Abstract
There are some cases that are difficult to cure with only circumferential pulmonary vein isolation (CPVI) of persistent atrial fibrillation (PerAF). Recently, prolonged interatrial conduction times (IACTs), which seem to be associated with progressive remodeled atria, have been reported as a predictor of new-onset AF. This study aimed to investigate the prognostic value of a prolonged IACT for predicting AF recurrences after CPVI of PerAF. One hundred thirteen patients who underwent CPVI without an empirical substrate modification of PerAF were retrospectively analyzed. The IACT was defined as the interval from the earliest P-wave onset on the ECG to the latest activation in the coronary sinus and was measured after achieving the CPVI and conversion to sinus rhythm. During a mean 22.7-month follow-up after the initial procedure, 56 patients (50%) had AF recurrences. Patients with AF recurrence had a longer IACT than those without AF recurrence (p < 0.001). The best discriminative cut-off value for the IACT was 123 ms (sensitivity 53%, specificity 85%). In a Cox multivariate analysis, a prolonged IACT of ≥ 123 ms was the only independent predictor (hazard ratio: 2.38; 95% confidence interval: 1.36–4.16, p = 0.002) of being associated with the incidence of an AF recurrence. Even after multiple CPVI procedures, patients with an IACT ≥ 123 ms had a higher AF recurrence rate than those with an IACT < 123 ms (p = 0.002). In conclusion, a prolonged IACT of ≥ 123 ms may be a useful marker for predicting AF recurrences after both initial and multiple CPVI procedures for PerAF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radiofrequency catheter ablation of persistent atrial fibrillation (PerAF) is more challenging than that of paroxysmal AF (PAF) [1,2,3,4,5,6]. A previous randomized controlled trial demonstrated that an empirical extensive substrate modification targeting roof and mitral isthmus linear lesions or complex fractionated electrograms could not improve the cure rate as compared to circumferential pulmonary vein isolation (CPVI) alone [1]. However, AF recurrences after CPVI alone are still frequent in patients with PerAF and there are some cases that are difficult to cure even after undergoing multiple procedures [1,2,3,4,5,6]. We still only have a few available parameters for distinguishing those who are appropriate to undergo only a CPVI and those in whom we have to consider another extensive substrate modification to improve the procedural outcome.
A prolonged total atrial conduction time has been reported to be associated with AF recurrences after catheter ablation in patients with PAF [7,8,9,10,11]. Recently, a new method to evaluate the total atrial conduction time, the so-called interatrial conduction time (IACT), has been proposed as an independent marker associated with the incidence of AF [12,13]. The IACT was defined as the interval between the high right atrium and distal coronary sinus atrial electrogram and can be measured easily and quickly during an invasive electrophysiological study. Therefore, the aim of this study was to investigate the predictive value of a prolonged IACT associated with AF recurrences after the CPVI without an empirical extensive substrate modification in patients with PerAF.
Materials and methods
Study population
In this observational, retrospective cohort study, consecutive patients who underwent their initial catheter ablation for symptomatic, drug-refractory PerAF between August 2012 and December 2016 at the Tokyo Women’s Medical University Hospital were enrolled. PerAF was defined according to the Heart Rhythm Society, European Society of Cardiology, and European Cardiac Arrhythmia Society 2012 Consensus Statement on Catheter and Surgical Ablation of AF [14]. All patients underwent transthoracic and transesophageal echocardiography, and multidetector computed tomography using a 64-slice CT scanner within 2 days prior to the scheduled ablation procedure as a preoperative evaluation. Before the procedure, all antiarrhythmic drugs (AADs) were discontinued for at least 5 half-lives. Patients who had been prescribed amiodarone were excluded from this study. Furthermore, patients who were pacemaker dependent were also excluded. All patients gave their written informed consent before the procedures. The study was approved by the local institutional ethics board.
