Abstract
Late recovery of sinus rhythm is unusual in patients with permanent AF treated by (radiofrequency) RF maze procedure during mitral valve surgery. Identification of clinical and instrumental preoperative factors predictive of early success of RF ablation in patients with permanent AF undergoing mitral valve surgery may improve selection of subjects to obtain long-term results. Hundred and thirty consecutive patients with permanent AF and mitral valve disease underwent modified RF maze procedure during concomitant mitral valve surgery. Rheumatic valve disease (61 pts) and mitral valve prolapse (41 pts) were the more common aetiology of valve abnormalities. Mitral valve replacement was performed in 54 % of patients and mitral valve repair in the remaining 46 %. Four patients died after surgery. At discharge, 87 patients (69 %) were in sinus rhythm (group 1) and 43 patients in AF persisted (group 2). At an average 24-month follow-up, sinus rhythm was present in 67 % of patients, and 33 % were in atrial fibrillation. In this period, late recovery of sinus rhythm was observed only in five patients, while eight discharged in sinus rhythm developed again atrial fibrillation. Among preoperative parameters at univariate analysis female sex, atrial fibrillation >24 months, left atrial diameter >54 mm, left atrial area >24 cm2, rheumatic valve disease and NYHA class were associated with persistence of AF. At Cox regression multivariate analysis, increased left atrial area (OR 1.07 per unit increase—95 % CI 1.01–1.131) and rheumatic aetiology of valve disease (OR 4.52, 95 % CI 1.65–12.4) were associated with persistence of AF at hospital discharge. Persistence of AF after RF ablation in patients undergoing mitral valve surgery is related to aetiology, e.g. rheumatic valve disease, and to increasing left atrial diameter. Due to low rate of late recovery of sinus rhythm, indication to RF ablation associated with MV surgery should be carefully considered in patients with large atria and rheumatic mitral valve disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spontaneous sinus rhythm recovery occurs in not more than 10 % of patients with mitral valve disease undergoing mitral valve surgery [1–3]. Persistence of atrial fibrillation (AF) after surgery is associated with an increased risk of systemic embolization, with a decreased exercise tolerance and with an higher long-term mortality [4–6]. Modified Cox maze radiofrequency (RF) ablation has been demonstrated to be highly effective in the treatment of AF associated with valve diseases [7, 8]. Favourable long-term results of RF ablation have been reported in several studies; however, few information exists on the clinical and echocardiographic variables related to the early success of treatment (at hospital discharge) in patients undergoing RF ablation of permanent AF associated with mitral valve surgery. The identification of “early responders” may be useful to clarify clinical indication to RF ablation procedure and to decrease the need and the related costs of re-hospitalization for sinus rhythm restoration attempts in patients with early failure of ablation procedure. This aspect appears of particular relevance considering that the number of “late responders”, e.g. of patients who recover sinus rhythm in the period after hospital discharge, from previous experiences seems to be limited [9] at least in patients treated with monopolar RF ablation. Aim of the present study was to investigate which factors may be related to sinus rhythm restoration at hospital discharge by the RF maze procedure in permanent atrial fibrillation patients undergoing concomitant mitral valve surgery.
Materials and methods
Patient population
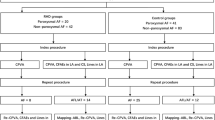
Between January 2005 and June 2011, 130 patients with permanent AF (atrial fibrillation lasting at least 6 months after the last attempt of sinus rhythm restoration) and mitral valve disease underwent the maze procedure utilizing RF energy, while undergoing concomitant mitral valve surgery. Fifty-three were men and 77 women, and mean age was 67 (± 9 years). Preoperative duration of AF ranged from 6 to 254 months (Table 1). End point of the study was to identify clinical factors associated with early success of RF maze procedure, defined as persistence in sinus rhythm or correct dual-chamber stimulation in patients with permanent pacemaker at hospital discharge. Before surgery, none of these patients were in amiodarone treatment; 82 % were treated with beta-blockers and 87 % with ACE-inhibitors or AT1 receptor inhibitors. All patients were on oral anticoagulation with K vitamin inhibitors. Rheumatic valve disease (61 pts—47 %) and mitral valve prolapse (41pts—30 %) were the more common diagnosed valve abnormalities. Detailed etiologic distribution is reported in Fig. 1. At hospital admission, 14 % patients were in NYHA functional class IV, 61 % patients were in class III, and 22 % patients were in NYHA functional class II. Mitral valve replacement was performed in 54 % (St Jude bileaflet mechanical valve in 52 %, Carpentier–Edwards biologic valve in 48 %), and mitral valve repair in 46 %. Tricuspid valve repair (25 patients), coronary artery bypass graft surgery (35 patients) and aortic valve replacement (20 patients) were the more frequently associated procedures. Informed consent was obtained from each patient. The study protocol was approved by the Institutional Review Committee on Human Research in our institution.
Maze procedure
The Medtronic Cardioablate surgical ablation system (Medtronic, Minneapolis USA) was used for treatment. Access to the inside of the left atrium was gained through a standard atriotomy in the interatrial groove. After the left atrial appendage (LAA) was excised, an ablation line from the LAA to the left superior pulmonary vein was created. In addition to the incision in the interatrial groove, isolation of the right pulmonary veins was completed by a circular ablation line. The left pulmonary veins were encircled. Two linear ablations were performed endocardially. The first connected the two encirclings to the postero-superior atrial wall. This lesion was kept cranial, opposite the transverse sinus, to prevent any possible damage to the oesophagus. The last ablation connected the left appendage to the posterior aspect of the mitral annulus. To protect the circumflex artery from heat trauma, the lesion line reached the mitral posterior annulus far from the antero-lateral commissure. Transesophageal echocardiographic probe was removed during the ablation to prevent any damage by the transmission of the heat waves to the oesophagus. The mitral valve procedure was completed, and the left atriotomy was sutured in the standard fashion. Surgical times and surgery-related complications are reported in Table 2.
