Abstract
During circumferential pulmonary vein (PV) isolation for ongoing atrial fibrillation (AF), distinguishing passive conduction to the pulmonary vein (PV) from rapid PV arrhythmia in the isolated PV is difficult. Hence, the purpose of this study is to investigate both the feasibility of distinguishing the PV tachycardia after circumferential PV isolation and the electrophysiological characteristics of these tachycardia. Among 178 consecutive patients who underwent circumferential PV isolation during ongoing AF, fibrillatory PV converted to a regular cycle length PV tachycardia independent of the atrial rhythm (=independent PV tachycardia) in 13 PVs among 12 (7%) patients. We classified independent PV tachycardia according to 3 different atrial rhythms: sinus rhythm (type 1, n = 2), atrial tachycardia (type 2, n = 4), and AF (type 3, n = 6). independent PV tachycardia was observed in 3 right PV and 10 left PV (P = 0.0864). There were 10 mappable independent PV tachycardia, in which 8 were focal and 2 were macroreentrant tachycardia. i-PVT can be diagnosed in a small number of patients who underwent circumferential PV isolation during AF. The main mechanism or independent PV tachycardia was focal tachycardia mainly in the left PV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary vein (PV) plays an important role in the initiation and perpetuation of atrial fibrillation (AF). Initially, the main target to prevent AF was to ablate the ectopic foci in the PVs [1]. Subsequently, ipsilateral PV isolation (PVI) of both superior and inferior PVs by circumferential PVI has become the corner stone for AF treatment [2, 3].
Dissociated PV activity after PVI is seen in 9 to 91% in patients with AF [4–10]. Slow dissociated PV activity is important to recognize as these arrhythmias can be predictors for AF recurrence and targeting these arrhythmias may improve clinical results [4, 5, 11]. To the contrary, little is known about rapid PV arrhythmia with a regular cycle length (CL) within the PV after circumferential PVI which we named “independent PV tachycardia”. The current manuscript shows the feasibility of diagnosing independent PV tachycardia and its electrophysiological characteristics during circumferential PVI for treating ongoing AF.
Materials and methods
Study population and electrophysiological study
We analyzed 178 consecutive patients who entered the catheter room with spontaneous AF and performed circumferential PVI at our department form October 2007 to July 2010. After completing circumferential PVI, there were 12 patients with independent PV tachycardia sustaining more than 10 min within the isolated PV. Clinical characteristics of each patient are shown in Table 1.
Patients underwent ablation therapy in the fasting state under deep sedation with intravenous propofol and pentazocine hydrochloride. Antiarrhythmic medications were discontinued at least 5 half-lives before the procedure. Warfarin was administered (international normalized ratio 2–3 times) for at least 1 month and transesophageal echocardiography was performed prior to the procedure to exclude LA thrombus. Standard catheters were positioned as follows: a 5F quadripolar electrode catheter (Livewire RV-His. St Jude Medical, Inc., Minnetonka, MN, USA) at His-bundle, a 6F decapolar catheter in the coronary sinus (EP star. Japan Life Line, Inc., Tokyo, Japan). Two or Three 8 or 8.5 F long sheaths (SL0, St Jude Medical, Inc. or Preface, Biosense Webster Inc., Diamond Bar, CA, USA) were positioned in the LA via transseptal approach. One or two duo-decapolar lasso catheters (Biosense Webster Inc.) were placed within the common or ipsilateral superior and inferior PV, respectively, during RF delivery. After transseptal catheterization, intravenous unfractionated heparin was administered to maintain the activated clotting time between 300 and 350 s and monitored every 30 min.
The study was approved by the institutional review board and all patients were given written informed consent.
Three-dimensional electroanatomical mapping and RF ablation
The method of 3-D electroanatomical mapping in the LA has been described previously in detail [2]. Briefly, mapping was performed with a 3.5 mm-tip catheter (ThermoCool Navi-Star, Biosense Webster Inc.) during AF using the CARTO mapping system (Biosense Webster Inc.). After construction of the LA shell, each PV ostium was identified by selective venography and tagged on the electroanatomic map 5 mm outside from the angiographically defined PV ostia. In all patients, circumferential PVI was performed from the right-sided PV (RPV) followed by the left-sided PV (LPV). Electrical PVI was the initial endpoint for all procedures unless AF converted to atrial tachycardia. If so, we mapped the tachycardia and made an anatomical linear block to the critical site of the circuit. We did not perform complexed fractionated electrogram ablation. We performed electrical cardioversion if AF did not terminate after these procedures. Target temperature was 43 °C at a maximal power of 25–30 W with an infusion rate of 17 mL/min.
