Abstract
Renal dysfunction and its change pattern are associated with short- and long-term mortality. However, it remains to be investigated whether or not worsening renal function (WRF) defined by baseline renal function identified from different time points would provide prognostic implication on outcomes in acute coronary syndrome (ACS) patients. This study consists of 334 ACS patients (mean age 68 ± 11 years, 75% male) treated with emergent percutaneous coronary intervention (PCI). Estimated glomerular filtration rate (eGFR) was evaluated on baseline, during hospitalization, at discharge, and at 3-month follow-up. WRF was defined as a relative decrease of eGFR > 20% at 3 months using baseline eGFR identified from different time points. The primary end point was a composite event of major cardiovascular events (MACE), including all-cause death, ACS, and heart failure hospitalization. The associations of chronic kidney disease (CKD), acute kidney injury (AKI), and WRF with MACE were evaluated. During a mean follow-up of 3.3 ± 1.7 years, a total of 64 MACE were observed. Multivariable analysis revealed that CKD (hazard ratio 2.16; p = 0.018) and AKI (hazard ratio 1.95; p = 0.030) were independent predictors of MACE, but WRF did not remain as an independent predictor of MACE (p = 0.208). The highest risk was observed in AKI patients with CKD when stratified by the presence or absence of CKD and AKI. In ACS patients treated with emergent PCI, this study demonstrated that CKD and AKI were independent predictors of MACE, while there was no independent relationship between WRF and MACE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal function plays a key role in predicting disease progression and short- and long-term outcomes in patients with acute coronary syndrome (ACS) [1,2,3,4]. Acute kidney injury (AKI) is frequently observed in ACS patients treated with emergent percutaneous coronary intervention (PCI) that is accelerated by cardiogenic shock, heart failure, and preexisting chronic kidney disease (CKD) [3,4,5,6,7]. Previous studies demonstrated the substantial relationship between AKI and subsequent renal function decline [8,9,10]. Although several studies emphasize the importance of monitoring renal function after AKI [4, 9,10,12], limited data exist on the association between change pattern of renal function and long-term outcome in patients who survived ACS event.
Worsening renal function (WRF) has been shown to be associated with outcome in coronary artery disease (CAD) [8, 13, 14], heart failure (HF) [15,16,17], and other clinical settings [11, 18]. The mechanisms by which WRF increases mortality depend on a variety of different clinical settings, and prognostic implications of decline in renal function are heterogeneous [12, 16]. Since ACS involves acute hemodynamic changes on underlying risks of renal dysfunction, AKI might have started before hospital admission that can be improved by optimized medical therapy and PCI [2, 4]. These findings suggest the need for identification of appropriate baseline renal function to examine the prognostic implication of WRF in ACS patients. Thus, it remains to be seen whether WRF defined by baseline renal function identified from different time points would provide prognostic value on outcomes in patients who survived ACS. Furthermore, despite that recent evidence supports the evaluation of estimated glomerular filtration rate (eGFR) rather than serum creatinine to predict outcome [1, 11, 19], many studies have employed the WRF definition of a relative or absolute increase of serum creatinine. The present study aimed to investigate the association of renal function and its change pattern, as assessed by eGFR, with outcomes in ACS patients treated with emergent PCI.
Methods and materials
Study population and design
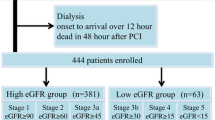
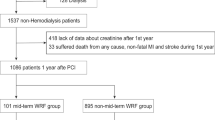
In this retrospective study, we screened consecutive 402 ACS patients who were treated with emergent PCI at Ishikiri-seiki Hospital between January 2011 and December 2014. The clinical ACS diagnosis of the present study included ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation ACS based on AHA/ACC guidelines [20, 21]. We excluded the following: patients treated with maintenance hemodialysis, n = 20; patients who died during hospitalization and within 3 months after discharge, n = 18; patients with insufficient blood sample data collection, n = 27; and lost follow-up patients, n = 3. The final analysis cohort consisted of 334 ACS patients treated with PCI. Informed consent was obtained before urgent invasive coronary angiography in all study patients. The Ethics Committee of Ishikiri-seiki Hospital approved the use of data for the purposes of this research.
