Abstract
The prognostic significance of the SYNTAX (Synergy between PCI with Taxus and cardiac surgery) score has recently been demonstrated in patients with stable multivessel or left main coronary artery disease (CAD). The present study determines whether adding the SYNTAX score to Framingham risk score (FRS), left ventricular ejection fraction (LVEF) and presence of myocardial infarction (MI) by late gadolinium enhancement (LGE) magnetic resonance imaging can improve the risk stratification in patients with stable CAD. We calculated the SYNTAX score in 161 patients with stable CAD (mean age: 66 ± 10 years old). During a mean follow-up of 2.3 years, 56 (35 %) of 161 patients developed cardiovascular events defined as cardiovascular death, non-fatal MI, cerebral infarction, unstable angina pectoris, hospitalization due to heart failure and revascularization. Multivariate Cox regression analysis selected triglycerides [hazard ratio (HR): 1.005 (95 % confidence interval (CI): 1.001–1.008), p < 0.008], presence of LGE [HR: 6.329 (95 % CI: 2.662–15.05), p < 0.001] and the SYNTAX score [HR: 1.085 (95 % CI: 1.044–1.127), p < 0.001] as risk factors for future cardiovascular events. Adding the SYNTAX score to FRS, EF and LGE significantly improved the net reclassification index (NRI) [40.4 % (95 % CI: 18.1–54.8 %), p < 0.05] with an increase in C-statistics of 0.089 (from 0.707 to 0.796). An increase in C-statistics and significant improvement of NRI showed that adding the SYNTAX score to the FRS, LVEF and LGE incrementally improved risk stratification in patient with stable CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Synergy between PCI with Taxus and cardiac surgery (SYNTAX) score is an angiographic scoring system based on X-ray coronary angiography (CAG) which can evaluate anatomical complexity of the coronary arterial plaque [1]. Recently, the prognostic significance of the SYNTAX scores to predict future cardiovascular event has been demonstrated in patients with stable multivessel or left main coronary artery disease (CAD) [2] and acute coronary syndrome (ACS) [3]. Late gadolinium-enhanced (LGE) MRI allows for the accurate assessment of irreversible myocardial injury such as myocardial infarction (MI) or myocardial fibrosis [4, 5]. The transmural extent is useful as a marker of myocardial viability in infarcted myocardium [6]. Furthermore, presence of LGE is a strong prognostic predictor in patients with various cardiovascular diseases such as acute MI, stable CAD, unrecognized MI and cardiomyopathy [7–14].
In the current study, we hypothesized that adding the SYNTAX score to LGE MRI would improve the ability to predict the future cardiovascular events among patients with stable CAD. The purpose of this study was to investigate the incremental prognostic value of the SYNTAX score over LGE MRI in patients with stable CAD.
Materials and methods
Patients
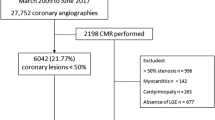
Figure 1 shows a flow chart of the study enrollment. Among 310 patients who were initially enrolled in this study, X-ray CAG confirmed the presence and absence of significant coronary artery stenosis in 139 and 171 patients. Significant coronary artery stenosis was defined as ≥50 % luminal narrowing on quantitative coronary angiography (QCA) images. All patients underwent cardiac MRI to evaluate their cardiac function and myocardial infarction. We excluded 139 patients without CAD from analysis. Ten patients each who were treated by coronary artery bypass graft surgery (CABG) were excluded. Finally, 161 stable CAD patients were enrolled in the final analysis (Fig. 1). This study was approved by the institutional review board, and all patients gave written informed consent to participate in this study.
Acquisition of MR images
We acquired MRI images using a 1.5-T MR scanner equipped with 32 channel cardiac coils (Achieva, Philips Healthcare, Best, The Netherlands). Cine MRI and LGE MRI were imaged in the entire study population.
Acquisition of cine MR images
Vector-electrocardiographic (VCG) monitoring leads were attached to supine patients and scout images were acquired in three orthogonal planes for cardiac orientation. Vertical and horizontal long-axis slices of cine MR images of the LV were acquired using a steady-state free precession (SSFP) sequence. The volume and mass of the LV were calculated from short-axis cine MR images acquired from the apex to the base of the LV (repetition time, 4.1 ms; echo time, 1.7 ms; flip angle, 55°; field of view, 350 × 350 mm; acquisition matrix, 128 × 128; slice thickness, 10 mm; number of phases per cardiac cycle, 20).