Definition of independent PV tachycardia
We defined independent PV tachycardia as a tachycardia with a regular CL < 400 ms continuing more than 10 min and classified into 3 types according to the atrial rhythm. First, if sinus rhythm (SR) restored during circumferential PVI, PV tachycardia dissociating from atrial SR was diagnosed as type 1 independent PV tachycardia (Fig. 1a). Second, if AF converted to a regular CL atrial tachycardia (AT), PV tachycardia who’s CL is discordant to AT CL was diagnosed as type 2 independent PV tachycardia (Fig. 1b). Third, if AF continues after circumferential PVI, PV tachycardia demonstrating a regular CL was diagnosed as type 3 independent PV tachycardia (Fig. 1c).
Electrogram and schematic image of each independent PV tachycardia. The moment of PV isolation is shown by the dotted line in each figure. a Type 1 independent PV tachycardia before and after circumferential PVI (Patient #1). The scheme represents the independent PV tachycardia dissociating from atrial SR after PVI. In the electrogram, SR restored after isolation and PV activity changed to independent PV tachycardia with a 2:1 conduction from proximal LSPV to mid LSPV and 4:1 conduction from proximal LSPV to LIPV. b Type 2 independent PV tachycardia before and after circumferential PVI (Patient #5). The scheme represents the AF converting to an AT in the atrium and independent PV tachycardia who’s CL is discordant to the AT cycle length. In the electrogram, AF converted to AT after circumferential PVI with a discordant cycle length compared to independent PV tachycardia potentials in the LSPV (arrow head) (CSCL = 300 ms, PVCL = 170 ms). LIPV is a passive 2:1 activation from LSPV. Distal part of LSVP catheter are with LA potentials showing AT rhythm (arrow). c Type 3 independent PV tachycardia before and after circumferential PVI (Patient #8). The scheme represents the atrium continuing AF, while the PV starts to be an independent PV tachycardia. In the electrogram, AF continues after circumferential PVI, but the rhythm changes independent PV tachycardia (arrow head) in LSPV. Proximal part of LSPV catheter is with LA potentials showing AF (arrow). Abl ablation catheter, AF atrial fibrillation, AT atrial tachycardia, PVI pulmonary vein isolation, CS coronary sinus, CSCL cycle length of coronary sinus, LA left atrium, LIPV left inferior pulmonary vein, LSPV left superior pulmonary vein, PV pulmonary vein, PVCL cycle length of independent pulmonary vein tachycardia, PVI pulmonary vein isolation, SR sinus rhythm
Entrainment pacing and activation mapping were performed during tachycardia within the PV to analyze electrophysiological characteristics. The CL of independent PV tachycardia and atrium were measured by lasso catheter (PVCL) and distal CS electrode (CSCL) respectively during tachycardia. If AF continued after circumferential PVI, CSCL was defined as the mean CL analyzed during 30 s.
Statistical analysis
Quantitative values are presented as mean ± standard deviation. Means of continuous variables that showed normal distribution were compared with Student t test for independent samples. Fisher’s exact test or χ 2 test was used for categorical variables. Continuous variables that did not show a normal distribution were compared with nonparametric statistics (Mann–Whitney test). P < 0.05 was considered statistically significant. All analyses were performed with SPSS 17.0 statistical package (SPSS, Inc., Chicago, IL, USA).
Results
Patient characteristics
There were 12 patients (n = 9; men, age, 65 ± 6 years) who had independent PV tachycardia. Six were paroxysmal and six were persistent AF. The mean duration between AF diagnosis and radiofrequency (RF) ablation was 4.7 ± 2.6 years. There was no structural heart disease in all patients and the mean left atrial (LA) diameter was 44 ± 5 mm. There were 5 patients with left common PV defined as superior and inferior left PV joining >5 mm before entering LA.
