Abstract
Although Nobori®, with a bioresorbable polymer and biolimus A9 abluminal coating, has unique characteristics, few data exist regarding endothelialization early after implantation. Fifteen Nobori® and 14 control bare-metal stents (S-stent™) were implanted in 12 pigs. Histopathology of stented segments, inflammation, and intimal fibrin content was evaluated on the 2nd and 14th day after implantation. On the 2nd day, endothelial cells were morphologically and immunohistologically confirmed on the surface of both stents, although some inflammatory cells might be involved. Stent surface endothelialization evaluated with a scanning electron microscope showed partial cellular coverage in both stents. On the 14th day, neointimal thickness and percentage of the neointimal area were significantly lower in Nobori® than in S-stent™ (51.4 ± 4.5 vs. 76.4 ± 23.6 µm, p < 0.05 and 10.8 ± 2.6 vs. 14.1 ± 4.2%, p < 0.01). No significant differences were found in these parameters on the 2nd day (17.3 ± 14.9 vs. 26.7 ± 13.6 µm and 3.7 ± 3.0 vs. 6.7 ± 3.7%), in inflammatory and intimal fibrin content scores. These results demonstrate that endothelialization could occur early after Nobori® implantation with similar inflammatory reaction to bare-metal stents, probably contributing to low frequency of in-stent thrombosis and restenosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drug-eluting stents (DES) have been developed to inhibit the response to vessel wall injury, which is mainly responsible for restenosis after stent implantation [1,2,3]. As a result, restenosis and target-vessel revascularization after DES implantation were reduced to rates below 10% [4, 5]. Even in large-size coronary arteries, including the left main coronary artery, DES reduce the risk for restenosis [6,7,8], but may increase late thrombosis and delay arterial healing. Incomplete endothelialization of the stent struts and positive vessel remodelling due to chronic inflammation might cause this thrombosis; indeed, the persistence of a durable polymer material on first-generation DES after completed drug release might trigger an inflammatory response [9,10,11,12]. This adverse event results in abrupt occlusion of the implanted artery, with a high risk of sudden cardiac death or myocardial infarction [13, 14]. Autopsies of patients who died because of DES thrombosis within 30 days after implantation suggest pathological disorders, such as delayed neointimal healing, incomplete tissue coverage of the stent struts, and chronic inflammation [9, 12, 13, 15, 16].
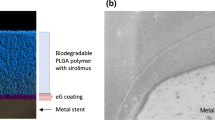
Nobori®, which are abluminally coated with a bioresorbable polymer [polylactic acid (PLA)], and the antiproliferative agent biolimus A9 reduce thrombosis by degradation of the polymer over a period of 9 months [17, 18]. In a long-term follow-up study, Nobori® was related to a significant reduction in very late stent thrombosis and associated composite clinical endpoints [19]. On the other hand, previous reports demonstrated that Nobori® implantation was non-inferior to and not different from everolimus-eluting stent implantation based on 1-year clinical outcomes [20], another report indicated that Nobori® was not superior to first-generation DES [21]. One of the reasons for these controversies can result from few data regarding endothelialization and vessel response early after implantation. Therefore, we compared the appearance of endothelialization after Nobori® and S-stent™ implantation by histologic analysis and scanning electron microscope (SEM) in a porcine model.
Methods
Animal study protocol
The animal study was approved by the Animal Care and Use Committee of Kanazawa University, and the experiments were conducted according to the “Basic Guidelines for Conduct of Animal Experiments” published by the Ministry of Health, Labor and Welfare, Japan.
Nobori® (n = 15) and control S-stent™ (n = 14) were implanted in 12 pigs (mean weight 29.4 ± 2.5 kg) that were followed until the 2nd day or the 14th day (n = 3, each timepoint and stent) after implantation. Nobori® (TERUMO Corporation, Tokyo, Japan) and S-stent™, a platform of Nobori® (BIOSENSORS JAPAN, Tokyo, Japan), with different characteristics were implanted: 11 (length 8 mm and diameter 2.75 mm) and 4 (length 8 mm and diameter 3.0 mm) Nobori®; 7 (length 8 mm and diameter 3.0 mm); and 7 (length 11 mm and diameter 3.0 mm) S-stent™. Both types of stents were made of 316L stainless steel. Nobori® is coated with Biolimus A9 which is a lipophilic analogue of sirolimus.
