Abstract
The ratio of serum eicosapentaenoic acid (EPA) to arachidonic acid (AA) is significantly associated with long-term clinical outcomes in patients with acute myocardial infarction (AMI). However, it has not been conclusively demonstrated that higher serum EPA/AA ratio fares better clinical outcomes in the early phase of AMI. The Japanese registry of acute Myocardial INfarction diagnosed by Universal dEfiniTion (J-MINUET) is a prospective multicenter registry conducted in 28 Japanese medical institutions between July 2012 and March 2014. We enrolled 3,283 consecutive AMI patients who were admitted to participating institutions within 48 h of symptom onset. A serum EPA/AA ratio was available for 629 of these patients. The endpoints were in-hospital mortality and major adverse cardiac events (MACE), defined as a composite of all cause death, cardiac failure, ventricular tachycardia (VT) and/or ventricular fibrillation (VF) and bleeding during hospitalization. Although similar rates of in-hospital mortality, cardiac failure, bleeding, and MACE were found in the lower serum EPA/AA group and higher serum EPA/AA group, the incidence of VT/VF during hospitalization was significantly higher in the low ratio group (p = 0.008). Receiver operating characteristic curve analysis showed that an EPA/AA ratio < 0.35 could predict the incidence of VT/VF with 100% sensitivity and 64.0% specificity. A lower serum EPA/AA ratio was associated with a higher frequency of fatal arrhythmic events in the early phase of AMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have shown that consumption of fish and fish oil containing n-3 polyunsaturated fatty acids (PUFAs), including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), can reduce the risk of cardiovascular events [1,2,3,4]. The Japan EPA Lipid Intervention Study (JELIS) [5] reported that pure EPA treatment decreased the incidence of major cardiac events by 19% in hypercholesterolemic patients undergoing statin treatment. A secondary prevention analysis from JELIS found that the incidence of sudden cardiac death (SCD) and myocardial infarction (MI) was lower in the high serum EPA/arachidonic acid (AA) ratio group than that in the low ratio group [6]. A clinical trial demonstrated that a serum EPA/AA ratio > 0.4 was associated with a significantly lower incidence of major cardiac events in patients who had undergone elective percutaneous coronary intervention (PCI) due to angina pectoris [7]. However, it has not yet been fully demonstrated that a higher serum EPA/AA ratio results in improved clinical outcomes in the early phase of acute myocardial infarction (AMI). The aim of this study was to investigate the relationship between the EPA/AA ratio and in-hospital clinical outcomes in patients with AMI.
Materials and methods
Study design and subjects
The Japanese registry of acute Myocardial INfarction diagnosed by Universal dEfiniTion (J-MINUET) is a prospective multicenter registry conducted in 28 Japanese medical institutions [8]. We enrolled 3,283 consecutive patients with AMI who were admitted to participating institutions within 48 h of symptom onset between July 2012 and March 2014. Twelve out of 28 institutions participated in EPA/AA ratio substudy. Diagnosis of AMI was based on the ESC/ACC Foundation/American Heart Association/World Heart Federation Task Force for the Universal Definition of Myocardial Infarction [9]. AMI was diagnosed by the rise and/or fall of cardiac biomarkers with at least 1 value above the 99th percentile of the upper reference limit observed together with evidence of myocardial ischemia with at least one of the following: symptoms of ischemia, electrocardiography (ECG) changes indicative of new ischemia, development of pathological Q waves in the ECG, or imaging evidence of a new loss of viable myocardium or new regional wall motion abnormalities. ST-elevation MI (STEMI) was diagnosed in the presence of a new ST elevation at the J point in at least two contiguous leads ≥ 2 mm (0.2 mV) in men or ≥ 1.5 mm (0.15 mV) in women in leads V2–3 and/or ≥ 1 mm (0.1 mV) in other contiguous chest leads or limb leads [10, 11]. A new left bundle branch block was considered as a STEMI equivalent. Patients were evaluated for baseline clinical characteristics, laboratory data, and medication on admission. Clinical events were collected at the time of discharge.