Acquisition of LGE MR images
The patients were injected with 0.15 mmol/kg of gadopentetate dimeglumine (Magnevist; Bayer Healthcare, Leverkusen, Germany). LGE MRI images were acquired 15 min after in the same planes as the cine images using inversion recovery—prepared gradient-echo sequences. The imaging parameters for late gadolinium-enhanced imaging were as follows: repetition time, 4.3 ms; echo time, 1.3 ms; flip angle, 15°; field of view, 380 × 380 mm; acquisition matrix, 256 × 180; and slice thickness, 10 mm. We detected the null point of the normal myocardium using a Look–Locker sequence.
X-ray coronary angiography
An observer who was blinded to the cardiac MRI results interpreted conventional X-ray CAG images using QangioXA quantitative software (Medis Inc., Raleigh, NC, USA). Patients received an intracoronary administration of isosorbide dinitrate (2–3 mg), then contrast agent was injected and the degree of coronary arterial stenosis was evaluated on the images using quantitative coronary angiography (QCA) analysis. Significant coronary arterial stenosis was defined as ≥50 % reduction in luminal diameter by QCA.
Data analysis
Analysis of cine MR and LGE MR images
Two observers used an Extend MR WorkSpace workstation (Philips Healthcare) to analyze the cine MR and LGE MR images. All images were rendered innominate and reviewed in random order. The LV epi- and endocardial borders on the short axis of cine MR images were manually traced with exclusion of the papillary muscles that encompassed the LV myocardium. The LV mass was then calculated by the consensus of two observers as the sum of the myocardial volume areas multiplied by the specific gravity (1.05 g/mL) of the myocardial tissue [15].
Late gadolinium enhancement was visually assessed and interpreted by the consensus of two observers who were blinded to the information about the patients. The LGE mass was measured on short-axis slices using manual planimetry method. The total LGE mass was calculated by summing the LGE mass of all sections, and the ratio (%) of LGE is expressed as:
None of the patients had atypical enhancement defined as mid-myocardial or sub-epicardial enhancement with multifocal distribution.
Calculation of the SYNTAX scores
Based on the quantitative CAG analysis, we defined significant coronary artery stenosis as ≥50 % narrowing of coronary artery diameter in at least one coronary artery. The SYNTAX score for each angiogram was independently evaluated by two experienced cardiologists who were blinded to the MRI results. Differences in opinion were resolved by the consensus of two cardiologists. Briefly, lesions that caused ≥50 % luminal narrowing in vessels ≥1.5 mm were defined based on the modified American Heart Association coronary tree segment classification and separately scored regarding bifurcations or trifurcations or aortic ostial localization, chronic occlusion, vessel tortuosity, length, calcification and thrombus formation. Finally, the lesion score was added to obtain the SYNTAX score for each patient. Observer who calculated the SYNTAX score was blinded to clinical information and MRI data. Occluded infarct-related arteries were scored as occlusions of unknown duration. A high SYNTAX score indicates complex coronary disease. We assessed the reproducibility of the SYNTAX scores in a random sample of 30 patients. The kappa values of assessment of the SYNTAX scores for intra- and interobserver agreement were 0.81 and 0.70, respectively.
Risk assessment calculated by FRS
Previous study using the FRS showed that 24.7 % patients with coronary artery disease or stroke will experience cardiovascular events during a 4-year follow-up [16]. We modified this risk assessment model and stratified the patients into low–intermediate, high or very high risk categories calculated as 2-year risk scores for primary and secondary prevention of <12 %, 12–25 % and >25 %, respectively.
Follow-up
Clinical information was obtained from hospital records and via telephone interviews of patients. Major adverse cardiac and cerebrovascular events included any of cardiovascular death, non-fatal MI, unstable angina requiring revascularization, cerebral infarction, hospitalization due to heart failure and revascularization (percutaneous coronary intervention or CABG). When a patient experienced more than one event, the first event was included in the analysis. When at least two events occurred simultaneously, the events were selected in the order of cardiovascular death > non-fatal MI > cerebral stroke > UAP > HF > revascularization.