Catheter ablation of PerAF
The details of the ablation technique have been previously described [15]. In brief, following the insertion of the sheaths, an initial intravenous bolus of 5,000 IU of heparin were given, and repeated doses of heparin were given to maintain an activated clotting time between 300 and 350 s. A decapolar or duodecapolar catheter was advanced into the coronary sinus via a jugular or femoral vein, until a stable position was achieved beyond the lateral margin of the cardiac silhouette in the 45° left anterior oblique fluoroscopic view. After a transseptal puncture, 2 long sheaths were introduced into the left atrium (LA). Before beginning the ablation, electrical cardioversion was performed to convert to sinus rhythm. If sinus rhythm was hard to restore due to the immediate recurrence, ablation was performed firstly during an AF rhythm. All patients underwent a wide CPVI guided by electroanatomical mapping combined with image integration. A 3.5-mm cooled-tip catheter (Navistar ThermoCool or ThermoCool SF, Biosense Webster Inc., Diamond Bar, CA, USA) was utilized for mapping and ablation. Radiofrequency energy was delivered to the atrial tissue with a power of 25–30 W using irrigation rates of 17 mL/min with the Navistar ThermoCool or 8 mL/min with the Navistar ThermoCool SF to achieve the desired power delivery. The power was limited to 20–25 W at the posterior wall of the LA. After achieving a bilateral CPVI, if the rhythm was still not in sinus rhythm, another electrical cardioversion was performed. Then, a superior vena cava (SVC) isolation was systematically and empirically performed except for in the absence of electrical potentials. After that, an intravenous injection of a 10 μg bolus of isoproterenol and an administration of adenosine triphosphate was given to provoke a reconnection of the LA-pulmonary veins (PVs) and right atria-SVC junction. If any sustained atrial tachycardias (ATs) or reproducible premature atrial contractions (PACs) that could be mapped were induced by programmed electrical stimuli with/without an injection of a 10 μg bolus of isoproterenol, they were targeted for ablation. A cavotricuspid isthmus (CTI) linear ablation was performed only if common atrial flutter was documented before the procedure or was induced during the procedure. No empirical substrate modification targeting linear lesions or complex fractionated electrograms was performed during the procedures.
Measuring the IACT
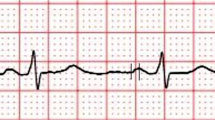
The IACT was defined as the interval from the earliest P-wave onset in all twelve ECG leads to the latest activation on the coronary sinus catheter during sinus rhythm at a sweep speed of 100 mm/s (Fig. 1). In each patient, the IACT was measured at a point in time immediately after achieving the bilateral CPVI and conversion to sinus rhythm. For evaluating the feasibility to measure the IACT before undergoing the CPVI, the IACT was also measured at a point immediately after the initial electrical cardioversion before undergoing the CPVI in the cases that could achieve sinus conversion. Furthermore, for evaluating the correlation between the IACT and P-wave duration, the max P-wave duration (MPWD) was also measured at a point in time immediately after achieving a bilateral CPVI. The MPWD was measured from the earliest onset to the latest offset in all twelve ECG leads. Those measurements were all made using digital calipers on a polygraph system by two trained observers blinded to the clinical data.
Measurement of the interatrial conduction time (IACT) in the surface electrocardiogram leads (I and V1) and intracardiac electrograms. The IACT was defined as the interval from the earliest P-wave onset in all 12 ECG leads to the latest activation on the coronary sinus catheter during sinus rhythm at a sweep speed of 100 mm/s. CS coronary sinus, pro proximal, dis distal
To evaluate the inter-rater reliability of the measured results, two trained observers blinded to clinical data independently measured the IACT and MPWD at the same point for each patient. Further, to evaluate the intra-rater reliability, one observer measured the parameters twice at the same point on different days.