Diagnosis of independent PV tachycardia
One hundred and seventy-eight patients performed circumferential PVI during AF and 13 PVs among 12 patients (7%) showed independent PV tachycardia (Table 1). Completing circumferential PVI around LPV terminated AF and restored SR in 2 patients (Type 1).
AF converted to typical atrial flutter in 3 and mitral flutter in 1 patient (Type 2). PVCL was shorter than CSCL during AT (PVCL = 190 ± 41 vs. CSCL = 268 ± 33 ms, P = 0.027) in all patients. Linear ablation at the cavo-tricuspid or mitral isthmus terminated the atrial tachycardia and restored SR in all patients though independent PV tachycardia continued.
In the remaining 6 patients, AF did not terminate after complete circumferential PVI, but the fibrillatory PV activity converted to regular PV tachycardia (Type 3). PVCL during independent PV tachycardia was longer than CSCL during AF (PVCL = 166 ± 22 vs. CSCL = 119 ± 12 ms, P = 0.002) in all patients. One patient had an independent PV tachycardia in both LPV and RPV (Patient #9).
Although there was a tendency for more frequent independent PV tachycardia in the LPV, it was not significant (LPV = 10/178 vs. RPV = 3/178, P = 0.0864). There was only one patient who had independent PV tachycardia limited in the inferior PV.
Electrophysiological characteristics of independent PV tachycardia
Among 13 independent PV tachycardia, 3 terminated spontaneously or by catheter manipulation before mapping and the mechanism could not be diagnosed. Two were macrorentrant (Patient #11 and #12) and eight were focal. Patient #12 had a large left common PV and had a fibrillatory PV activity before circumferential PVI. It was converted to independent PV tachycardia by complete circumferential PVI though AF continued in the atrium (Fig. 2a). By pacing from inside the PV, concealed entrainment with a perfect match of post-pacing interval was observed (Fig. 2b). After electrical cardioversion, AF terminated in the atrium, but independent PV tachycardia continued within the PV as an evidence of exit block (Fig. 2c). The electroanatomical map during independent PV tachycardia demonstrated a reentrant pattern within the left common PV covering the whole CL (Fig. 2d), suggesting reentry as the mechanism of tachycardia along with the entrainment study. Applying few RF application terminated independent PV tachycardia (Fig. 2c).
Case of a type 3 i-PVT with common left PV. a AF continues after circumferential PVI (shown as dotted line), but the rhythm changes to independent PV tachycardia in the left common PV. b Entrainment pacing from proximal PV entrains the independent PV tachycardia with a perfect post-pacing interval. Even during this pacing study, AF and independent PV tachycardia continues in LA and LPV respectively. c Electrogram during RF application after electrical cardioversion. LA is in SR, though independent PV tachycardia continues. During RF application, independent PV tachycardia terminates (shown as dotted line). d Reconstructed 3D-CT image of the left atrium on the left side and the activation map of the atrial tachycardia covering the whole cycle length of independent PV tachycardia. CARTO tags definition: white tagged ostium of pulmonary veins, dark red ablation point, sky-blue good post-pacing interval point. LPV left pulmonary vein, other abbreviations are as in Fig. 1. (Color figure online)
Finally, independent PV tachycardia terminated spontaneously in 2, by catheter manipulation in 1, by RF applications in 7, and after entrainment pacing in 1. The other 2 cases were terminated with electrical cardioversion.
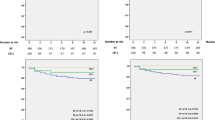
Procedure outcome
Electrical PVI was achieved in all patients. In the 4 patents with cavo-tricuspid dependent AFL or mitral AFL, linear lesions were created at the CTI or mitral isthmus and the bidirectional block was confirmed in all patients. Mean procedure time was 299 ± 71 min, RF duration was 47 ± 7 min, and fluoroscopy exposure time was 45 ± 10 min. No complication occurred during and after the ablation procedure. After 1 year of follow-up period, the recurrence-free rate of AF/AT was 66.7 and 68.9% for patients with and without independent PV tachycardia, respectively.
Discussion
Main findings
The main findings in this study about of independent PV tachycardia were: (1) 7% of the patients had independent PV tachycardia and could be classified into 3 types according to the atrial rhythm; (2) PVCL was shorter than CSCL in type 2 and longer in type 3; and (3) the frequent mechanism was focal tachycardia majorly in the left PVs.