Statistical analysis
Data were statistically analyzed using SPSS software, version 17.0 (SPSS, Inc., Chicago, IL, USA) and SAS version 9.2 (SAS Institute, Cary, NC, USA). Continuous values are shown as mean ± standard deviation (SD). Skewed values are presented as medians with interquartile ranges (IQR). Normality was determined using the Shapiro–Wilk test. Differences between groups were evaluated using an unpaired t test for normally distributed variables, and the Mann–Whitney U test for skewed variables. We calculated the cumulative incidence of events according to the presence or absence of LGE using the Kaplan–Meier method and compared the two curves using a log-rank test. We used Cox proportional hazards models to estimate HRs for cardiovascular events and 95 % confidence intervals (CI). Two-sided P < 0.05 was considered to indicate a significant difference. C-statistics for the Cox proportional hazards regression models were estimated. We evaluated whether adding the SYNTAX score to the FRS, EF and LGE incrementally improves the prediction of cardiovascular events using the net reclassification index. Low–intermediate, high risk and very high risk categories were defined as <12 %, 12–25 % and >25 %, respectively.
Results
Patient characteristics
Table 1 summarizes the characteristics of the patients (mean age, 66 ± 10 years), of whom 140 (87 %) were male. The prevalence of hypertension, dyslipidemia, diabetes mellitus, current smoking, family history of CAD and obesity were 65, 57, 21, 13, 7, 15 %, respectively. Blood test results for mean LDL cholesterol and mean HbA1c were 126 ± 36 mmol/L and 5.9 ± 1.2 %, respectively. Mean LVEF was 54 ± 15 %, and regional wall motion abnormalities (RWMA) were found in 31 (19 %) patients. Myocardial infarction was identified in 73 (45 %) patients and the mean % LGE was 8 ± 12 %. The mean FRS was 13 ± 6 and the mean SYNTAX score was 9 ± 7.
Cardiovascular events during follow-up
During a mean follow-up period of 2.3 years, 56 patients experienced cardiovascular events as follows: 2 cardiovascular death, 11 UAP, 2 cerebral infarction, 4 heart failure requiring hospitalization, 37 revascularization. Figure 2 shows Kaplan–Meier survival curves stratified by presence of LGE and the SYNTAX score. All patients (n = 161) were assigned to groups based on LGE and median SYNTAX score of 8. Kaplan–Meier survival curves for 161 patients with CAD revealed a significant difference in cumulative survival between those with and without LGE (p < 0.001; log-rank test) and with SYNTAX score >8 and ≤8 (p < 0.001; log-rank test). Figure 3 shows the Kaplan–Meier survival curves for patients with CAD assigned to groups based on median SYNTAX score and LGE [group 1, LGE (−) and the SYNTAX score ≤8; group 2, LGE (−) and the SYNTAX score >8; group 3, LGE (+) and the SYNTAX score ≤8; group 4, LGE (+) and the SYNTAX score >8]. Outcome was significantly better and significantly worse for groups 1 and 4, respectively, compared with the other groups (Fig. 3). Table 2 summarizes the results of Cox proportional hazard analyses for cardiovascular events. Univariate analysis selected triglycerides (HR, 1.004; 95 % CI, 1.001–1.008; p = 0.021), RWMA (HR, 2.160; 95 % CI, 1.247–3.743; p = 0.006), LGE (HR, 5.841; 95 % CI, 3.012–11.33; p < 0.001) and the SYNTAX score (HR, 1.104; 95 % CI, 1.070–1.139; p < 0.001) as significant predictors of cardiovascular events. Multivariate analysis selected triglycerides (HR, 1.005; 95 % CI, 1.001–1.008; p = 0.008), LGE (HR, 6.329; 95 % CI, 2.662–15.05; p < 0.001) and the SYNTAX score (HR, 1.085; 95 % CI, 1.044–1.127; p < 0.001).
Kaplan–Meier survival curves stratified by the SYNTAX score and LGE. Patients were divided into two groups based on presence or absence of LGE and median value of the SYNTAX score. Median value of the SYNTAX score was 8 for CAD patients. LGE late gadolinium-enhanced magnetic resonance imaging, CAD coronary artery disease
Net reclassification index and C-statistics for Cox proportional hazard models to predict cardiovascular events
Table 3 shows the results of C-statistics for Cox proportional hazard analysis to predict cardiovascular events. Adding the STNTAX score to the FRS, EF and presence of LGE resulted in an increase in the C-statistics. C-statistics for FRS + EF + LGE + the SYNTAX score was 0.796 (95 % CI, 0.723–0.865).