Follow-up
All patients were scheduled for outpatient visits at 1, 2, 3, 6, 9, and 12 months after the procedures and then every 6 months. AF recurrences were evaluated by the symptoms, ECG recordings, and 24-h ambulatory monitoring (1, 3, 6, 9, and 12 months after the ablation and then every 6 months). Patients with palpitations were encouraged to use portable ECG monitoring (HCG-801R; Omron, Kyoto, Japan). Recurrence was defined as recurrent symptoms and/or documented AF on the ECG, 24-h ambulatory monitoring, or portable ECG monitoring (lasting > 30 s) after a 2-month blanking period from the ablation procedure. The discontinuation of AADs was recommended 3 months after the procedures.
The repeat ablation
The electrophysiological study was the same as that in the initial procedure. First of all, re-isolation of all PVs and the SVC was performed by targeting the recovery of the electrical potentials along the previous ablation line during sinus or an atrial pacing rhythm. After that, if any sustained ATs or reproducible PACs that could be mapped were induced by programmed electrical stimuli with the administration of isoproterenol, those were mapped and ablated. However, an empirical substrate modification was not also performed during the repeat procedures.
Statistical analysis
The continuous variables are described as the mean ± standard deviation (SD), or median (first quartile, third quartile). The Student t test, Fisher exact test, and Mann–Whitney U test were used to compare the differences across the two groups. All tests were two-sided, and statistical significance was set at a value of p < 0.05. The inter-rater and intra-rater reliabilities for measuring the IACT and MPWD were analyzed using intra-class correlation coefficients (ICC). Correlations between the parameters were evaluated by the Spearman correlation test. A Cox proportional hazards model was used to identify predictors of AF recurrences after the initial ablation. All parameters with a p value < 0.05 in the univariate analysis were entered into the multivariate model. A Kaplan–Meier analysis with a log-rank test was used to determine the probability of the freedom from AF recurrences after ablation. A p value < 0.05 was considered significant. The data were analyzed by SPSS software version 23.0 (SPSS Inc, Chicago, IL).
Results
Baseline characteristics according to the AF recurrences after the initial procedures
One hundred and twenty-seven patients underwent an initial ablation procedure during the period. Among those patients, 8 who had been prescribed amiodarone, 5 who were pacemaker dependent, and 1 with junctional rhythm during the entire procedure were excluded and the remaining 113 patients were analyzed.
A flow chart of the rhythm management during the initial procedures is summarized in Fig. 2. Among the 113 patients, 92 (81%) had sinus conversion after an initial electrical cardioversion. A bilateral CPVI was successfully achieved in all patients. After achieving the CPVI, another electrical cardioversion was required in 35 patients (31%) including 21 who had an immediate AF recurrence after the initial electrical cardioversion and 14 who had another AF recurrence during the ablation. Finally, sinus rhythm was restored in all patients.
An SVC isolation was performed in 89 patients (79%) and a CTI linear ablation in 25 (22%). Three ATs (3%) originating from the mitral annulus, left atrial appendage, and right atrial free wall, and three PACs (3%) originating from the atrial septum, posterior LA, and crista terminalis were induced during the procedures and successfully ablated.
During a mean follow-up of 22.7 months after the initial procedure, 56 patients (50%) had an AF recurrence without any AADs. All patients were divided into two groups based on the presence or absence of an AF recurrence after the initial procedure. The baseline characteristics of the two groups are shown in Table 1. Patients with AF recurrences had a significantly higher BMI, higher prevalence of hypertension, larger left atrial volume (LAV), lower achievement of sinus conversion after the initial electrical cardioversion, and longer MPWD and IACT (Fig. 3) compared to those without AF recurrences.
Box plot graph of the interatrial conduction time measurements in the 56 patients with atrial fibrillation recurrences and 57 without atrial fibrillation recurrences after the initial procedure. The horizontal black line and box correspond to the median and interquartile ranges, respectively. The whiskers represent the range; the dots correspond to outliers
Details of the repeat ablation
The details of the repeat ablation procedures are summarized in Table 2. Among the 56 patients with AF recurrences, 45 underwent second procedures after a median of a 6-month interval from the initial procedure. During the second procedure, recovered LA-PV conduction was found in 42 patients (93%), and recovered right atrium-SVC conduction in 36 (80%), but those were all re-isolated. There were 12 ATs and 2 PACs induced and successfully ablated. After the second procedure, 17 patients had AF recurrences and among those, 4 underwent a third procedure. In the third procedure, 2 patients required a re-PVI and one a re-SVC isolation. Four ATs and one PAC were induced and successfully ablated. During a mean follow-up of 20.9 months after the last procedure, there were 89 patients (79%) who had no AF recurrences without AADs.