All swine were treated with aspirin (200 mg, Bayer, Land Nordrheine-Westfalen, Germany) and clopidogrel (300 mg, Sanofi Aventis, Gouda, The Netherlands) for pre-procedure. Aspirin (200 mg) and clopidogrel (75 mg) were administered daily until the end of the study. After being anaesthetized with ketamine (20 mg/kg intramuscularly), swine were maintained on general anesthesia with 2% halothane and oxygen. During experimental procedure, we carefully observed anesthesia situation to maintain appropriate sedation. Electrocardiogram and heart rate were continuously monitored by a polygraph recording system (OptiPlex755, Nihon-Kohden, Tokyo, Japan) throughout the entire procedure. Heparin (5000 IU) was administered via the left carotid artery through 7 Fr sheath, and 2000 IU were injected every hour.
Stent deployment was performed by the method previously described previous report [22]. Briefly, stent delivery catheters (6 Fr Heartrail II, JR-4.0 or AL-1.0, TERUMO) were inserted through the sheath and were advanced over the 0.035 guidewire to the left and right coronary artery orifice. After coronary angiography, using intravascular ultrasound, the segments of the left anterior descending artery, left circumflex artery, or right coronary artery were selected to match available stent sizes. Repeated angiograms were obtained immediately after stent implantation, which was performed by inflation with nominal atm of each stent for 20 s. After stent implantation, we also performed intravascular ultrasound to optimize coronary artery stenting after procedures. Under these conditions, if necessary, we performed balloon dilation to optimize coronary stenting. Each animal received 2 or 3 Nobori® and S-stent™ in the coronary artery. Each coronary artery was implanted with a single stent. At the end of the study, the hearts were harvested and processed for SEM and histological analysis. Under these condition, we controlled anesthesia not to response animal pain.
Tissue preparation
The stented vessels and normal coronary artery were perfused with saline and perfusion-fixed with 4% formaldehyde. The stented and normal coronary artery vessels were embedded in GMA resin and N, N-dimethyl aniline. Sections (5–6 µm thick, for a total of 2 sections) were cut using a cemented tungsten carbide knife (RM2245, Leica, Germany), and stained with hematoxylin and eosin (New Histology Science Laboratory Corporation, Tokyo, Japan). The sections were evaluated with an optical microscope (BZ-9000, KEYENCE, Osaka, Japan).
Endothelialization was evaluated by staining with antibodies against the von Willebrand factor (ab6994, abcam, Cambridge, UK), VE-Cadherin (#2500, Cell Signaling Technology, Danvers, MA, USA), and KDR/VEGFR2 (LS-C356165, LifeSpan BioSciences, Seattle, WA, USA). The stented sections (examined and negative control) and normal coronary artery sections (control) were rinsed 3 times with phosphate buffered saline (PBS) and treated with target retrieval solution (S2031, Dako, Tokyo, Japan) according to manufacturer`s instructions. The sections were maintained at a sub-boiling temperature (30 min). Thereafter, the sections were cooled on the bench (30 min) and incubated in 5% normal goat serum blocking solution (143-06561, Wako, Osaka, Japan)/0.3% TritonX-100 in PBS (30 min) and protein block (X0909, Dako, Tokyo, Japan) (30 min). The sections were labeled with anti-von Willebrand factor antibody at a dilution ratio of 1:400, followed by Alexa Flour 594-conjugated anti-rabbit IgG antibody (A-11037, ThermoFisher Scientific, Rockford, IL, USA) at a dilution ratio of 1:1000, anti-VE-Cadherin and anti-KDR/VEGFR2 at a dilution ratio of 1:400, followed by Alexa Fluor 488-conjugated anti-rabbit IgG antibody (A-11034, ThermoFisher Scientific, Rockford, IL, USA) at a dilution ratio of 1:1000.