PCI procedures were performed according to the guidelines for current clinical practice using a biplane X-ray system (Philips, Allura 115 Xper FD 10-10). Nonionic contrast agent (Omnipaque 350, Daiichi Sankyo Co., Tokyo, Japan) was used for the invasive coronary angiography and PCI. In our institution, consecutive intravenous saline injection was performed during and after emergent PCI [20, 21]. According to the current guidelines, the discontinuation of nephrotoxic medication was decided after the completion of emergent PCI [19, 22]. Clinical data were obtained by reviewing the medical records. Baseline blood sample tests were taken before the emergent PCI. Serum creatinine measurements were recorded at different time points, including on hospital admission, within 72 h after PCI, at discharge, and at 3-month follow-up after discharge. Furthermore, serum creatinine before hospitalization was used to assess baseline renal function if present.
Definitions
Renal function was assessed by eGFR using the CKD-EPI equation [23, 24]. CKD was defined as baseline eGFR on admission < 60 ml/min/1.73 m2. AKI was defined as an increase in serum creatinine of ≥ 0.3 mg/dl and/or ≥ 50% within 72 h after hospital admission [3, 6]. For the definition of CKD and AKI, the higher eGFR or the lower serum creatinine value measured before hospitalization (n = 153) or on hospital admission (n = 181) was used as baseline renal function, respectively. WRF was defined as a relative decrease in eGFR of > 20% at 3 months [25,26,27]. Since PCI may improve cardiac function and lead to improvement of renal dysfunction that is caused by AKI started before hospitalization, we evaluated baseline renal function at different time points for the definition of WRF. For the calculation of WRF, the highest eGFR value was used as a “baseline eGFR” identified from different time points, including before hospitalization, on hospital admission, and at discharge. Contrast-induced nephropathy (CIN) risk score was calculated using parameters on hospital admission as described previously [28].
End point
The primary end point was defined as a composite event of all-cause death, ACS requiring coronary revascularization, and HF hospitalization. Outcome data were collected and adjudicated by two cardiologists (H.K. and N.K.) through the medical records for a period starting with hospital admission and ending with the last visit to our hospital up to 5 years in all study patients. All-cause death and ACS requiring coronary revascularization were judged according to the medical record in our hospital. HF hospitalization was recorded when patients were admitted to hospital with HF symptoms showing any evidence of congestion and/or biomarker increase in association with transthoracic cardiac echocardiographic examination. All patients were followed with a scheduled revaluation at every 2–3 months after discharge in our institution. Further assessments were planned according to the clinical status of each patient.
Statistical analysis
Continuous variables were expressed as mean ± SD and were compared by using the unpaired Student’s t test. Categorical variables were summarized as frequencies with percentages and compared by Pearson χ2 analysis. Comparisons between continuous variables at baseline, after PCI, and follow-up examination of eGFR were performed with paired t test. Univariate and multivariate Cox regression analyses were carried out to determine the predictors of WRF. The effect of variables on outcome was investigated with univariate and multivariate Cox proportional-hazard model. Multivariate model included the variables with a p value ˂ 0.05 in the univariate analysis except for medications. Furthermore, considering the underlying high-risk clinical profile and condition, we performed Cox proportional-hazard analysis to investigate independent predictors of MACE in patients with STEMI as a sub-analysis. For survival analysis, time-to-event data for ACS and STEMI patients were presented as Kaplan–Meier estimates. All statistical analyzes were performed using the SPSS software version 22 (SPSS Japan Inc, Tokyo, Japan) and p values < 0.05 (2-sided) were considered statistically significant.