Table 4 shows reclassification according to the SYNTAX score in addition to FRS and EF. Adding the SYNTAX score significantly improved the net reclassification index (NRI) for those with CAD (60.1 %; 95 % CI, 38.7–81.5, p < 0.001). Table 5 show reclassification by adding the SYNTAX score to the FRS, EF and LGE MRI. Adding the SYNTAX score significantly improved the NRI in CAD patients (40.4 %; 95 % CI, 22.5–58.4; p < 0.001).
Discussion
To the best of our knowledge, this is the first study to assess the incremental increase in the prognostic significance of adding the SYNTAX score to LGE MRI, FRS and LVEF to predict cardiovascular events. The results in the current study indicated that the simultaneous assessment of extent of myocardial infarction by LGE MRI and coronary arterial atherosclerosis by the SYNTAX score would help to stratify patients with CAD who are at risk for cardiovascular events.
Prognostic value of the SYNTAX score in recent studies
The SYNTAX score was originally conceived as a mean of evaluating the complexity and severity of atherosclerosis of the coronary artery visualized by X-ray coronary CAG in patients with CAD [1]. Recent studies have shown that the SYNTAX score has prognostic significance for future cardiovascular events in patient with stable CAD, triple-vessel CAD and left main coronary arterial stenosis and ACS [2, 17–22]. Palmerini et al. [3] analyzed 2627 patients with non-ST segment elevation ACS who were treated by PCI from a subgroup of the ACUITY (acute catheterization and urgent intervention triage strategy) trial and found that the SYNTAX score is an independent and significant predictor of 1-year rates of death, cardiac death, MI and target vessel revascularization. However, to date, the number of evidences regarding prognostic significance of the SYNTAX score is relatively limited. Therefore, we conducted this study to investigate the prognostic value of the SYNTAX score in CAD patients and to compare directly with established prognostic marker, severity of myocardial infarction by LGE MRI.
Deleterious effects of LGE in cardiovascular diseases
Irreversible myocardial injury can be assessed accurately by LGE MRI. The spatial resolution of LGE MRI is higher than that of myocardial single-photon emission computed tomography (SPECT) imaging [6]. Previous studies showed that the presence of LGE is a powerful prognostic marker of various cardiovascular diseases [23–25]. For example, myocardial scar on LGE is associated with a poor response to beta-blocker therapy [26] and revascularization (PCI or CABG) [4, 27]. Scott et al. [28] reported that the extent of LV scar quantified by LGE MRI is associated with spontaneous ventricular arrhythmia in patients with CAD and implantable cardiac defibrillators (ICD). Moreo et al. [29] showed a significant relationship between diastolic dysfunction evaluated by Doppler echocardiography and LGE on MRI and Wong et al. [30] showed a relationship between LGE and hospitalization of heart failure. Furthermore, unrecognized MI detected by LGE MRI has prognostic value in patients without clinical evidence of MI [7, 14]. The hazardous effect of LGE MRI was also observed in the current study.
Clinical implications
Here, we showed that an integrated approach using FRS, EF, LGE MRI and the SYNTAX score can predict future cardiovascular events with C-statistics of 0.796 in patients with known CAD. Although the incremental prognostic value of the SYNTAX score was statistically significant, the magnitude of increment in C-statistics is relatively small (increment of C-statistics = 0.089, Table 3). We believe that main finding of this study is that the SYNTAX score is not necessarily useful as an isolated prognostic predictor, however, when we used the SYNTAX score combined with LGE MRI, it might be useful as a reliable marker which can identify patients who is going to have worse prognosis compared to patients without LGE and with low SYNTAX score.