Negative control sections were labeled with Rabbit IgG, Isotype Control (ab172730, abcam, Cambridge, UK) at a dilution ratio of 1:400, followed by Alexa Flour 594-conjugated anti-rabbit IgG antibody and Alexa Fluor 488-conjugated anti-rabbit IgG antibody at a dilution ratio of 1:1000. In addition, all sections were labeled with anti-α Smooth Muscle Actin (A2547, SIGMA, Saint Louis, MO, USA) at a dilution ratio of 1:2000, followed by Alexa Fluor 488-conjugated anti-mouse IgG2a antibody (A-11001, ThermoFisher SCIENTIFIC, Rockford, IL, USA) and Alexa Fluor 568-conjugated anti-mouse IgG2a antibody (A-21134, ThermoFisher SCIENTIFIC, Rockford, IL, USA) at a dilution ratio of 1:2000. Nuclei were stained with DAPI (D1306, Molecular Probes, Life Technologies, Carlsbad, CA, USA) at a dilution ratio of 1:3000.
Immunofluorescence images were obtained using a custom confocal microscope based on an inverted IX70 microscope (Olympus, Tokyo, Japan) equipped with an UPLSAPO ×60/NA1.35-oil objective, a confocal laser unit (CSU10, Yokogawa, Tokyo, Japan), an electron multiplying charge-coupled device digital camera (iXon, Andor, Belfast, Northern Ireland), and a Light engine (Lumencor, Inc, Veaverton, OR, USA).
The stented vessels for SEM were fixed with 2.5% glutaraldehyde containing PBS for 2 h and subsequently treated with a series of dehydration steps using graded ethanolic aqueous solutions (50, 70, 90, 99, 99, and 99% ethanol, 10 min each step), freeze-dried in t-butyl alcohol, and then sputter-coated with platinum. SEM images were observed using SEM-EDX (Hitachi-Hitechnologies, Tokyo, Japan) and JSM-5400 (JEOL, Nagoya, Japan) at an acceleration voltage of 10 kV.
Histological analysis
Histological analysis of the neointima was performed by an experienced observer (M.M). Histological evaluation included the measurement of neointimal thickness and the percentage of neointimal area. Morphometric analysis of the inflammation, injury (graded as scores 0–3), and intimal fibrin content scores (graded as scores 1–3) was also assessed. These parameters were calculated according to the previous reports method [23, 24]. The sum of these scores for each segment was divided by the total number of struts in the examined section. Neointimal thickness was measured above the stent and over the stent struts (each mid-portion), and averaged in that cross section. Neointimal areas were measured around the stent and above the inner membrane. The percentage of neointimal area was defined as 100 × neointimal area/stent area [25]. The histological parameters were measured with digital morphometry.
Statistical analysis
All data are expressed as mean ± standard deviation (SD). The parameters (neointimal thickness, percentage of neointimal area, inflammatory score, fibrin content score, and injury score) were compared using the nonparametric method: Wilcoxon rank-sum test for the 2nd day and 14th day for each groups. A p value <0.05 was considered statistically significant (JMP software, SAS Institute Inc, Cary, NC, USA).
Results
Nobori® and S-stent™ were successfully implanted in the coronary arteries of 12 swine. All animals survived after the procedure and remained healthy until the end of the study.
Neointimal coverage
On the 2nd day, both Nobori® (n = 1) and S-stent™ (n = 1) were partly covered with a thin tissue, such as the neointima, although their surfaces seemed to be still rough (Fig. 1a, b). Both stents were covered with multiple cells layer, including spindle and round cells, and inflammatory cells, such as monocytes and blood cells aggregated surrounding stent (Fig. 1c, d, arrows). Remarkably, we morphologically characterized endothelial cells on both Nobori® and S-stent™ surfaces (Fig. 1c, d, insets). These cells were immunohistologically positive for staining with anti-von Willebrand factor antibody, anti-VE-Cadherin, and anti-KDR/VEGFR2 (Fig. 2) as well as normal coronary artery sections suggesting that endothelialization could occur at early phases. Negative control sections that were stained with non-immuno IgG did not give positive signals (data not shown).