Predictive value of the IACT
To study the discriminative performance of the IACT and MPWD in order to predict an AF recurrence after the initial CPVI, receiver operator characteristic (ROC) curve analyses were performed. The area under the ROC curve for the IACT was 0.73 (95% CI 0.63–0.82, p < 0.001) and best discriminative cut-off value for the IACT was 123 ms (sensitivity 53%, specificity 85%). On the other hand, the area under the ROC curve for the MPWD was 0.68 (95% CI: 0.62–0.81, p < 0.001) and best discriminative cutoff value for the MPWD was 126 ms (sensitivity 64%, specificity 71%).
For analyzing the predictors of an AF recurrence after the initial CPVI, both a univariate and multivariate analysis were performed using a Cox proportional hazards model (Table 3). In the univariate analysis, the BMI, presence of hypertension, LAV, and prolonged IACTs ≥ 123 ms, and MPWDs ≥ 126 ms were significantly associated with AF recurrences (Table 3). In the multivariate analysis, both the prolonged IACTs and MPWDs demonstrated they were independent predictors of AF recurrences, whereas a prolonged IACT (adjusted hazard ratio [HR]: 2.38, 95% confidence interval [CI]: 1.36–4.16, p = 0.002) had a markedly smaller p value than a prolonged MPWD (adjusted HR: 2.23, 95% CI: 1.20–4.15, p = 0.01) (Table 4). Furthermore, when analyzing the incremental AF recurrence rate per 10ms IACT, increasing the IACT by 10 ms demonstrated a 30% likelihood of an incremental AF recurrence rate (p = 0.004).
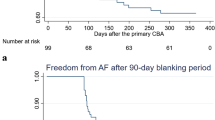
In creating the Kaplan–Meier curve for the analysis of the incidence of an AF recurrence without any AADs according to a cut-off for an IACT of 123 ms, patients with an IACT ≥ 123 ms had a significantly lower AF-free survival rate after the initial procedure than those with an IACT < 123 ms (p < 0.0001) (Fig. 4a). Even after the last procedure, patients with an IACT ≥ 123 ms still had a significantly lower AF-free survival rate compared to those with an IACT < 123 ms (p = 0.002) (Fig. 4b).
Kaplan–Meier survival curve for the freedom from atrial fibrillation recurrence without any antiarrhythmic drugs according to a cut-off value of the IACT of 123 ms. a After the initial procedure. b After the last procedure. Solid line: patients with an IACT < 123 ms. Dotted line: patients with an IACT ≥ 123 ms. IACT interatrial conduction time
Correlations between the IACT measurements and MPWD
There were 92 patients in whom an IACT could be measured before undergoing the CPVI after the initial electrical cardioversion (Fig. 2). Among those, 41 patients had an AF recurrence and the remaining 51 had no AF recurrences after the initial procedure. Even at this point of the measurement, the patients with AF recurrences also had a significantly longer IACT compared to those without AF recurrences (125.2 ± 16.6 ms vs. 111.3 ± 14.5 ms, respectively, p < 0.001). In analyzing the mean IACT between that before and after the CPVI, there was no significant difference between the two measurements (118.1 ± 15.8 ms vs. 119.1 ± 14.8 ms, respectively, p = 0.12). In the Spearman correlation test, there was a strong correlation between the IACT before the CPVI and that after the CPVI (Spearman r = 0.79, p < 0.001) (Fig. 5a).