Results
Patient characteristics and serial changes in renal function
In the present study, WRF was observed in 71 patients (21%). The baseline clinical and angiographic characteristics in patients with and without WRF are shown in Table 1. Compared to the non-WRF patients, WRF patients had advanced age (p = 0.004), lower eGFR (p < 0.001) and higher BNP (p = 0.001). When compared to non-WRF patients, WRF patients were more likely to have NYHA III/IV (p < 0.001), CKD (p < 0.001), AKI (p < 0.001), diuretics therapy (p < 0.001) and CIN risk score > 17 (p < 0.001). Figure 1 shows the serial changes in eGFR in patients with and without CKD, AKI, WRF and MACE, respectively. CKD patients had lower eGFR than non-CKD patients at all the different time points, while both CKD and non-CKD patients had slightly but significantly decreased eGFR at 3 months (p < 0.001) compared to baseline (Fig. 1a). Both AKI and non-AKI patients had significantly decreased eGFR at 3 months compared to baseline (Fig. 1b). When compared with non-AKI patients, AKI patients showed a greater change in eGFR at 3 months. Although there was significant difference in baseline eGFR between WRF and non-WRF patients, the difference between the two groups was more highlighted at 3 months (Fig. 1c). Compared to the non-MACE group, the MACE group showed significantly lower eGFR at all the different time points and decreased eGFR at 3 months over baseline as well as non-MACE patients (Fig. 1d). When analyzing the 153 patients who had baseline renal function before hospitalization, the eGFR on hospital admission was significantly decreased compared to baseline eGFR before hospitalization (75 ± 20 versus 67 ± 22 ml/min/1.73 mm2; p < 0.001). Decreased eGFR was observed in 75% of the patients who had baseline eGFR (n = 153). Furthermore, when analyzing the difference in eGFR between hospital admission and discharge in 334 ACS patients, the eGFR at discharge was significantly improved from the value measured on hospital admission (71.4 ± 20 versus 73.2 ± 19; p = 0.005). The improvement of eGFR at discharge was observed in 46% of ACS patients. Multivariable regression analysis revealed that CKD (β = 1.68, p < 0.001) and AKI (β = 1.255, p = 0.001) were independent predictors of WRF, as shown in Table 2.
Serial change of eGFR according to the presence or absence of CKD, AKI, WRF, and MACE. Serial change of eGFR in patients with and without CKD (a), AKI (b), WRF (c), and MACE (d). Tables below the graphs show the mean ± SD of eGFR at each time point. p value in the tables indicates statistical difference in eGFR between the two groups at each time point. p value in the graph indicates statistical difference in eGFR between baseline and 3-month (** and * indicate p < 0.001 and p < 0.05, respectively). AKI acute kidney injury, CKD chronic kidney disease, MACE major adverse cardiovascular event, and WRF worsening renal function
Patient outcome
During a mean follow-up of 3.3 ± 1.7 years, a total of 64 patients were in primary end point (all-cause death, n = 25; ACS requiring revascularization, n = 21; and HF hospitalization, n = 18), as shown in Table 3. The baseline patient and angiographic characteristics in patients with and without MACE are shown in Table 4. Compared with the non-MACE group, the MACE group was more likely to have advanced age (p = 0.003), decreased eGFR (p = 0.007) and lower hemoglobin levels (p = 0.014) and had higher prevalence of left ventricular ejection fraction (LVEF) ≤ 40% (p = 0.011), diuretic therapy (p = 0.002) and statin therapy (p = 0.018). For angiographic characteristics, there was no significant difference in prevalence of LAD culprit lesion (p = 0.88) and contrast volume (p = 0.94). The lower risks of CIN risk score were more common in the non-MACE group (Table 4). Figure 2 shows the incidence of MACE in patients with and without CKD, AKI and WRF. When compared to patients without each renal complication, significantly higher incidence for MACE was observed in patients with CKD (p < 0.001), AKI (p < 0.001) and WRF (p < 0.001), respectively.