Representative electronmicroscopic and histologic images of Nobori® and S-stent™ on the 2nd day after implantation. As observed by scanning electron microscope, Nobori® (a) and S-stent™ (b) were partly covered with thin tissues, such as neointima, although their surfaces were still rough. Inflammatory cells and blood cells in Nobori® (c) and S-stent™ (d) (arrows) were also present together with endothelial-like cells on the surfaces (c, d, inset)
Immunohistological findings of cells on the stent surfaces on the 2nd day after implantation. In both Nobori® and S-stent™, endothelial-like cells were positive for staining with anti-von Willebrand factor (b, c, red), anti-VE-Cadherin (e, f, green), and anti-KDR/VEGFR2 (h, i, green) as well as normal coronary artery (a, d, g)
On the 14th day, both Nobori® (n = 2) and S-stent™ (n = 1) were completely covered with endothelial layer which surface was smoother than on the 2nd day (Fig. 3a, b). Nobori® stent struts still contained inflammatory cells (Fig. 3c, inset), although these cells were seldom observed in S-stent™. Interestingly, smooth muscle cells, which were rarely found in Nobori®, were present in S-stent™ (Fig. 3d, inset).
Representative electronmicroscopic and histologic images of Nobori® and S-stent™ on the 14th day after implantation. As observed by scanning electron microscope, Nobori® (a) and S-stent™ (b) were completely covered with neointima, and their surfaces were smoother than those on the 2nd day (a, b, inset). Both stent struts were completely covered with an endothelial layer (c, d). Inflammatory cells were still observed in Nobori® (c, inset), although smooth muscle cells instead of inflammatory cells were observed in S-stent™ (d, inset)
Histological analysis
There were no significant differences in the neointimal thickness and percentage of neointimal area between Nobori® (n = 6) and S-stent™ (n = 6) on the 2nd day (17.3 ± 14.9 vs. 26.7 ± 13.6 µm and 3.7 ± 3.0 vs. 6.7 ± 3.7%, respectively) (Fig. 4a, b). On the 14th day, the neointimal thickness and percentage of neointimal area of Nobori® (n = 6) were 51.4 ± 4.5 µm and 10.8 ± 2.6% and those of S-stent™ (n = 6) were 76.4 ± 23.6 µm and 14.1 ± 4.2% (p < 0.05, p < 0.01) (Fig. 4a, b). This suggests that neointima proliferation in Nobori® was lower than in S-stent™, although both stent struts were completely covered with neointima on the 14th day.
Quantitative analysis of neointimal thickness and percentage of neointimal area. Both neointimal thickness and percentage of neointimal area were significantly greater in S-stent™ (n = 6) than in Nobori® (n = 6) 14th day after implantation, although no significant differences were observed in these parameters between the 2 groups (n = 6, each) on the 2nd day; *p < 0.05, **p < 0.01
No significant differences in inflammatory (1.3 ± 0.1 vs. 1.3 ± 0.3), fibrin content (2.5 ± 0.2 vs. 2.3 ± 0.2), and injury (0.10 ± 0.10 vs. 0.10 ± 0.20) scores between the 2 groups (n = 6, each stent) were observed on the 2nd day (Fig. 5a–c). Interestingly, inflammatory (1.4 ± 0.1 vs. 1.2 ± 0.2, p < 0.05) and fibrin content (1.7 ± 0.5 vs. 1.1 ± 0.1, p < 0.01) scores were significantly higher in Nobori® (n = 6) in S-stent™ (n = 6) on the 14th day, although no significant difference in injury scores (0.15 ± 0.09 vs. 0.20 ± 0.15) between the 2 groups was detected (Fig. 5a–c).
Quantitative analysis of inflammatory, fibrin content, and injury scores. There were no significant differences in inflammatory, fibrin content, and injury scores between Nobori® (n = 6) and S-stent™ (n = 6) on the 2nd day after implantation. On the 14th day, inflammatory and fibrin content scores were greater in Nobori® (n = 6) than in S-stent™ (n = 6), although the injury score was not different between the 2 groups; *p < 0.05, **p < 0.01
Discussion
The major findings of our study were the following: (1) SEM on the 2nd and 14th days after implantation showed similar tissue coverage on the Nobori® and S-stent™ struts; (2) endothelial-like cells appeared not only on S-stent™ but also on Nobori® at an early phase after implantation; and (3) histological analysis on the 14th day showed that neointima proliferation in Nobori® was lower than in S-stent™. These results suggest a possible mechanism for the low frequency of in-stent thrombosis and late in-stent restenosis in Nobori®.