Study limitation
This single-center retrospective study had a relatively small patient cohort and thus our results require clarification in a multicenter study of a larger population. Although LGE MRI is non-invasive and useful for risk stratification, MRI is contraindicated for patients implanted with pacemakers or cardiovascular defibrillators and those with claustrophobia. Such patients were excluded from the present study. In the study done by Kelle et al. [31], the presence of inducible wall motion abnormality and LGE independently identify patients at increased risk for subsequent cardiac events. The assessment of myocardial ischemia is vital for the risk stratification of CAD patients. Further study is necessary to investigate if the SYNTAX score has incremental prognostic significance over the myocardial ischemia detected by MRI imaging (e.g., inducible wall motion abnormality by cine MRI or pharmacological stress perfusion MRI). Another limitation of this study is that we excluded patients treated with CABG. In the current study, number of CABG patients was relatively small to assess the prognostic value. Therefore, we excluded these patients and focused to assess prognosis in patients with low to moderate SYNTAX score. Further study is necessary to elucidate if the SYNTAX score has incremental prognostic value over LGE MRI in patients with high SYNTAX score. In addition, not all the patients were treated with FFR-guided PCI. FFR can provide us an appropriate indication of PCI procedure. Further study is necessary to investigate if the combination of the SYNTAX score and LGE can predict the occurrence of PCI for FFR-evidenced myocardial ischemia.
Conclusion
An increase in C-statistics showed that adding the SYNTAX score to the Framingham risk model, LVEF and LGE MRI incrementally improved risk stratification. An integrated approach using LGE MRI and the SYNTAX score might be useful for predicting vulnerable patients to develop the future cardiovascular events.
References
Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, van den Brand M, Van Dyck N, Russell ME, Mohr FW, Serruys PW (2005) The syntax score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1:219–227
Serruys PW, Onuma Y, Garg S, Vranckx P, De Bruyne B, Morice MC, Colombo A, Macaya C, Richardt G, Fajadet J, Hamm C, Schuijer M, Rademaker T, Wittebols K, Stoll HP (2010) 5-year clinical outcomes of the ARTS II (arterial revascularization therapies study II) of the sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. J Am Coll Cardiol 55:1093–1101
Palmerini T, Genereux P, Caixeta A, Cristea E, Lansky A, Mehran R, Dangas G, Lazar D, Sanchez R, Fahy M, Xu K, Stone GW (2011) Prognostic value of the syntax score in patients with acute coronary syndromes undergoing percutaneous coronary intervention: analysis from the acuity (acute catheterization and urgent intervention triage strategy) trial. J Am Coll Cardiol 57:2389–2397
Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM (2000) The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 343:1445–1453
Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, Bundy J, Finn JP, Klocke FJ, Judd RM (1999) Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 100:1992–2002
Wagner A, Mahrholdt H, Holly TA, Elliott MD, Regenfus M, Parker M, Klocke FJ, Bonow RO, Kim RJ, Judd RM (2003) Contrast-enhanced MRI and routine single photon emission computed tomography (spect) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet 361:374–379
Kwong RY, Chan AK, Brown KA, Chan CW, Reynolds HG, Tsang S, Davis RB (2006) Impact of unrecognized myocardial scar detected by cardiac magnetic resonance imaging on event-free survival in patients presenting with signs or symptoms of coronary artery disease. Circulation 113:2733–2743
Wu KC, Zerhouni EA, Judd RM, Lugo-Olivieri CH, Barouch LA, Schulman SP, Blumenthal RS, Lima JA (1998) Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation 97:765–772