Incident rates of MACE during follow-up. Accumulating rates for MACE during follow-up according to the presence (red bar) and absence (blue bar) of each group, including CKD, AKI, and WRF. AKI acute kidney injury, CKD chronic kidney disease, MACE major adverse cardiovascular event, and WRF worsening renal function
Predictors of MACE
Table 5 shows the univariate and multivariate Cox hazard analyzes to predict MACE for all study patients (model 1) and STEMI patients (model 2). Multivariable analysis model 1 revealed that baseline CKD [hazard ratio (HR) 2.16; 95% confidence interval (CI) 1.14–4.09; p = 0.018] and AKI (HR 1.95; 95% CI 1.06–3.58; p = 0.030) were independent predictors of MACE (Table 5 model 1), while WRF did not remain as an independent predictor of MACE (p = 0.208) in ACS patients. To investigate the prognostic implication of WRF defined by serum creatinine, we also performed multivariate analysis to predict MACE in ACS patients, where WRF was defined by an increase in serum creatinine of ≥ 0.3 mg/dl and/or ≥ 50% within 72 h. Similarly, independent predictors of MACE were CKD (HR 2.49; 95% CI 1.350–4.613, p = 0.004) and AKI (HR 2.13; 95% CI 1.176–3.875, p = 0.013). In the sub-analysis of STEMI patients, the multivariate model 2 demonstrated that CKD (HR 2.56; 95% CI 1.14–5.70; p = 0.021) and AKI (HR 3.18; 95% CI 1.52–6.63; p = 0.002) were independent predictors of MACE. The cumulative rates of MACE are shown as Kaplan–Meier estimates in Fig. 3. Figure 3a demonstrates a graded risk of MACE when stratified by the presence or absence of CKD and AKI. Although the AKI patients with WRF had the worst prognosis during follow-up, non-AKI patients with or without WRF showed similar outcomes (Fig. 3b). The non-CKD patients without WRF had benign outcome compared to other groups (Fig. 3c). Similar results were obtained when analysis was performed only in STEMI patients (Fig. 3d–f).
Time-to-event curves for MACE during follow-up in patients with ACS and STEMI. The cumulative rates of MACE are shown as Kaplan–Meier estimates according to the presence or absence of AKI and CKD (a), AKI and WRF (b), CKD and WRF (c) for patients with ACS; and AKI and CKD (d), AKI and WRF (e), CKD and WRF (f) for patients with STEMI. AKI acute kidney injury, CKD chronic kidney disease, MACE major adverse cardiovascular event, STEMI ST-segment elevation myocardial infarction, and WRF worsening renal function
Discussion
This study demonstrated that baseline renal dysfunction and AKI were independent predictors of MACE, while WRF did not remain as an independent predictor of MACE in ACS patients treated with emergent PCI. Our findings confirm the prognostic significance of renal dysfunction and AKI and may provide practical insights into change pattern of renal dysfunction and long-term outcomes in ACS patients treated with emergent PCI.
Prognostic significance of CKD and AKI
The high prevalence of renal dysfunction among ACS patients is well documented with its substantial association of adverse outcomes [1,2,3,4,5,6]. In the present study, baseline CKD was observed in 20% of patients, which is similar to that in previous reports (17.9–34%) [1,2,3,4, 6, 7, 14, 29]. Anavekar et al. demonstrated that even mild decline in renal function, as assessed by the eGFR, was associated with increased risk of cardiovascular events after acute myocardial infarction [1]. Renal dysfunction is known to be associated with worse prognosis in CAD [3, 4, 6,7,8], HF [15,16,17] and other clinical settings [11, 18]; however, few studies have reported its change pattern in ACS patients treated with PCI.