The endpoints were in-hospital mortality and major adverse cardiac events (MACE), defined as a composite of all cause death, cardiac failure, ventricular tachycardia (VT) and/or ventricular fibrillation (VF), and bleeding during hospitalization. Cardiac failure was defined as congestive heart failure and/or cardiogenic shock requiring treatment. VT/VF was detected from documentation of continuous ECG monitoring. VT encompassed only sustained VT, which was defined as VT lasting > 30 s and at least 150 beats/min, and/or accompanied by hemodynamic compromise requiring electrical cardioversion or anti-arrhythmic therapy. The study was conducted in accordance with the Declaration of Helsinki, and the test protocol was approved by the ethics committees of every participating institution.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and compared using the unpaired t test or the Wilcoxon rank sum test. Categorical variables were presented as numbers and frequencies and compared using the Chi square test. A univariate logistic regression model was used to assess the predictor of VT/VF. A p < 0.05 was used to indicate statistical significance. A receiver operating characteristic (ROC) curve was constructed to identify optimal EPA/AA cutoff points and true-positive (sensitivity) and false-positive rates (1-specificity) of EPA/AA for predicting VT/VF. All analyses were performed using JMP version 12.0.1 for Windows (SAS, North Carolina, USA).
Results
Baseline and procedural characteristics
A total of 629 patients were enrolled in the J-MINUET EPA/AA ratio substudy. All patients were undergone urgent coronary angiography and PCI. Out of these, 527 (83.8%) were diagnosed with STEMI and 102 (16.2%) with non-STEMI. The EPA/AA ratio ranged from 0.03 to 2.10, with a mean standard deviation of 0.35 ± 0.24 and a median of 0.28. In the previous study, a serum EPA/AA ratio > 0.4 was associated with a significantly lower incidence of MACE in patients who had undergone elective PCI due to angina pectoris [7]. Therefore, we divided the patients into lower (EPA/AA < 0.4, n = 448) and higher (EPA/AA ≥ 0.4, n = 181) groups.
The baseline characteristics from the EPA/AA ratio are shown in Table 1. A lower serum EPA/AA ratio was associated with a younger age, lower systolic blood pressure, higher hemoglobin, lower high-density lipoprotein cholesterol, and higher low-density lipoprotein cholesterol (Table 1). Procedural characteristics and outcomes are shown in Table 2. No significant differences were found between the lower and higher serum EPA/AA ratio groups.
In-hospital clinical outcomes
Table 3 shows the in-hospital clinical outcomes. Although the two groups were similar in rates of in-hospital mortality, cardiac failure, bleeding, and MACE, the incidence of VT/VF while hospitalized was significantly higher in the lower serum EPA/AA group (p = 0.008). All 17 patients in whom VT/VF occurred showed low serum EPA/AA ratio. Periprocedural VT/VF was observed in eight patients (47%).
Logistic regression analysis of independent factors related to VT/VF
Logistic regression analysis identified higher peak creatine kinase (CK), pre-procedural thrombolysis in myocardial infarction (TIMI) flow grade 0, Killip class 2–4, and lower serum EPA/AA ratio as significant correlates of VT/VF (Table 4).
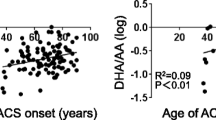
ROC curve for the incidence of VT/VF using the EPA/AA ratio
Figure 1 shows the ROC curve for the incidence of VT/VF using the EPA/AA ratio. ROC analysis showed that the EPA/AA ratio could predict the incidence of VT/VF with 100% sensitivity and 64.0% specificity at a cutoff value of 0.35 (area under the curve: 0.66).
Discussion
The study demonstrated a significantly higher incidence of VT/VF in patients with lower serum EPA/AA ratio than those with higher serum EPA/AA ratio, in the early phase of AMI.
It is well known that n-6 PUFAs such as AA promote atherosclerosis after being transformed into eicosanoids, whereas n-3 PUFAs such as EPA and DHA play an important role in the prevention of coronary artery disease [12]. Itakura et al. [13] demonstrated that EPA/AA ratios > 0.75 are associated with significantly fewer major coronary events [hazard ratio (HR) 0.83; 95% confidence interval (CI) 0.69–0.98; p = 0.031]. Nishizaki et al. [14] reported that patients with EPA/AA ratios ≤ 0.33 had a greater probability of acute coronary syndrome (odds ratio 3.14; 95% CI 1.16–8.49). The serum EPA/AA ratio is, therefore, considered to be a marker of coronary artery disease.