Furthermore, in analyzing the correlation between the IACT and MPWD, there was also a strong correlation between the two measurements (Spearman r = 0.89, p < 0.001) (Fig. 5b).
Correlation between the interatrial conduction time (IACT) measured after achieving a circumferential pulmonary vein isolation (CPVI) and a the IACT measured before undergoing the CPVI and b the max P-wave duration measured after achieving the CPVI. IACT interatrial conduction time, MPWD max P-wave duration
Intra-rater reliability and inter-rater reliability of measuring the IACT and MPWD
Table 5 shows the inter-rater and intra-rater ICCs for the measurements of the IACT and MPWD. The intra-rater ICC score was high for measuring both the IACT (0.86, 95% CI 0.75–0.91) and MPWD (0.88, 95% CI 0.83–0.92), suggesting a strong reliability. However, in the inter-rater ICC analysis, the score was higher only for the measurement of the IACT (0.89, 95% CI 0.80–0.91), suggesting a poorer inter-rater reliability for measuring the MPWD (0.61, 95% CI 0.33–0.77).
Discussion
Major findings
The present study investigated the value of a procedural electrophysiological assessment using the IACT to predict AF recurrences after the CPVI in patients with PerAF. The main findings were that a prolonged IACT of ≥ 123 ms was independently associated with an AF recurrence after the initial CPVI with a strong intra-rater and inter-rater reliability, and it had a 2.4-fold increase in the probability of a recurrence of AF as compared to that with an IACT of < 123 ms. Patients with an IACT ≥ 123 ms still had a higher AF recurrence rate even after multiple CPVI procedures. No matter when the IACT was measuring before undergoing the CPVI, the results did not significantly differ from those measured after achieving the CPVI. Furthermore, though the MPWD was also demonstrated to have an independent predictive value for an AF recurrence, the inter-rater reliability seemed to be relatively poorer than that of measuring the IACT.
Significance of assessing the IACT during the CPVI without an extensive substrate modification
In the Substrate and Trigger Ablation for Reduction (STAR) of AF II trial [1], an empirical extensive substrate modification targeting roof and mitral isthmus linear lesions or complex fractionated electrograms could not improve the cure rate as compared to PVI alone. That result suggested that an extensive substrate modification was not always required in patients with PerAF. However, in our present study, there was still a significantly higher AF recurrence rate in the cases with a prolonged IACT even after undergoing multiple CPVI procedures compared to those without a prolonged IACT. As shown by our results, the LA-PV reconnections were almost always only seen after one CPVI procedure [1,2,3]. However, the probability of a durable PVI may increase after multiple CPVI procedures. Our finding suggested that patients with a prolonged IACT might be associated with a limited efficacy after only a durable CPVI.
A large number of reports have indicated that advanced atrial remodeling seems to be highly associated with an AF recurrence after the procedure [2,4,6,8,16]. Ausma et al. reported that the total atrial conduction time might integrate the atrial dimension and electrical properties of the atrial [17]. A prolonged IACT may reflect a more comprehensive estimation of both advanced structural and electrical atrial remodeling. This may be associated with a stronger discriminative power to detect those who have a more advanced atrial substrate than the previous parameters.
Recently, several reports have suggested that in the case of progressive atrial remodeling, an extensive substrate modification targeting low-voltage areas might improve the success rate in patients with PerAF [18,19]. Chao et al. previously reported that a prolonged total atrial conduction time might be associated with a decreased atrial voltage [17]. Without creating a voltage map in all patients, evaluating the IACT may be helpful in detecting those who have progressive atrial remodeling and in whom it would be worthwhile to undergo a voltage-guided ablation. Furthermore, an extensive substrate modification often requires a longer procedure time and multiple procedures to achieve success [1,4,5]. Therefore, measuring the IACT and easily selecting whether the patients would have a better efficacy with only a CPVI, or would have a limited efficacy with only a CPVI and be favorable to consider for an extensive substrate modification from the initial procedure, may be feasible not only to save procedural time, but also to improve the outcome.