Autopsy studies of patients implanted with first-generation DES showed that stent thrombosis is frequently associated with incomplete endothelialization of the stent struts and vessel walls [9]. Direct exposure of the strut surfaces to the blood stream may result in stent thrombosis, because the functional endothelial layer is known to exhibit antithrombotic and anticoagulant function via secretion of factors inhibiting platelet aggregation [26]. In our study, endothelialization of Nobori® occurred on the 2nd day, and endothelial cells were present in both Nobori® and S-stent™. SEM images showed similar endothelial coverage above Nobori® and S-stent™ struts.
In contrast to other DES, Nobori® are abluminally coated with biolimus A9, which probably enhances endothelialization at an early phase. On the 14th day after implantation, Nobori® stent struts were completely covered with neointima. Importantly, neointimal thickness and percentage of neointimal area were effectively inhibited by biolimus A9, even though the biolimus A9 was present only on the vessel wall side of the stent struts. Previous reports showed longitudinal neointimal formation and endothelialization in porcine and human coronary arteries. The response to healing after placement of the coronary stent in a human coronary artery is 5–6 times longer than in a porcine coronary artery [27,28,29]. Our experimental time course of 2 and 14 days after implantation in swine may correspond to a reasonable approximation of 10 days and 3 months in humans, respectively. Therefore, we guess that neointimal proliferation on Nobori® starts within 10 days, and endothelialization completes within 3 months after implantation in humans. Our data demonstrate that endothelialization occurred at an early phase, offering the advantage of shorter dual antiplatelet therapy period than those of other DES.
Persistent inflammatory responses in first-generation DES may lead to impaired endothelial function and in-stent thrombosis [10, 11, 13]. In contrast, lower inflammatory response in the stented segments and rapid recovery of endothelial function in the Nobori® compared with first-generation DES were observed 1 month after implantation in a porcine coronary model [30]. Furthermore, minimal inflammation response was observed with Nobori® at 1–6 month follow-ups [31, 32], probably because the drug was completely released from the polymer coating 6–9 months after implantation (data from TERUMO). In our study, there were no significant differences in inflammatory and fibrin content scores on the 2nd day, although these parameters on the 14th day were slightly higher in Nobori® than in S-stent™. With regard to inflammatory cells and fibrin deposition, biolimus A9 showed high inflammatory and fibrin content scores and inflammatory reaction in Nobori®, as a biological reaction against PLA degradation products. On the other hand, no significant differences were detected in inflammatory and fibrin content scores on the 2nd day, suggesting high biocompatibility of Nobori® in the early phase.
Implication and limitations
The present study provides important implications for development of coronary stents. In terms of early endothelialization of the stent surface, the enhanced method to capture the endothelial progenitor cells can be an alternative way for effective endothelialization [33]. Actually, we previously reported that VEGF-coated metal stent could capture endothelial progenitor cells to enhance early endothelialization in an experimental model [22].
Our study has some limitations. First, since we only studied healthy swine not suffering from arteriosclerosis, our data revealed vessel response to stents in healthy conditions. However, even under these conditions, early endothelialization in Nobori® may explain the mechanism of low frequency of in-stent thrombosis. Second, we identified endothelial cells by immunohistological staining. Under these conditions, one might speculate the possible contamination of inflammatory cells which appeared in response to stent implantation. However, it is highly possible that the newly appeared cells were endothelial cells because of positive for 3 different antibodies which were confirmed in control and negative control. Third, the time points were only the 2nd and 14th day after stent implantation. At the end of the study, we observed higher inflammatory response in Nobori® than in S-stent™. Although this might be derived from the reaction against PLA degradation products, it is still unclear how long these reactions may last in Nobori®. Although long-term studies already showed minimal inflammatory reaction in Nobori® as well as in BMS 3–15 months after implantation [34], we should performed to confirm these findings.
Conclusions
Our study demonstrated that endothelialization could occur early after Nobori® implantation with similar inflammatory reaction to BMS. The neointimal proliferation was effectively inhibited in Nobori® on the 14th day after implantation, suggesting low frequency of in-stent thrombosis and restenosis.