Assomull RG, Prasad SK, Lyne J, Smith G, Burman ED, Khan M, Sheppard MN, Poole-Wilson PA, Pennell DJ (2006) Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 48:1977–1985
Wu KC, Weiss RG, Thiemann DR, Kitagawa K, Schmidt A, Dalal D, Lai S, Bluemke DA, Gerstenblith G, Marban E, Tomaselli GF, Lima JA (2008) Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J Am Coll Cardiol 51:2414–2421
Patel MR, Cawley PJ, Heitner JF, Klem I, Parker MA, Jaroudi WA, Meine TJ, White JB, Elliott MD, Kim HW, Judd RM, Kim RJ (2009) Detection of myocardial damage in patients with sarcoidosis. Circulation 120:1969–1977
Bruder O, Wagner A, Jensen CJ, Schneider S, Ong P, Kispert EM, Nassenstein K, Schlosser T, Sabin GV, Sechtem U, Mahrholdt H (2010) Myocardial scar visualized by cardiovascular magnetic resonance imaging predicts major adverse events in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 56:875–887
O’Hanlon R, Grasso A, Roughton M, Moon JC, Clark S, Wage R, Webb J, Kulkarni M, Dawson D, Sulaibeekh L, Chandrasekaran B, Bucciarelli-Ducci C, Pasquale F, Cowie MR, McKenna WJ, Sheppard MN, Elliott PM, Pennell DJ, Prasad SK (2010) Prognostic significance of myocardial fibrosis in hypertrophic cardiomyopathy. J Am Coll Cardiol 56:867–874
Kwong RY, Sattar H, Wu H, Vorobiof G, Gandla V, Steel K, Siu S, Brown KA (2008) Incidence and prognostic implication of unrecognized myocardial scar characterized by cardiac magnetic resonance in diabetic patients without clinical evidence of myocardial infarction. Circulation 118:1011–1020
Semelka RC, Tomei E, Wagner S, Mayo J, Kondo C, Suzuki J, Caputo GR, Higgins CB (1990) Normal left ventricular dimensions and function: interstudy reproducibility of measurements with cine mr imaging. Radiology 174:763–768
D’Agostino RB, Russell MW, Huse DM, Ellison RC, Silbershatz H, Wilson PW, Hartz SC (2000) Primary and subsequent coronary risk appraisal: new results from the Framingham study. Am Heart J 139:272–281
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW (2009) Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 360:961–972
Capodanno D, Di Salvo ME, Cincotta G, Miano M, Tamburino C (2009) Usefulness of the syntax score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv 2:302–308
Chen SL, Chen JP, Mintz G, Xu B, Kan J, Ye F, Zhang J, Sun X, Xu Y, Jiang Q, Zhang A, Stone GW (2010) Comparison between the ners (new risk stratification) score and the syntax (synergy between percutaneous coronary intervention with taxus and cardiac surgery) score in outcome prediction for unprotected left main stenting. JACC Cardiovasc Interv 3:632–641
Kim YH, Park DW, Kim WJ, Lee JY, Yun SC, Kang SJ, Lee SW, Lee CW, Hong MK, Park SW, Park SJ (2010) Impact of the extent of coronary artery disease on outcomes after revascularization for unprotected left main coronary artery stenosis. J Am Coll Cardiol 55:2544–2552
Onuma Y, Girasis C, Piazza N, Garcia-Garcia HM, Kukreja N, Garg S, Eindhoven J, Cheng JM, Valgimigli M, van Domburg R, Serruys PW (2010) Long-term clinical results following stenting of the left main stem: insights from RESEARCH (rapamycin-eluting stent evaluated at rotterdam cardiology hospital) and T-SEARCH (taxus-stent evaluated at rotterdam cardiology hospital) Registries. JACC Cardiovasc Interv 3:584–594
Valgimigli M, Serruys PW, Tsuchida K, Vaina S, Morel MA, van den Brand MJ, Colombo A, Morice MC, Dawkins K, de Bruyne B, Kornowski R, de Servi S, Guagliumi G, Jukema JW, Mohr FW, Kappetein AP, Wittebols K, Stoll HP, Boersma E, Parrinello G (2007) Cyphering the complexity of coronary artery disease using the syntax score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol 99:1072–1081
Funada A, Kanzaki H, Noguchi T, Morita Y, Sugano Y, Ohara T, Hasegawa T, Hashimura H, Ishibashi-Ueda H, Kitakaze M, Yasuda S, Ogawa H, Anzai T (2015) Prognostic significance of late gadolinium enhancement quantification in cardiac magnetic resonance imaging of hypertrophic cardiomyopathy with systolic dysfunction. Heart Vessels. doi:10.1007/s00380-015-0670-4