Prolonged IACT of ≥ 123 ms
In the current study, the best discriminative cut-off value for the IACT to predict an AF recurrence was 123 ms. Wang et al. performed a systemic review and meta-analysis to clarify the utilization of a prolonged P-wave duration (PWD) in the prediction of AF recurrences after ablation procedures [7]. They reported that though the best criterion of a prolonged PWD varied between the studies [7,8,9], a PWD measured after the ablation procedure of > 120 ms may suggest a higher risk of recurrence in patients who undergo catheter ablation of AF. However, that data mostly consisted of studies that were targeting patients with PAF. Blanche et al. reported that the PWD was shorter in patients with PAF compared to that in those with PerAF [8].
In the present study, a cut-off value of 123 ms did not have either a high sensitivity or specificity. Further studies are required to clarify the optimal criterion of what defines “prolonged” as associated with this new IACT parameter for patients with PerAF.
Clinical advantages of measuring the IACT
Recently, the signal-averaged electrogram [7,8] and tissue Doppler imaging using transthoracic echocardiography [9,10] have been established as useful modalities for evaluating the total atrial conduction time. However, those methods have limitations regarding their use in all clinical situations, in that the signal-averaged electrogram requires special hardware and tissue Doppler imaging requires transthoracic echocardiography skills. In contrast, measuring the IACT does not require any specific equipment besides the basic set up for AF ablation. The direct cumulative atrial depolarization from the onset at the sinus node to the last left atrial activation can be quickly and easily measured during the procedures and also directly reflects the ongoing ablation strategy.
Furthermore, for measuring the atrial conduction time in patients with PerAF, conversion and maintenance of sinus rhythm are required. However, in the present study, 19% of the patients had immediate AF recurrences after the electrical cardioversion and it was difficult to measure the atrial conduction time. In contrast, all patients could maintain sinus rhythm after achieving the CPVI. Measuring the IACT after achieving the CPVI has a greater advantage than the pre-procedural measurement parameters in that it might be less difficult to maintain sinus rhythm in patients with PerAF. However, in our results, the IACTs measured before the CPVI did not differ from those measured after the CPVI. This finding suggested that measuring the IACT at the beginning of the procedure might also be considered in some cases in which it might be favorable.
Measuring the MPWD during the procedure might also be a useful parameter for predicting patients who would have AF recurrences. However, discriminating the precise border between the baseline and end of the P-Wave is sometimes difficult because of the gradual slope of the P-wave [7,8]. This might be more often seen in patients with PerAF who have more progressive remodeled atria. This limitation might affect the inter-rater difference when measuring the MPWD. In contrast, since the local potentials on the intracardiac electrograms are easier to distinguish, the IACT might be measured with a minimal intra and inter-rater difference.
Limitations
Several limitations must be taken into account when interpreting this study. First, the present study was a retrospective study and was comprised of a relatively small group of patients. Furthermore, our cut off level had a relatively low sensitivity. Therefore, the present findings need to be validated in a larger group of patients. Second, since not all subclinical recurrences of AF could be completely detected, we may have underestimated the recurrences. However, we tried to reduce this error by strongly instructing all patients to assess their daily pulse. Third, since the IACT was affected by the catheter position in the coronary sinus, some measurements might have been underestimated. However, since this bias would have been equally distributed in both the groups with and without recurrences, it would not have strongly affected the comparison of the two groups. Fourth, there were some patients who did not undergo repeat procedures despite AF recurrences and that may have had an affect on the cure rates after multiple procedures. However, in the present study, the AF recurrence free rate was 79% after multiple procedures. Compared to the previous reports [1,2,3,4,5], we think this may be an acceptable result regarding the efficacy of a triggered ablation, including a CPVI and SVC isolation, without an extensive substrate modification.