References
Versaci F, Gaspardone A, Tomai F, Crea F, Chiariello L, Gioffrè PA (1997) A comparison of coronary-artery stenting with angioplasty for isolated stenosis of the proximal left anterior descending coronary artery. N Engl J Med 336:817–822
Grines CL, Cox DA, Stone GW, Garcia E, Mattos LA, Giambartolomei A, Brodie BR, Madonna O, Eijgelshoven M, Lansky AJ, O’Neill WW, Morice MC (1999) Coronary angioplasty with or without stent implantation for acute myocardial infarction. Stent primary angioplasty in myocardial infarction study group. N Engl J Med 341:1949–1956
Uchiyama K, Ino H, Hayashi K, Fujioka K, Takabatake S, Yokawa J, Namura M, Mizuno S, Tatami R, Kanaya H, Nitta Y, Michishita I, Hirase H, Ueda K, Aoyama T, Okeie K, Haraki T, Mori K, Araki T, Minamoto M, Oiwake H, Konno T, Sakata K, Kawashiri M, Yamagishi M (2011) Impact of severe coronary disease associated or not associated with diabetes mellitus on outcome of interventional treatment using stents: results from HERZ (Heart Research Group of Kanazawa) analyses. J Int Med Res 39:549–557
Kastrati A, Dibra A, Mehilli J, Mayer S, Pinieck S, Pache J, Dirschinger J, Schömig A (2006) Predictive factors restenosis after coronary implantation of sirolimus- or paclitaxel-eluting stents. Circulation 113:2293–2300
Serruys PW, Kutryk MJ, Ong AT (2006) Coronary-artery stents. N Engl J Med 354:483–495
Yoshida T, Sakata K, Nitta Y, Taguchi T, Kaku B, Katsuda S, Shimojima M, Gamou T, Nakahashi T, Konno T, Kawashiri MA, Yamagishi M, Hayashi K (2015) Short- and long-term benefits of drug-eluting stents compared to bare metal stents even in treatment for large coronary arteries. Heart Vessels 31:635–642
Kawashiri MA, Sakata K, Uchiyama K, Konno T, Namura M, Mizuno S, Tatami R, Kanaya H, Nitta Y, Michishita I, Hirase H, Ueda K, Aoyama T, Okeie K, Haraki T, Mori K, Araki T, Minamoto M, Oiwake H, Ino H, Hayashi K, Yamagishi M (2014) Impact of lesion morphology and associated procedures for left main coronary stenting on angiographic outcome after intervention: sub-analysis of Heart Research Group of Kanazawa, HERZ, Study. Cardiovasc Interv Ther 29:117–122
Kobayashi N, Ito Y, Hirano K, Yamawaki M, Araki M, Sakai T, Takimura H, Sakamoto Y, Mori S, Tsutsumi M, Takama T, Takafuji H, Maruyama T, Honda Y, Tokuda T, Makino K, Shirai S, Muramatsu T (2016) Comparison of first- and second-generation drug-eluting stent efficacies for treating left main and/or three-vessel disease: a propensity matched study. Heart Vessels 31:1930–1942
Joner M, Finn AV, Farb A, Mont EK, Kolodgie FD, Ladich E, Kutys R, Skorija K, Gold HK, Virmani R (2006) Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol 48:193–202
Cook S, Ladich E, Nakazawa G, Eshtehardi P, Neidhart M, Vogel R, Togni M, Wenaweser P, Billinger M, Seiler C, Gay S, Meier B, Pichler WJ, Jüni P, Virmani R, Windecker S (2009) Correlation of intravascular ultrasound findings with histopathological analysis of thrombus aspirates in patients with very late drug-eluting stent thrombosis. Circulation 120:391–399
Sakata K, Namura M, Takagi T, Tama N, Inoki I, Terai H, Horita Y, Ikeda M, Yamagishi M (2015) Repeated occurrence of slow flow phenomenon during and late after sirolimus-eluting stent implantation. Heart Vessels 30:406–409
Kurosawa T, Kotani J, Matsuyama TA, Ishibashi-Ueda H (2015) A case of active peri-stent inflammation after sirolimus-eluting stent implantation. Heart Vessels 30:270–273