Incidence of independent PV tachycardia
The incidence of PV activity ranges 9 to 91% of patients after PV isolation and this wide range is from the various definition of PV activity [4–10]. Hence, the importance of terminology, we defined independent PV tachycardia as PV tachycardia with regular CL < 400 ms after complete circumferential PVI continuing longer than 10 min. This CL was determined following after Weerasooriya et al. defining rapid tachycardia irrespective of the rhythm [10] and 10 min was the least time to diagnose each independent PV tachycardia pattern.
According to this definition, there were 7% who showed independent PV tachycardia which is compatible with 9% to Weerasooriya et al. including fibrillating PV cases [10]. There was a tendency to have more frequent independent PV tachycardia in the LPV and only one case was limited in the inferior PV. This is a concordant result with Heissaguere et al. reporting the origins of ectopy for AF [1].
Feasibility of diagnosis
There were 2 patients classified as type 1 independent PV tachycardia which were easily diagnosed as the LA was already in SR during independent PV tachycardia.
There were 4 patients classified as type 2 independent PV tachycardia. In these cases, PVCL was shorter than CSCL in all cases and also the average for all patients was significantly shorter. This may be explained as AT after circumferential PVI are mainly macroreentrant tachycardia with a relatively long CL [12]. In fact, three were 3 typical atrial flutter and 1 mitral flutter in the present study. As PVCL was always shorter than CSCL, we should pay attention for shorter PVCL when AF converts to AT.
There were 6 patients classified as type 3 independent PV tachycardia and was difficult to diagnose, as we have to distinguish independent PV tachycardia from passive PV activity before complete circumferential PVI. A careful observation to notice the sudden change in the PV electrogram during the procedure is most important to identify independent PV tachycardia. As PVCL was longer than CSCL in all cases, and also the average was significantly longer, we should check for the elongation of PV cycle length when we are reaching the complete circumferential PVI.
Electrophysiology of independent PV tachycardia
The antrum is known to have both part of the substrate and trigger of AF [13–18]. We ablated 5 mm out of the PV ostium which results in keeping a large mass of antral tissue within the isolated area. As independent PV tachycardia is rarely observed during segmental pulmonary isolation, we think that the PV antrum plays an important role in maintaining independent PV tachycardia. We had 1 patient (Patient #12) whose independent PV tachycardia could be entrained at the antrum and within the PV which indicates a small circuit between the antrum and the PV. This is supported by the report from Kumagai et al. showing that the conduction circuit between the PV and the atrium plays an important role for the tachycardia [14].
Substrates out of the pulmonary vein
Since solo therapy with PVI is not sufficient in treating persistent AF patients, substrate ablation outside of PVs is granted important in these patients. From the early experiments, regions with rapid and continuous activation were known to be responsible for maintaining AF [19–21]. Nademanee et al. described that targeting these electrograms results in a 76% success rate after a single procedure [22]. By a noninvasive mapping system, PV antrum, atrial septum, and left atrial appendage were the most important driver region which correlated to complexed fractionated electrograms, with some conflicting data depending on the mapping system [23, 24]. To our interest, at least in the patients with independent PV tachycardia, AF substrate was most likely limited within the isolated wide PV and solo PVI may be favorable to maintain SR after ablation. However, the limited number of patients with the independent PV tachycardia suggested that the AF substrate out of PV was more important in the persistent AF.
Clinical implications
Some studies showed that ablating PV triggers have additional effect for clinical results and aggressive treatment to independent PV tachycardia may also have a similar additional effect as making a permanent PVI is difficult [4, 5, 25]. This must be proved in the future study.
Misdiagnosing independent PV tachycardia as a residual gap leads to potent risk for over treatment especially in type 2 and type 3 independent PV tachycardia patients. The regular activity after circumferential PVI especially in the left PVs suggests the presence of independent PV tachycardia and cardioversion of the LA can confirm the completion of circumferential PVI.