In our study, a lower serum EPA/AA ratio was associated with life-threatening ventricular arrhythmias during the early phase of AMI; however, no clear association was observed with short-term mortality or MACE. The incidence of VT/VF might be too low to affect short-term mortality and MACE. Ventricular arrhythmia is a major complication of AMI and is associated with poor in-hospital and long-term clinical outcomes [15, 16]. Several studies have shown that consumption of n-3 PUFAs significantly decreases the incidence of major cardiac events, especially SCD, in patients with ischemic heart disease. In the Gruppo Italiano per la Sperimentazione della Streptochinasi nell’Infarto Miocardico (GISSI) Prevenzione trial [3], post-MI patients taking n-3 PUFA supplement (1 capsule per day providing 850 mg of EPA/DHA in a 1.2:1 ratio) showed a 21 and 30% reduction in total and cardiovascular mortality, respectively. The reduction in risk of SCD was specifically shown to be statistically significant as early as 4 months [relative risk (RR) 0.47; 95% CI 0.219–0.995; p = 0.048], and became strongly statistically significant at 42 months (RR 0.55; 95% CI 0.39–0.77; p = 0.0006). A subgroup analysis from the GISSI Prevenzione trial [17] showed a significant increase in SCD with worsening of the left ventricular systolic function, with SCD in patients with an ejection fraction (EF) ≤ 40% being four times higher than in patients with EF > 50%. In a secondary prevention analysis from JELIS, 3,664 patients with coronary artery disease and hypercholesterolemia were randomly assigned to treatment with statin alone or statin and highly purified EPA at 1,800 mg/day [6]. At the end of the 5-year study, the EPA group showed a 23% lower incidence of major coronary events. The incidence of SCD or MI was significantly lower (adjusted HR 0.58; p = 0.038) in the highest EPA/AA ratio (≥ 1.06) group than in the lowest ratio (≤ 0.55) group.
However, recent randomized trials and meta-analyses of patients after MI have failed to demonstrate a favorable effect on cardiovascular events. The OMEGA trial was presented that assessed n-3 PUFAs for 12 months 3,851 patients within 3–14 days after AMI in addition to guideline-adjusted treatment [18]. Relative to the whole study population, the rate of SCD during follow-up was 1.5%, same as that of the control group (n-3 PUFAs group, 1.5%; control group, 1.5%; p = 0.84; odds ratio, 0.95; 95% CI 0.56–1.60). The Alpha Omega trial involving patients who had an MI and who were receiving good clinical care similarly showed no effect of low doses of n-3 PUFAs in significantly reducing the cardiovascular end points [19].
The failure of n-3 PUFA treatment to show any favorable effect on SCD in these studies has several possible explanations. First, the trials might have been underpowered for detecting significant reductions in SCD. Post-MI therapy using statins has improved considerably over the past years, resulting in low rates of SCD or other cardiovascular events following MI. Second, the EPA dosage was different in each study. The JELIS trial used a daily dose of 1800 mg, the OMEGA trial 460 mg, and the Alpha Omega trial 226 mg. In addition, the baseline blood levels of n-3 PUFAs differed significantly between the studies.
We speculate that the arrhythmia protection conferred by n-3 PUFAs may be stronger in the early phase of AMI. The mechanism of ventricular arrhythmia in the early phase is different from that in the late phase. In the early phase, it is due to myocardial ischemia and reperfusion injury [20,21,22]. During an acute ischemic event, a gradient of depolarization of cardiomyocytes arises within the ischemic tissue, and this can trigger ventricular arrhythmias. The theoretical anti-arrhythmic mechanism of n-3 PUFAs is the electrical stabilization of the cardiac myocyte by modulating the conductance of the sodium and calcium ion channels in the sarcolemma, which may prevent arrhythmias arising in the ischemic zone [23, 24]. Recent studies have shown that the median time to ventricular arrhythmia after PCI in patients with AMI is less than 5 days [21, 22]. Reperfusion VF accounted for 22% of VF occurring within the first 48 h of STEMI, when treated by primary PCI [25]. In our study, periprocedural VF was observed in eight patients (47%). Previous case–control studies suggested that high levels of n-3 PUFAs are able to protect against VF during the acute ischemic phase of AMI. Aarsetøy et al. [26] demonstrated that a 1% increase in the omega-3 index was associated with a 48% reduction in risk of VF during the ischemic phase of AMI. Doi et al. [27] reported that EPA treatment applied within 24 h of PCI in the acute stage of MI reduced the rate of adverse clinical events, including ventricular arrhythmias. The present study demonstrated that high EPA/AA ratios may be associated with a decrease in ventricular arrhythmias in patients with AMI, especially in the early phase.