Nabeta T, Inomata T, Iida Y, Ikeda Y, Iwamoto M, Ishii S, Sato T, Watanabe I, Naruke T, Shinagawa H, Koitabashi T, Takeuchi I, Nishii M, Inoue Y, Izumi T (2014) Baseline cardiac magnetic resonance imaging versus baseline endomyocardial biopsy for the prediction of left ventricular reverse remodeling and prognosis in response to therapy in patients with idiopathic dilated cardiomyopathy. Heart Vessels 29:784–792
Sano M, Satoh H, Suwa K, Nobuhara M, Saitoh T, Saotome M, Urushida T, Katoh H, Shimoyama K, Suzuki D, Ogawa N, Takehara Y, Sakahara H, Hayashi H (2014) Characteristics and clinical relevance of late gadolinium enhancement in cardiac magnetic resonance in patients with systemic sclerosis. Heart Vessels. doi:10.1007/s00380-014-0539-y
Bello D, Shah DJ, Farah GM, Di Luzio S, Parker M, Johnson MR, Cotts WG, Klocke FJ, Bonow RO, Judd RM, Gheorghiade M, Kim RJ (2003) Gadolinium cardiovascular magnetic resonance predicts reversible myocardial dysfunction and remodeling in patients with heart failure undergoing beta-blocker therapy. Circulation 108:1945–1953
Selvanayagam JB, Kardos A, Francis JM, Wiesmann F, Petersen SE, Taggart DP, Neubauer S (2004) Value of delayed-enhancement cardiovascular magnetic resonance imaging in predicting myocardial viability after surgical revascularization. Circulation 110:1535–1541
Scott PA, Morgan JM, Carroll N, Murday DC, Roberts PR, Peebles CR, Harden SP, Curzen NP (2011) The extent of left ventricular scar quantified by late gadolinium enhancement MRI is associated with spontaneous ventricular arrhythmias in patients with coronary artery disease and implantable cardioverter-defibrillators. Circ Arrhythm Electrophysiol 4:324–330
Moreo A, Ambrosio G, De Chiara B, Pu M, Tran T, Mauri F, Raman SV (2009) Influence of myocardial fibrosis on left ventricular diastolic function: noninvasive assessment by cardiac magnetic resonance and echo. Circ Cardiovasc Imag 2:437–443
Wong TC, Piehler KM, Zareba KM, Lin K, Phrampus A, Patel A, Moon JC, Ugander M, Valeti U, Holtz JE, Fu B, Chang CC, Mathier M, Kellman P, Butler J, Gheorghiade M, Schelbert EB (2013) Myocardial damage detected by late gadolinium enhancement cardiovascular magnetic resonance is associated with subsequent hospitalization for heart failure. J Am Heart Assoc 2:e000416
Kelle S, Nagel E, Voss A, Hofmann N, Gitsioudis G, Buss SJ, Chiribiri A, Wellnhofer E, Klein C, Schneeweis C, Egnell C, Vierecke J, Berger A, Giannitsis E, Fleck E, Katus HA, Korosoglou G (2013) A bi-center cardiovascular magnetic resonance prognosis study focusing on dobutamine wall motion and late gadolinium enhancement in 3138 consecutive patients. J Am Coll Cardiol 61:2310–2312
Acknowledgments
We are grateful to Hiroshi Hayashi, RT and Yukihiro Ishii, RT (Department of Radiology, Kanagawa Cardiovascular and Respiratory Center) for their technical assistance.
Conflict of interest
There are no conflicts of interest to declare.
Disclosure
Shingo Kato, MD, PhD: Scholarship from Banyu Life Science Foundation International. Satoshi Umemura, MD, PhD: Research support or honoraria or both from Astellas Pharm Inc., AstraZeneca K.K., Bayer Yakuhin, Ltd., Boehringer Ingelheim Japan, Inc., Chugai Pharmaceutical Co., Ltd., Daiichi-Sankyou Company, Limited, Dainippon Sumitimo Pharma Co., Ltd., Kowa Company, Ltd., MSD K.K., Novartis Pharma K.K., Otsuka Pharmaceutical Co., Ltd., Pfizer Japan Inc., Sanofi K.K., Takeda Pharmaceutical Company,, Torii Pharmaceutical Co.,Ltd., Shionogi & Co. Ltd., Kyouwa-Hakkou-Kirin Co. Ltd.,, Mochida Pharmaceutical Co. Ltd.,, Mitsubishi Tanabe Pharma Corporation, Teijin Pharma Ltd.,, Acterion Pharmaceuticals Japan Ltd., Sanwa-Kagaku Kenkyusho Co. Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kato, S., Saito, N., Kirigaya, H. et al. Incremental prognostic value of the SYNTAX score to late gadolinium-enhanced magnetic resonance images for patients with stable coronary artery disease. Heart Vessels 31, 871–880 (2016). https://doi.org/10.1007/s00380-015-0685-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-015-0685-x