In type 3 independent PV tachycardia patients, AF was not able to terminate even by electrical cardioversion before completing circumferential PVI. However, after electrical PVI, sinus rhythm was achieved with electrical cardioversion. Therefore, independent PV tachycardia can be both the trigger and the driver of AF in patients with persistent AF. In patients with independent PV tachycardia, solo circumferential PVI may be enough to maintain SR without additional application such as linear lesions and complexed fractionated electrogram ablation. This may lead to potent merit as aggressive applications often end up in further problems with post-ablation AT [12].
Limitations
We performed cardioversion in some patients during ablation before complete circumferential PVI. As cardioversion has a chance to terminate both AF and independent PV tachycardia, there was a potential possibility to underestimate independent PV tachycardia. Further investigations including more patients are awaited to prove the effect of the clinical outcome.
Conclusions
Independent PV tachycardia was able to recognize during circumferential PVI with ongoing AF. As the difference of PVCL and CSCL had specific difference in each type, routine check of the CL discrepancy helps to realize these arrhythmias. The main mechanism or independent PV tachycardia was focal tachycardia majorly in the left PVs.
References
Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Metayer P, Clementy J (1998) Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med 339(10):659–666
Ouyang F, Bansch D, Ernst S, Schaumann A, Hachiya H, Chen M, Chun J, Falk P, Khanedani A, Antz M, Kuck KH (2004) Complete isolation of left atrium surrounding the pulmonary veins: new insights from the double-Lasso technique in paroxysmal atrial fibrillation. Circulation 110(15):2090–2096
Pappone C, Rosanio S, Oreto G, Tocchi M, Gugliotta F, Vicedomini G, Salvati A, Dicandia C, Mazzone P, Santinelli V, Gulletta S, Chierchia S (2000) Circumferential radiofrequency ablation of pulmonary vein ostia: A new anatomic approach for curing atrial fibrillation. Circulation 102(21):2619–2628
Doi A, Satomi K, Makimoto H, Yokoyama T, Yamada Y, Okamura H, Noda T, Aiba T, Aihara N, Yasuda S, Ogawa H, Kamakura S, Shimizu W (2013) Efficacy of additional radiofrequency applications for spontaneous dissociated pulmonary vein activity after pulmonary vein isolation in patients with paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 24(8):894–901
De Greef Y, Tavernier R, Vandekerckhove Y, Duytschaever M (2010) Triggering pulmonary veins: a paradoxical predictor for atrial fibrillation recurrence after PV isolation. J Cardiovasc Electrophysiol 21(4):381–388
Kabra R, Heist EK, Barrett CD, Donaldson D, Blendea D, Beinart R, Koruth J, Singh S, Ruskin J, Mansour M (2010) Incidence and electrophysiologic properties of dissociated pulmonary vein activity following pulmonary vein isolation during catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 21(12):1338–1343
Buiatti A, Ammar S, Reents T, Semmler V, Kathan S, Hofmann M, Bourier F, Telishevska M, Koch-Buttner K, Kaess B, Lennerz C, Kolb C, Hessling G, Deisenhofer I (2015) Dissociated pulmonary vein activity after pulmonary vein isolation for paroxysmal atrial fibrillation: a predictor for recurrence? J Cardiovasc Electrophysiol 26(1):7–13
Willems S, Weiss C, Risius T, Rostock T, Hoffmann M, Ventura R, Meinertz T (2003) Dissociated activity and pulmonary vein fibrillation following functional disconnection: impact for the arrhythmogenesis of focal atrial fibrillation. Pacing Clin Electrophysiol 26(6):1363–1370
Chen H, Yang B, Ju W, Zhang F, Hou X, Chen C, Zhai L, Wang J, Cao K, Chen M, Tse HF (2011) Long-term clinical implication of the occurrence of dissociated pulmonary vein activities after circumferential left atrial ablation in patients with paroxysmal atrial fibrillation. Circ J 75(1):73–79