This study demonstrates that AKI was a robust predictor of MACE, while there was no independent relationship between WRF and outcome in ACS. It is well established that AKI is a frequent complication and associates with worse prognosis in multiple populations [3, 4, 6,7,8,9,10, 18, 30], independent of residual kidney function [31]. In the present study, we observed a graded risk when patients were stratified by the presence of CKD and AKI. Watabe et al. have found that contrast-induced AKI was an incremental predictor of cardiovascular outcome at each stage of CKD in ACS patients [3]. Furthermore, accumulating evidence demonstrated that a greater decline in renal function during AKI, such as severe AKI resulting in renal replacement therapy, was associated with a poorer patient prognosis [2, 4, 19]. As a surrogate end point of outcome, the identification of AKI rather than WRF may serve as a robust predictor of long-term outcomes in ACS patients.
Worsening renal function and outcome
The mechanisms by which WRF increases hazard risk of outcomes may involve the progression to CKD, side effects of medical therapies and heterogeneity of underlying causes and diseases. AKI severity and multiple hits of AKI predispose patients to faster progression of subsequent CKD progression [10]. Nemoto et al., demonstrated that continuous deterioration in kidney function was an independent predictor of mortality in ACS patients; however, AKI was not included in the multivariate model to predict the outcome [14]. In the present study, we found that CKD and AKI were robust factors associated with WRF, contributing to reducing the prognostic significance of WRF.
Sawhney et al., suggest that the long-term prognosis after AKI varies depending on the clinical setting with underlying pre- and post-AKI renal function rather than zthe AKI itself [12]. Maioli et al., demonstrated that persistent renal damage after AKI showed poorer outcomes compared to those with transient AKI in CAD patients with estimated creatinine clearance < 60 ml/min [8]. In line with the previous study, we found that patients having AKI and WRF showed poorer outcomes compared to other groups, both in ACS and STEMI patients. On the other hand, we observed that non-AKI with WRF had similar outcomes compared to non-AKI without WRF. Considering the substantial associations of CKD and its severity with outcomes [1,2,3,4], it is likely that CKD influences the prognosis in non-AKI patients with or without WRF, and appropriate definition for WRF may be different among patients with and without CKD, and also among patients with different CKD stages. Furthermore, pre-existing AKI starting before hospital admission may cause misclassification of WRF in ACS patients. An observational study demonstrated that 11% of ACS patients had improved renal function during hospitalization [2]. In fact, we observed deterioration of eGFR on hospital admission in patients having baseline renal function before hospitalization, which was improved at discharge. These observations suggest that AKI might have started before hospitalization in the ACS population, which can be improved by appropriate medical therapy and PCI [2, 4]. Since no effective therapy for AKI is available [32], early identification of AKI may help better risk stratification of ACS patents treated with emergent PCI.
Study limitations
This study has several limitations. First, this was a single-center retrospective study consisting of a relatively small number of patients. Second, this study excluded patients who died in hospital and within 3 months in the study cohort. These exclusions may have attenuated the prognostic value of baseline renal dysfunction and AKI as well as other clinical predictors on patient prognosis. In addition, the prognostic significance of advanced age may also have been attenuated, since these high-risk populations included patients with relatively advanced age. Third, although previous studies demonstrated that renal replacement therapy following AKI has been shown to be associated with poorer patient outcomes, we did not include renal replacement therapy in the multivariate model to predict WRF and MACE due to its low incidence in the present study. However, the rate of renal replacement therapy in the present study was similar to the previous reports [33]. Fourth, although many studies have evaluated WRF by an absolute or relative increase of serum creatinine over baseline levels [8, 12, 14, 16, 18], we used WRF definition based on eGFR. However, recent evidence supports the evaluation of eGFR rather than the serum creatinine to predict adverse outcome [11, 19, 34]. Future prospective study is necessary to investigate the association of eGFR decline with patient outcomes. Fifth, we found baseline renal function before hospitalization only in 46% of the study patients. Although it is difficult to evaluate true renal function at baseline in ACS patients treated with emergent PCI, the missing data for baseline renal function may affect the classification of CKD, AKI and WRF. However, the strength of the present study is that we defined the WRF on the basis of baseline eGFR determined from different time points of data collection. Finally, for the retrospective study nature, the present study did not include analysis to determine the association of medical therapies and renovascular protection strategies, including discontinuation of nephrotoxic medications and effects of renal protective drugs with outcomes [19, 35, 36]. Future well-designed study is needed to investigate the associations of the effects of medical therapies on WRF with patient prognosis in the ACS population.
