, Krum H, Metra M, Connor CMO, Parker JD, Lewsey J, Frey A, Rainisio M, Kobrin I (2007) Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials. JAMA 298:2009–2019
O’Connor CM, Starling RC, Hernandez AF, Armstrong PW, Dickstein K, Hasselblad V, Heizer GM, Komajda M, Massie BM, McMurray JJ, Nieminen MS, Reist CJ, Rouleau JL, Swedberg K, Adams KF Jr, Anker SD, Atar D, Battler A, Botero R, Bohidar NR, Butler J, Clausell N, Corbalán R, Costanzo MR, Dahlstrom U, Deckelbaum LI, Diaz R, Dunlap ME, Ezekowitz JA, Feldman D, Felker GM, Fonarow GC, Gennevois D, Gottlieb SS, Hill JA, Hollander JE, Howlett JG, Hudson MP, Kociol RD, Krum H, Laucevicius A, Levy WC, Méndez GF, Metra M, Mittal S, Oh BH, Pereira NL, Ponikowski P, Tang WH, Tanomsup S, Teerlink JR, Triposkiadis F, Troughton RW, Voors AA, Whellan DJ, Zannad F, Califf RM (2011) Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med 365:32–43
Shiraishi Y, Kohsaka S, Sato N, Takano T, Kitai T, Yoshikawa T, Matsue Y (2018) 9-year trend in the management of acute heart failure in Japan: a report from the national consortium of acute heart failure registries. J Am Heart Assoc 7:e008687
Funding
This research was supported by a grant from the Japan Agency for Medical Research and Development (201439013C; S.K.), Health Labor Sciences Research Grant (14528506; S.K.), and a Grant-in-Aid for Young Scientists (JPSS KAKENHI, 18K15860 [Y.S.]). Dr. Kohsaka reports investigator-initiated grant funding from Bayer and Daiichi Sankyo and personal fees from AstraZeneka, Bayer, Bristol-Myers Squibb, Daiichi Sankyo, and Pfizer, outside the submitted work. John A. Spertus owns the copyright to the Kansas City Cardiomyopathy Questionnaire.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The other authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shoji, S., Shiraishi, Y., Sawano, M. et al. Discrepancy between patient-reported quality of life and the prognostic assessment of Japanese patients hospitalized with acute heart failure. Heart Vessels 34, 1464–1470 (2019). https://doi.org/10.1007/s00380-019-01378-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01378-1