Conclusions
A prolonged IACT of ≥ 123 ms may have a higher degree of discrimination for predicting patients who would have AF recurrences after the initial CPVI of PerAF. A prolonged IACT might also contribute to detecting patients who would have AF recurrences even after multiple CPVIs. This simple and practical parameter may help to select patients who are inappropriate for being treated with only a CPVI and in whom optimization of the ablation strategy of PerAF is required.
References
Verma A, Jiang CY, Betts TR, Chen J, Deisenhofer I, Mantovan R, Macle L, Morillo CA, Haverkamp W, Weerasooriya R, Albenque JP, Nardi S, Menardi E, Novak P, Sanders P, Investigators STARAFII (2015) Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med 372:1812–1822
Tilz RR, Rillig A, Thum AM, Arya A, Wohlmuth P, Metzner A, Mathew S, Yoshiga Y, Wissner E, Kuck KH, Ouyang F (2012) Catheter ablation of long-standing persistent atrial fibrillation: 5-year outcomes of the Hamburg Sequential Ablation Strategy. J Am Coll Cardiol 60:1921–1929
Higuchi S, Sohara H, Nakamura Y, Ihara M, Yamaguchi Y, Shoda M, Hagiwara N, Satake S (2016) Is it necessary to achieve a complete box isolation in the case of frequent esophageal temperature rises? Feasibility of shifting to a partial box isolation strategy for patients with non-paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 27:897–904
Jaïs P, Hocini M, Hsu LF, Sanders P, Scavee C, Weerasooriya R, Macle L, Raybaud F, Garrigue S, Shah DC, Le Metayer P, Clémenty J, Haïssaguerre M (2004) Technique and results of linear ablation at the mitral isthmus. Circulation 110:2996–3002
Nademanee K, McKenzie J, Kosar E, Schwab M, Sunsaneewitayakul B, Vasavakul T, Khunnawat C, Ngarmukos T (2004) A new approach for catheter ablation of atrial fibrillation: mapping of the electrophysiologic substrate. J Am Coll Cardiol 43:2044–2053
Scherr D, Khairy P, Miyazaki S, Aurillac-Lavignolle V, Pascale P, Wilton SB, Ramoul K, Komatsu Y, Roten L, Jadidi A, Linton N, Pedersen M, Daly M, O'Neill M, Knecht S, Weerasooriya R, Rostock T, Manninger M, Cochet H, Shah AJ, Yeim S, Denis A, Derval N, Hocini M, Sacher F, Haissaguerre M, Jais P (2015) Five-year outcome of catheter ablation of persistent atrial fibrillation using termination of atrial fibrillation as a procedural endpoint. Circ Arrhythm Electrophysiol 8:18–24
Wang YS, Chen GY, Li XH, Zhou X, Li YG (2017) Prolonged P-wave duration is associated with atrial fibrillation recurrence after radiofrequency catheter ablation: a systematic review and meta-analysis. Int J Cardiol 227:355–359
Blanche C, Tran N, Rigamonti F, Burri H, Zimmermann M (2013) Value of P-wave signal averaging to predict atrial fibrillation recurrences after pulmonary vein isolation. Europace 15:198–204
Chao TF, Sung SH, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Suenari K, Li CH, Ueng KC, Wu TJ, Chen SA (2011) Associations between the atrial electromechanical interval, atrial remodelling and outcome of catheter ablation in paroxysmal atrial fibrillation. Heart 97:225–230
Ejima K, Kato K, Arai K, Fukushima K, Fukushima N, Suzuki T, Yoshida K, Nuki T, Uematsu S, Hoshi H, Manaka T, Ashihara K, Shoda M, Hagiwara N (2014) Impact of atrial remodeling on the outcome of radiofrequency catheter ablation of paroxysmal atrial fibrillation. Circ J 78:872–877