Conclusions
Our data provide practical insights into change pattern of renal dysfunction and long-term outcomes in ACS patients treated with PCI. The baseline renal dysfunction and AKI were strong predictors of outcome in this population. Future studies are necessary to assess whether WRF is associated with outcome in ACS patients treated with PCI.
References
Anavekar NS, McMurray JJV, Velazquez EJ, Solomon SD, Kober L, Rouleau J-L, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM, Pfeffer MA (2004) Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med 351:1285–1295
Marenzi G, Cabiati A, Cosentino N, Assanelli E, Milazzo V (2014) Prognostic significance of serum creatinine and its change patterns in patients with acute coronary syndromes. Am Heart J 169:363–370
Watabe H, Sato A, Hoshi T, Takeyasu N, Abe D, Akiyama D, Kakefuda Y, Nishina H, Noguchi Y, Aonuma K (2014) Association of contrast-induced acute kidney injury with long-term cardiovascular events in acute coronary syndrome patients with chronic kidney disease undergoing emergent percutaneous coronary intervention. Int J Cardiol 174:57–63
Marenzi G, Cosentino N, Bartorelli AL (2015) Acute kidney injury in patients with acute coronary syndromes. Heart 101:1778–1785
Matsue Y, Matsumura A, Abe M, Ono M, Seya M, Nakamura T, Iwatsuka R, Mizukami A, Setoguchi M, Nagahori W, Ohno M, Suzuki M, Hashimoto Y (2013) Prognostic implications of chronic kidney disease and anemia after percutaneous coronary intervention in acute myocardial infarction patients. Heart Vessels 28:19–26
Abe D, Sato A, Hoshi T, Kakefuda Y, Watabe H, Ojima E, Hiraya D, Harunari T, Takeyasu N, Aonuma K (2014) Clinical predictors of contrast-induced acute kidney injury in patients undergoing emergency versus elective percutaneous coronary intervention. Circ J 78:85–91
Shacham Y, Leshem-Rubinow E, Gal-Oz A, Arbel Y, Keren G, Roth A, Steinvil A (2015) Acute cardio-renal syndrome as a cause for renal deterioration among myocardial infarction patients treated with primary percutaneous intervention. Can J Cardiol 31:1240–1244
Maioli M, Toso A, Leoncini M, Gallopin M, Musilli N, Bellandi F (2012) Persistent renal damage after contrast-induced acute kidney injury: Incidence, evolution, risk factors, and prognosis. Circulation 125:3099–3107
Coca SG, Singanamala S, Parikh CR (2012) Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int 81:442–448
Siew ED, Parr SK, Abdel-Kader K, Eden SK, Peterson JF, Bansal N, Hung AM, Fly J, Speroff T, Ikizler TA, Matheny ME (2016) Predictors of recurrent AKI. J Am Soc Nephrol 27:1190–1200
Coresh J, Turin TC, Matsushita K, Sang Y, Ballew SH, Appel LJ, Arima H, Chadban SJ, Cirillo M, Djurdjev O, Green JA, Heine GH, Inker LA, Irie F, Ishani A, Iiix JH, Kovesdy CP, Marks A, Ohkubo T, Shalev V, Shankar A, Wen CP, de Jong PE, Iseki K, Stengel B, Gansevoort RT, Levey AS (2014) Decline in estimated glomerular filtration rate and subsequent risk of end-stage renal disease and mortality. JAMA 311:2518–2531
Sawhney S, Mitchell M, Marks A, Fluck N, Black C (2015) Long-term prognosis after acute kidney injury (AKI): what is the role of baseline kidney function and recovery? A systematic review. BMJ Open 5:e006497
Ogita M, Sakakura K, Nakamura T, Funayama H, Wada H, Naito R, Sugawara Y, Kubo N, Ako J, Momomura SI (2012) Association between deteriorated renal function and long-term clinical outcomes after percutaneous coronary intervention. Heart Vessels 27:460–467