Weerasooriya R, Jais P, Scavee C, Macle L, Shah DC, Arentz T, Salerno JA, Raybaud F, Choi KJ, Hocini M, Clementy J, Haissaguerre M (2003) Dissociated pulmonary vein arrhythmia: incidence and characteristics. J Cardiovasc Electrophysiol 14(11):1173–1179
Satomi K (2010) Electrophysiological characteristics of atrial tachycardia after pulmonary vein isolation of atrial fibrillation. Circ J 74(6):1051–1058
Castrejon-Castrejon S, Ortega M, Perez-Silva A, Doiny D, Estrada A, Filgueiras D, Lopez-Sendon JL, Merino JL (2011) Organized atrial tachycardias after atrial fibrillation ablation. Cardiol Res Pract 2011:957538
Nakagawa H, Jackman WM, Scherlag BJ, Lazzara R (2003) Pulmonary vein isolation during atrial fibrillation: insight into the mechanism of pulmonary vein firing. J Cardiovasc Electrophysiol 14(3):261–262
Kumagai K, Ogawa M, Noguchi H, Yasuda T, Nakashima H, Saku K (2004) Electrophysiologic properties of pulmonary veins assessed using a multielectrode basket catheter. J Am Coll Cardiol 43(12):2281–2289
Lazar S, Dixit S, Callans DJ, Lin D, Marchlinski FE, Gerstenfeld EP (2006) Effect of pulmonary vein isolation on the left-to-right atrial dominant frequency gradient in human atrial fibrillation. Heart Rhythm 3(8):889–895
Roux JF, Gojraty S, Bala R, Liu CF, Dixit S, Hutchinson MD, Garcia F, Lin D, Callans DJ, Riley M, Marchlinski F, Gerstenfeld EP (2009) Effect of pulmonary vein isolation on the distribution of complex fractionated electrograms in humans. Heart Rhythm 6(2):156–160
Scherlag BJ, Nakagawa H, Jackman WM, Yamanashi WS, Patterson E, Po S, Lazzara R (2005) Electrical stimulation to identify neural elements on the heart: their role in atrial fibrillation. J Interv Card Electrophysiol 13(Suppl 1):37–42
Pappone C, Santinelli V, Manguso F, Vicedomini G, Gugliotta F, Augello G, Mazzone P, Tortoriello V, Landoni G, Zangrillo A, Lang C, Tomita T, Mesas C, Mastella E, Alfieri O (2004) Pulmonary vein denervation enhances long-term benefit after circumferential ablation for paroxysmal atrial fibrillation. Circulation 109(3):327–334
Morillo CA, Klein GJ, Jones DL, Guiraudon CM (1995) Chronic rapid atrial pacing. Structural, functional, and electrophysiological characteristics of a new model of sustained atrial fibrillation. Circulation 91(5):1588–1595
Konings KT, Kirchhof CJ, Smeets JR, Wellens HJ, Penn OC, Allessie MA (1994) High-density mapping of electrically induced atrial fibrillation in humans. Circulation 89(4):1665–1680
Hoshiyama T, Yamabe H, Koyama J, Kanazawa H, Ogawa H (2016) Left atrial electrophysiologic feature specific for the genesis of complex fractionated atrial electrogram during atrial fibrillation. Heart Vessels 31(5):773–782
Nademanee K, McKenzie J, Kosar E, Schwab M, Sunsaneewitayakul B, Vasavakul T, Khunnawat C, Ngarmukos T (2004) A new approach for catheter ablation of atrial fibrillation: mapping of the electrophysiologic substrate. J Am Coll Cardiol 43(11):2044–2053
Haissaguerre M, Hocini M, Denis A, Shah AJ, Komatsu Y, Yamashita S, Daly M, Amraoui S, Zellerhoff S, Picat MQ, Quotb A, Jesel L, Lim H, Ploux S, Bordachar P, Attuel G, Meillet V, Ritter P, Derval N, Sacher F, Bernus O, Cochet H, Jais P, Dubois R (2014) Driver domains in persistent atrial fibrillation. Circulation 130(7):530–538
Narayan SM, Krummen DE, Shivkumar K, Clopton P, Rappel WJ, Miller JM (2012) Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J Am Coll Cardiol 60(7):628–636
Ouyang F, Antz M, Ernst S, Hachiya H, Mavrakis H, Deger FT, Schaumann A, Chun J, Falk P, Hennig D, Liu X, Bansch D, Kuck KH (2005) Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation 111(2):127–135
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yamagata, K., Doi, A., Kawata, H. et al. Persistent tachycardia within isolated pulmonary veins during atrial fibrillation ablation. Heart Vessels 32, 1006–1012 (2017). https://doi.org/10.1007/s00380-017-0963-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-0963-x