Mugnai G, Chierchia GB, de Asmundis C, Juliá J, Conte G, Sieira-Moret J, Capulzini L, Wauters K, Rodriguez-Mañero M, Ciconte G, Baltogiannis G, Di Giovanni G, Saitoh Y, Brugada P (2016) P-wave indices as predictors of atrial fibrillation recurrence after pulmonary vein isolation in normal left atrial size. J Cardiovasc Med (Hagerstown) 17:194–200
Deftereos S, Kossyvakis C, Efremidis M, Bouras G, Panagopoulou V, Papadimitriou C, Doudoumis K, Deftereos G, Synetos A, Davlouros P, Toutouzas K, Alexopoulos D, Manolis AS, Giannopoulos G (2014) Interatrial conduction time and incident atrial fibrillation: a prospective cohort study. Heart Rhythm 11:1095–1101
Henmi R, Ejima K, Shoda M, Yagishita D, Hagiwara N (2016) Interatrial Conduction Time Can Predict New-Onset Atrial Fibrillation After Radiofrequency Ablation of Isolated, Typical Atrial Flutter. J Cardiovasc Electrophysiol 27:1293–1297
Calkins H, Kuck KH, Cappato R, Brugada J, Camm AJ, Chen SA, Crijns HJ, Damiano RJ Jr, Davies DW, DiMarco J, Edgerton J, Ellenbogen K, Ezekowitz MD, Haines DE, Haissaguerre M, Hindricks G, Iesaka Y, Jackman W, Jalife J, Jais P, Kalman J, Keane D, Kim YH, Kirchhof P, Klein G, Kottkamp H, Kumagai K, Lindsay BD, Mansour M, Marchlinski FE, McCarthy PM, Mont JL, Morady F, Nademanee K, Nakagawa H, Natale A, Nattel S, Packer DL, Pappone C, Prystowsky E, Raviele A, Reddy V, Ruskin JN, Shemin RJ, Tsao HM, Wilber D (2012) 2012 HRS/EHRA/ECAS Expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace 14:528–606
Ejima K, Henmi R, Iwanami Y, Yagishita D, Shoda M, Hagiwara N (2017) Comparison of the efficacy of empiric thoracic vein isolation for the treatment of paroxysmal and persistent atrial fibrillation in patients without structural heart disease. J Cardiovasc Electrophysiol 28:266–272
Abecasis J, Dourado R, Ferreira A, Saraiva C, Cavaco D, Santos KR, Morgado FB, Adragão P, Silva A (2009) Left atrial volume calculated by multi-detector computed tomography may predict successful pulmonary vein isolation in catheter ablation of atrial fibrillation. Europace 11:1289–1294
Ausma J, Litjens N, Lenders MH, Duimel H, Mast F, Wouters L, Ramaekers F, Allessie M, Borgers M (2001) Time course of atrial fibrillation-induced cellular structural remodeling in atria of the goat. J Mol Cell Cardiol 33:2083–2094
Jadidi AS, Lehrmann H, Keyl C, Sorrel J, Markstein V, Minners J, Park CI, Denis A, Jaïs P, Hocini M, Potocnik C, Allgeier J, Hochholzer W, Herrera-Sidloky C, Kim S, Omri YE, Neumann FJ, Weber R, Haïssaguerre M, Arentz T (2016) Ablation of Persistent Atrial Fibrillation Targeting Low-Voltage Areas With Selective Activation Characteristics. Circ Arrhythm Electrophysiol. https://doi.org/10.1161/CIRCEP.115.002962
Masuda M, Fujita M, Iida O, Okamoto S, Ishihara T, Nanto K, Kanda T, Shiraki T, Sunaga A, Matsuda Y, Uematsu M (2016) Influence of underlying substrate on atrial tachyarrhythmias after pulmonary vein isolation. Heart Rhythm 13:870–888
Acknowledgements
We would like to thank Mr. John Martin for his linguistic assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Higuchi, S., Ejima, K., Shoda, M. et al. Impact of a prolonged interatrial conduction time for predicting the recurrence of atrial fibrillation after circumferential pulmonary vein isolation of persistent atrial fibrillation. Heart Vessels 34, 616–624 (2019). https://doi.org/10.1007/s00380-018-1272-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1272-8