Nemoto N, Iwasaki M, Nakanishi M, Araki T, Utsunomiya M, Hori M, Ikeda N, Makino K, Itaya H, Iijima R, Hara H, Takagi T, Joki N, Sugi K, Nakamura M (2014) Impact of continuous deterioration of kidney function 6 to 8 months after percutaneous coronary intervention for acute coronary syndrome. Am J Cardiol 113:1647–1651
Damman K, Navis G, Voors AA, Asselbergs FW, Smilde TDJ, Cleland JGF, van Veldhuisen DJ, Hillege HL (2007) Worsening renal function and prognosis in heart failure: systematic review and meta-analysis. J Card Fail 13:599–608
Damman K, Valente MAE, Voors AA, O’Connor CM, Van Veldhuisen DJ, Hillege HL (2014) Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J 35:455–469
Beldhuis IE, Streng KW, Ter Maaten JM, Voors AA, van der Meer P, Rossignol P, McMurray JJV, Damman K (2017) Renin-angiotensin system inhibition, worsening renal function, and outcome in heart failure patients with reduced and preserved ejection FractionCLINICAL PERSPECTIVE. Circ Hear Fail 10:e003588
Pannu N, James M, Hemmelgarn B, Klarenbach S (2013) Association between AKI, recovery of renal function, and long-term outcomes after hospital discharge. Clin J Am Soc Nephrol 8:194–202
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, Herzog CA, Joannidis M, Kribben A, Levey AS, MacLeod AM, Mehta RL, Murray PT, Naicker S, Opal SM, Schaefer F, Schetz M, Uchino S (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H, Lincoff AM, Peterson ED, Philippides GJ, Theroux P, Wenger NK, Zidar JP, Jacobs AK (2011) 2011 ACCF/AHA focused update of the guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline): a Report of the American College of Cardiology Foundation/American Heart Association. Circulation 123:2022–2060
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Ting HH, O’Gara PT, Kushner FG, Ascheim DD, Brindis RG, Casey DE Jr, Chung MK, de Lemos JA, Diercks DB, Fang JC, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX (2016) 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction. J Am Coll Cardiol 67:1235–1250
Jurado-Román A, Hernández-Hernández F, García-Tejada J, Granda-Nistal C, Molina J, Velázquez M, Albarrán A, Tascón J (2015) Role of hydration in contrast-induced nephropathy in patients who underwent primary percutaneous coronary intervention. Am J Cardiol 115:1174–1178
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S (2010) Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis 56:32–38
Ohsawa M, Tanno K, Itai K, Turin TC, Okamura T, Ogawa A, Ogasawara K, Fujioka T, Onoda T, Yoshida Y, Omama S, Ishibashi Y, Nakamura M, Makita S, Tanaka F, Kuribayashi T, Koyama T, Sakata K, Okayama A (2013) Comparison of predictability of future cardiovascular events between chronic kidney disease (CKD) stage based on CKD epidemiology collaboration equation and that based on modification of diet in renal disease equation in the Japanese general population. Circ J 77:1315–1325
Testani JM, Kimmel SE, Dries DL, Coca SG (2011) Prognostic importance of early worsening renal function after initiation of angiotensin-converting enzyme inhibitor therapy in patients with cardiac dysfunction. Circ Hear Fail 4:685–691