Finn AV, Joner M, Nakazawa G, Kolodgie F, Newell J, John MC, Gold HK, Virmani R (2007) Pathological correlates of late drug-eluting stent thrombosis: strut coverage as a marker of endothelialization. Circulation 115:2435–2441
Pfisterer M, Brunner-La Rocca HP, Buser PT, Rickenbacher P, Hunziker P, Mueller C, Jeger R, Bader F, Osswald S, Kaiser C, Investigators BASKET-LATE (2006) Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents. J Am Coll Cardiol 48:2584–2591
Virmani R, Guagliumi G, Farb A, Musumeci G, Grieco N, Motta T, Mihalcsik L, Tespili M, Valsecchi O, Kolodgie FD (2004) Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation 109:701–705
Nebeker JR, Virmani R, Bennett CL, Hoffman JM, Samore MH, Alvarez J, Davidson CJ, McKoy JM, Raisch DW, Whisenant BK, Yarnold PR, Belknap SM, West DP, Gage JE, Morse RE, Gligoric G, Davidson L, Feldman MD (2006) Hypersensitivity cases associated with drug-eluting coronary stents: a review of available cases from the Research on Adverse Drug Events and reports (RADAR) project. J Am Coll Cardiol 47:175–181
Chevalier B, Silber S, Park SJ, Garcia E, Schuler G, Suryapranata H, Koolen J, Hauptmann KE, Wijns W, Morice MC, Carrie D, van Es GA, Nagai H, Detiege D, Paunovic D, Serruys PW, NOBORI 1 Clinical Investigators (2009) Randomized comparison of the Nobori Biolimus A9-eluting coronary stent with the Taxus Liberte paclitaxel-eluting coronary stent in patients with stenosis in native coronary arteries: the NOBORI 1 trial—phase 2. Circ Cardiovasc Interv 2:188–195
Nishimiya K, Matsumoto Y, Shindo T, Hanawa K, Hasebe Y, Tsuburaya R, Shiroto T, Takahashi J, Ito K, Ishibashi-Ueda H, Yasuda S, Shimokawa H (2015) Association of adventitial vasa vasorum and inflammation with coronary hyperconstriction after drug-eluting stent implantation in pigs in vivo. Circ J 79:1787–1798
Serruys PW, Farooq V, Kalesan B, de Vries T, Buszman P, Linke A, Ischinger T, Klauss V, Eberli F, Wijns W, Morice MC, Di Mario C, Corti R, Antoni D, Sohn HY, Eerdmans P, Rademaker-Havinga T, van Es GA, Meier B, Jüni P, Windecker S (2013) Improved safety and reduction in stent thrombosis associated with biodegradable polymer-based biolimus-eluting stents versus durable polymer-based sirolimus-eluting stents in patients with coronary artery disease: final 5-year report of the LEADERS (Limus Eluted From A Durable Versus ERodable Stent Coating) randomized, noninferiority trial. JACC Cardiovasc Interv 6:777–789
Natsuaki M, Kozuma K, Morimoto T, Kadota K, Muramatsu T, Nakagawa Y, Akasaka T, Igarashi K, Tanabe K, Morino Y, Ishikawa T, Nishikawa H, Awata M, Abe M, Okada H, Takatsu Y, Ogata N, Kimura K, Urasawa K, Tarutani Y, Shiode N, Kimura T (2013) Biodegradable polymer biolimus-eluting stent versus durable polymer everolimus-eluting stent: a randomized, controlled, noninferiority trial. J Am Coll Cardiol 62:181–190
Christiansen EH, Jensen LO, Thayssen P, Tilsted HH, Krusell LR, Hansen KN, Kaltoft A, Maeng M, Kristensen SD, Bøtker HE, Terkelsen CJ, Villadsen AB, Ravkilde J, Aarøe J, Madsen M, Thuesen L, Lassen JF (2013) Biolimus-eluting biodegradable polymer-coated stent versus durable polymer-coated sirolimus-eluting stent in unselected patients receiving percutaneous coronary intervention (SORT OUT V): a randomised non-inferiority trial. Lancet 381:661–669
Takabatake S, Hayashi K, Nakanishi C, Hao H, Sakata K, Kawashiri MA, Matsuda T, Yamagishi M (2014) Vascular endothelial growth factor-bound stents: application of in situ capture technology of circulating endothelial progenitor cells in porcine coronary model. J Interv Cardiol 27:63–72