This study had a number of limitations. First, there may have been selection bias in the patients who participated because J-MINUET is not a population-based study, and the serum EPA/AA ratio was available for only 629 of the 3,283 patients. Second, the number of patients in the study was relatively small, so that factors related to VT/VF were confined to univariate analysis. Larger-scale studies should be conducted to better evaluate the relationship between the serum EPA/AA ratio and cardiac events such as SCD, MI, or arrhythmia.
A lower serum EPA/AA ratio was associated with fatal arrhythmic events in the early phase of AMI. Our findings suggest that a high EPA/AA ratio has an anti-arrhythmic effect in the acute ischemic phase of AMI.
References
Hu FB, Bronner L, Willett WC, Stampfer MJ, Rexrode KM, Albert CM, Hunter D, Manson JE (2002) Fish and omega-3 fatty acid intake and risk of coronary heart disease in women. JAMA 287:1815–1821
Iso H, Kobayashi M, Ishihara J, Sasaki S, Okada K, Kita Y, Kokubo Y, Tsugane S (2006) Intake of fish and n3 fatty acids and risk of coronary heart disease among Japanese: the Japan Public Health Center-Based (JPHC) Study Cohort I. Circulation 113:195–202
Marchioli R (2002) Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI)-Prevenzione. Circulation 105:1897–1903
Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, Elwood PC, Deadman NM (1989) Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet 2:757–761
Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K (2007) Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet 369:1090–1098
Matsuzaki M, Yokoyama M, Saito Y, Origasa H, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K, Matsuzawa Y (2009) Incremental effects of eicosapentaenoic acid on cardiovascular events in statin-treated patients with coronary artery disease. Circ J 73:1283–1290
Domei T, Yokoi H, Kuramitsu S, Soga Y, Arita T, Ando K, Shirai S, Kondo K, Sakai K, Goya M, Iwabuchi M, Ueeda M, Nobuyoshi M (2012) Ratio of serum n-3 to n-6 polyunsaturated fatty acids and the incidence of major adverse cardiac events in patients undergoing percutaneous coronary intervention. Circ J 76:423–429
Ishihara M, Fujino M, Ogawa H, Yasuda S, Noguchi T, Nakao K, Ozaki Y, Kimura K, Suwa S, Fujimoto K, Nakama Y, Morita T, Shimizu W, Saito Y, Tsujita K, Nishimura K, Miyamoto Y, J-MINUET investigators (2015) Clinical presentation, management and outcome of Japanese patients with acute myocardial infarction in the troponin era—Japanese registry of acute myocardial infarction diagnosed by universal definition (J-MINUET). Circ J 79:1255–1262
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BR, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow JJ, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Morais J, Aguiar C, Almahmeed W, Arnar DO, Barili F, Bloch KD, Bolger AF, Botker HE, Bozkurt B, Bugiardini R, Cannon C, de Lemos J, Eberli FR, Escobar E, Hlatky M, James S, Kern KB, Moliterno DJ, Mueller C, Neskovic AN, Pieske BM, Schulman SP, Storey RF, Taubert KA, Vranckx P, Wagner DR (2012) Third universal definition of myocardial infarction. J Am Coll Cardiol 60:1581–1598
Alpert JS, Thygesen K, Antman E, Bassand JP (2000) Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36:959–969
American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61(4):e78–140
Harris WS, Assaad B, Poston WC (2006) Tissue omega-6/omega-3 fatty acid ratio and risk for coronary artery disease. Am J Cardiol 98(4A):19i–26i
Itakura H, Yokoyama M, Matsuzaki M, Saito Y, Origasa H, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K, Matsuzawa Y (2011) Relationships between plasma fatty acid composition and coronary artery disease. J Atheroscler Thromb 18:99–107
Nishizaki Y, Shimada K, Tani S, Ogawa T, Ando J, Takahashi M, Yamamoto M, Shinozaki T, Miyauchi K, Nagao K, Hirayama A, Yoshimura M, Komuro I, Nagai R, Daida H (2014) Significance of imbalance in the ratio of serum n-3 to n-6 polyunsaturated fatty acids in patients with acute coronary syndrome. Am J Cardiol 113:441–445