Rossignol P, Cleland JGF, Bhandari S, Tala S, Gustafsson F, Fay R, Lamiral Z, Dobre D, Pitt B, Zannad F (2012) Determinants and consequences of renal function variations with aldosterone blocker therapy in heart failure patients after myocardial infarction: insights from the eplerenone post-acute myocardial infarction heart failure efficacy and survival study. Circulation 125:271–279
Hijazi Z, Hohnloser SH, Andersson U, Alexander JH, Hanna M, Keltai M, Parkhomenko A, López-Sendón JL, Lopes RD, Siegbahn A, Granger CB, Wallentin L (2016) Efficacy and safety of apixaban compared with warfarin in patients with atrial fibrillation in relation to renal function over time: Insights from the Aristotle randomized clinical trial. JAMA Cardiol 1:451–460
Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, Leon MB, Dangas G (2004) A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention. J Am Coll Cardiol 44:1393–1399
Giacoppo D, Madhavan MV, Baber U, Warren J, Bansilal S, Witzenbichler B, Dangas GD, Kirtane AJ, Xu K, Kornowski R, Brener SJ, Généreux P, Stone GW, Mehran R (2015) Impact of contrast-induced acute kidney injury after percutaneous coronary intervention on short- and long-term outcomes: pooled analysis from the HORIZONS-AMI and ACUITY trials. Circ Cardiovasc Interv 8:e002475
Yang L, Xing G, Wang L, Wu Y, Li S, Xu G, He Q, Chen J, Chen M, Liu X, Zhu Z, Yang L, Lian X, Ding F, Li Y, Wang H, Wang J, Wang R, Mei C, Xu J, Li R, Cao J, Zhang L, Wang Y, Xu J, Bao B, Liu B, Chen H, Li S, Zha Y, Luo Q, Chen D, Shen Y, Liao Y, Zhang Z, Wang X, Zhang K, Liu L, Mao P, Guo C, Li J, Wang Z, Bai S, Shi S, Wang Y, Wang J, Liu Z, Wang F, Huang D, Wang S, Ge S, Shen Q, Zhang P, Wu L, Pan M, Zou X, Zhu P, Zhao J, Zhou M, Yang L, Hu W, Wang J, Liu B, Zhang T, Han J, Wen T, Zhao M, Wang H (2015) Acute kidney injury in China: a cross-sectional survey. Lancet 386:1465–1471
Lafrance JP, Miller DR (2010) Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol 21:345–352
Vanmassenhove J, Kielstein J, Jörres A, Van Biesen W (2017) Management of patients at risk of acute kidney injury. Lancet 389:2139–2151
Nikolsky E, Mehran R, Turcot D, Aymong ED, Mintz GS, Lasic Z, Lansky AJ, Tsounias E, Moses JW, Stone GW, Leon MB, Dangas GD (2004) Impact of chronic kidney disease on prognosis of patients with diabetes mellitus treated with percutaneous coronary intervention. Am J Cardiol 94:300–305
Stevens PE, Levin A (2014) Evaluation and Management of Chronic Kidney Disease : Synopsis of the Kidney Disease : Improving Global Outcomes 2012 Clinical Practice Guideline. Ann Intern Med 158:825–831
Kinoshita M, Okayama H, Kosaki T, Hosokawa S, Kawamura G, Shigematsu T, Takahashi T, Kawada Y, Hiasa G, Yamada T, Matsuoka H, Kazatani Y (2018) Favorable effects of early tolvaptan administration in very elderly patients after repeat hospitalizations for acute decompensated heart failure. Heart Vessels 33:163–169
Matsumoto K, Ehara S, Nakamura Y, Otsuka K, Kawase Y (2018) The effects of tolvaptan dose on cardiac mortality in patients with acute decompensated heart failure after hospital discharge. Heart Vessels 33:1204–1213
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Otsuka, K., Shimada, K., Katayama, H. et al. Prognostic significance of renal dysfunction and its change pattern on outcomes in patients with acute coronary syndrome treated with emergent percutaneous coronary intervention. Heart Vessels 34, 735–744 (2019). https://doi.org/10.1007/s00380-018-1291-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1291-5