Schwartz RS, Huber KC, Murphy JG, Edwards WD, Camrud AR, Vlietstra RE, Holmes DR (1992) Restenosis and the proportional neointimal response to coronary artery injury: results in a porcine model. J Am Coll Cardiol 19:267–274
Suzuki T, Kopia G, Hayashi S, Bailey LR, Llanos G, Wilensky R, Klugherz BD, Papandreou G, Narayan P, Leon MB, Yeung AC, Tio F, Tsao PS, Falotico R, Carter AJ (2001) Stent-based delivery of sirolimus reduces neointimal formation in a porcine coronary model. Circulation 104:1188–1193
Sakata K, Waseda K, Kume T, Otake H, Nakatani D, Yock PG, Fitzgerald PJ, Honda Y (2012) Impact of diabetes mellitus on vessel response in the drug-eluting stent era: pooled volumetric intravascular ultrasound analyses. Circ Cardiovasc Interv 5:763–771
Pearson JD (1994) Endothelial cell function and thrombosis. Baillieres Clin Haematol 7:441–452
Carter AJ, Laird JR, Farb A, Kufs W, Wortham DC, Virmani R (1994) Morphologic characteristics of lesion formation and time course of smooth muscle cell proliferation in a porcine proliferative restenosis model. J Am Coll Cardiol 24:1398–1405
Taylor AJ, Gorman PD, Kenwood B, Hudak C, Tashko G, Virmani R (2001) A comparison of four stent designs on arterial injury, cellular proliferation, neointima formation, and arterial dimensions in an experimental porcine model. Catheter Cardiovasc Interv 53:420–425
Farb A, Sangiorgi G, Carter AJ, Walley VM, Edwards WD, Schwartz RS, Virmani R (1999) Pathology of acute and chronic coronary stenting in humans. Circulation 99:44–52
Pendyala LK, Matsumoto D, Shinke T, Iwasaki T, Sugimoto R, Hou D, Chen JP, Singh J, King SB 3rd, Chronos N, Li J (2012) Nobori stent shows less vascular inflammation and early recovery of endothelial function compared with Cypher stent. JACC Cardiovasc Interv 5:436–444
Nakazawa G, Shinke T, Ijichi T, Matsumoto D, Otake H, Torii S, Hiranuma N, Ohsue T, Otsuka F, Shite J, Hirata K, Ikari Y (2014) Comparison of vascular response between durable and biodegradable polymer-based drug-eluting stents in a porcine coronary artery model. EuroIntervention 10:717–723
Hiranuma N, Shinke T, Nakazawa G, Otake H, Matsumoto D, Ijichi T, Kawamori H, Nagoshi R, Osue T, Shite J, Hirata K (2014) Optical coherence tomography and histopathology assessment after implantation of first- and second-generation drug-eluting stents in a porcine coronary model. Circ J 78(11):2665–2673
Tagawa S, Matsuda T, Aomizu T, Kuwana M, Ohtake H, Watanabe G, Yamagishi M (2014) Surface-bound vascular endothelial growth factor promotes prolonged activation of endothelial cells: a new technology for capturing endothelial progenitor cells by intravascular stents. J Tissue Sci Eng 5:1000140. doi:10.4172/2157-7552.1000140
Hagiwara H, Hiraishi Y, Terao H, Hirai T, Sakaoka A, Sasaki M, Murota S, Inoue K, Kimura J (2012) Vascular responses to a biodegradable polymer (polylactic acid) based biolimus A9-eluting stent in porcine models. EuroIntervention 8:743–751
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was in part supported by TERUMO.
Conflict of interest
Masakazu Yamagishi receives significant research funding from TERUMO. The other authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mori, M., Sakata, K., Nakanishi, C. et al. Early endothelialization associated with a biolimus A9 bioresorbable polymer stent in a porcine coronary model. Heart Vessels 32, 1244–1252 (2017). https://doi.org/10.1007/s00380-017-0992-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-0992-5