Al-Khatib SM, Granger CB, Huang Y, Lee KL, Califf RM, Simoons ML, Armstrong PW, Van de Werf F, White HD, Simes RJ, Moliterno DJ, Topol EJ, Harrington RA (2002) Sustained ventricular arrhythmias among patients with acute coronary syndromes with no ST-segment elevation: incidence, predictors, and outcomes. Circulation 106:309–312
Gibson CM, Pride YB, Buros JL, Lord E, Shui A, Murphy SA, Pinto DS, Zimetbaum PJ, Sabatine MS, Cannon CP, Josephson ME (2008) Association of impaired thrombolysis in myocardial infarction myocardial perfusion grade with ventricular tachycardia and ventricular fibrillation following fibrinolytic therapy for ST-segment elevation myocardial infarction. J Am Coll Cardiol 51:546–551
Macchia A, Levantesi G, Franzosi MG, Geraci E, Maggioni AP, Marfisi R, Nicolosi GL, Schweiger C, Tavazzi L, Tognoni G, Valagussa F, Marchioli R, Investigators GI-P (2005) Left ventricular systolic dysfunction, total mortality, and sudden death in patients with myocardial infarction treated with n-3 polyunsaturated fatty acids. Eur J Heart Fail 7:904–909
Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, Gottwik M, Steinbeck G, Del Castillo U, Sack R, Worth H, Katus H, Spitzer W, Sabin G, Senges J, Group OS (2010) OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation 122:2152–2159
Kromhout D, Giltay EJ, Geleijnse JM (2010) n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med 363:2015–2026
Mehta RH, Harjai KJ, Grines L, Stone GW, Boura J, Cox D, O’Neill W, Grines CL, Primary Angioplasty in Myocardial Infarction I (2004) Sustained ventricular tachycardia or fibrillation in the cardiac catheterization laboratory among patients receiving primary percutaneous coronary intervention: incidence, predictors, and outcomes. J Am Coll Cardiol 43:1765–1772
Mehta RH, Starr AZ, Lopes RD, Hochman JS, Widimsky P, Pieper KS, Armstrong PW, Granger CB (2009) Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA 301:1779–1789
Piccini JP, White JA, Mehta RH, Lokhnygina Y, Al-Khatib SM, Tricoci P, Pollack CV Jr, Montalescot G, Van de Werf F, Gibson CM, Giugliano RP, Califf RM, Harrington RA, Newby LK (2012) Sustained ventricular tachycardia and ventricular fibrillation complicating non-ST-segment-elevation acute coronary syndromes. Circulation 126:41–49
Leaf A, Xiao YF, Kang JX, Billman GE (2003) Prevention of sudden cardiac death by n-3 polyunsaturated fatty acids. Pharmacol Ther 98:355–377
Xiao YF, Ke Q, Chen Y, Morgan JP, Leaf A (2004) Inhibitory effect of n-3 fish oil fatty acids on cardiac Na+/Ca2+ exchange currents in HEK293t cells. Biochem Biophys Res Commun 321:116–123
Demidova MM, Smith JG, Hoijer CJ, Holmqvist F, Erlinge D, Platonov PG (2012) Prognostic impact of early ventricular fibrillation in patients with ST-elevation myocardial infarction treated with primary PCI. Eur Heart J Acute Cardiovasc Care 1:302–311
Aarsetoy H, Ponitz V, Nilsen OB, Grundt H, Harris WS, Nilsen DW (2008) Low levels of cellular omega-3 increase the risk of ventricular fibrillation during the acute ischaemic phase of a myocardial infarction. Resuscitation 78:258–264
Doi M, Nosaka K, Miyoshi T, Iwamoto M, Kajiya M, Okawa K, Nakayama R, Takagi W, Takeda K, Hirohata S, Ito H (2014) Early eicosapentaenoic acid treatment after percutaneous coronary intervention reduces acute inflammatory responses and ventricular arrhythmias in patients with acute myocardial infarction: a randomized, controlled study. Int J Cardiol 176:577–582
Acknowledgements
This study was supported by the Intramural Research Fund, Grant Number 23-4-5, for Cardiovascular Diseases of the National Cerebral and Cardiovascular Center. The authors thank all the enrolled patients, participating cardiologists, medical and other staffs who have contributed to this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Hashimoto, T., Ako, J., Nakao, K. et al. A lower eicosapentaenoic acid/arachidonic acid ratio is associated with in-hospital fatal arrhythmic events in patients with acute myocardial infarction: a J-MINUET substudy. Heart Vessels 33, 481–488 (2018). https://doi.org/10.1007/s00380-017-1084-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-1084-2