Postoperative management
Amiodarone was used for postoperative antiarrhythmic prophylaxis. An intravenous bolus of 300 mg was followed by a continuous infusion of 1,200 mg for the first 24 h. Oral administration (200 mg every 8 h) was maintained until discharge. Maintenance regimen of 200 mg/d was then prescribed for a period of 3 months.
Weight-adjusted LMWH was administered subcutaneously b.i.d. starting 12 h after ICU admission. At drainage, tube removal warfarin was started (5 mg daily) and dosage was adjusted to reach target anticoagulation regimen. Low molecular weight heparin was withdrawn 24 h thereafter.
ECG monitoring
Cardiac rhythm was continuously monitored after surgery. Dual-chamber stimulation at 80 beats/minute through epicardial temporary pacing wires was used in most of patients for the first 48 h postoperatively to avoid severe brady arrhythmias. Recurrences of atrial fibrillation after surgery were treated by resuming amiodarone infusion and correcting, in the case, electrolyte abnormalities. In patients in whom AF persisted despite optimal medical therapy, at least one attempt of external DC-shock was performed before discharge. 12/51 patients recovered sinus rhythm after an average of 1.6 shocks.
Echocardiography
Echocardiographic examination was performed in left lateral position using a Sequoia Acuson instrument (Siemens Medical Solution, Mountain View, California with 2.5 and 3.5 MHz probes). Left and right atrial areas were measured by planimetry in the four-chamber view, and maximum areas were measured (at the end of the T wave on the ECG). Averaged of five beats was considered for statistical analysis. Left ventricular ejection fraction was measured by area–length method. Mean pulmonary artery pressure was calculated by acceleration time. Systolic pulmonary artery pressure was estimated measuring transvalvular gradient by maximal velocity of CW tricuspid flow plus right atrial pressure.
Follow-up
Patients were followed up for an average of 24 months. A telephonic questionnaire was administered to patients who were not able to undergo outpatients visit at our institution. End point of the study was the evaluation of recurrence of atrial fibrillation.
Statistical analysis
Values for continuous variables were given as the mean ± SD. Categoric variables were compared using the χ2 test or the Fisher exact test (two tailed). Multivariate analysis was performed using stepwise Cox regression method. Statistical analysis was performed with the use of a statistical software program (SPSS 18.0 software: SPSS Inc. Chicago, Illinois). A probability value of <0.05 was considered to be statistically significant.
Results
Four patients died during hospitalization (3 %), one due to cerebral haemorrhage on third postoperative day, two due to unresponsive cardiogenic shock and the last one as consequence of multiorgan failure due to sepsis 12 days after surgery. Two patients with sick sinus syndrome were treated with permanent pacemaker implantation.
The analysis was conducted on 126 patients discharged alive from hospital. At discharge, 87 (69 %), including the two who underwent successful dual-chamber pace maker implantation, were in sinus rhythm, while the remnant 39 (31 %) were still in atrial fibrillation.
At an average 24-month follow-up, sinus rhythm was present in 67 % of patients, and 33 % were in atrial fibrillation. In this period, late recovery of sinus rhythm was observed only in five patients, while eight discharged in sinus rhythm developed again atrial fibrillation.
Univariate analysis (Table 3) showed an early higher rate of RF ablation success in male patients. Restoration of sinus rhythm after maze procedure was observed more frequently in patients with a duration of documented AF lower than 24 months (p = 0.013). Smaller left atrial diameter and area (<52 mm and, respectively, 24 square cm) were associated with a significantly higher probability of sinus rhythm recovery.
By converse rheumatic aetiology of mitral valve disease was associated with an highly significant probability of procedural failure (84 % of patients with degenerative or ischaemic valve regurgitation were discharged in SR in comparison with 59 % of patients with rheumatic valve disease, p = 0.008) (Figs. 2, 3). Only 7 % of patients with preoperative NYHA functional class II were discharged in AF in comparison with 33 % in III–IV NYHA class patients. The type of surgical procedure did not significantly affect the rate of sinus rhythm restoration at hospital discharge. Finally, use of angiotensin-converting enzyme inhibitors, digoxin, ß-blockade, and calcium-channel blockers, the presence hypertension, hyperthyroidism, diabetes mellitus, preoperative left ventricular diameter and left ventricular ejection fraction did not affect the results.
By multiple stepwise logistic regression analysis, only preoperative left atrial area (odds ratio, 1.07 per each unit increase; 95 % confidence interval, 1.01–1.131; p < 0.005) and rheumatic aetiology of mitral valve disease (odds ratio, 4.52; 95 % confidence interval, 1.65–12.4; p < 0.005) were independently related to the risk of persistence of AF at discharge after RF maze procedure (Fig. 4). In patients with rheumatic mitral valve disease and left atrium area >24 cm2, only 20 % were in sinus rhythm at discharge.
Discussion
Radiofrequency ablation is an efficient option to treat chronic atrial fibrillation in mitral valve surgery [10]. Kosakai et al. [11] reported an higher three-year survival rate, a threefold more frequent presence of sinus rhythm (75 vs 36 %) and an absolute 25 % decrease in the risk of stroke in a group of patients treated with radiofrequency ablation in comparison with a clinical comparable historical group in which only valve surgery was performed. A randomized double-blind study showed at 1-year follow-up a significantly higher number of patients in sinus rhythm (44.4 %) in subjects randomized to radiofrequency ablation procedure in comparison with mitral valve surgery alone (4.5 %) despite a similar rate of postoperative complications and deaths [12]. Restoration of sinus rhythm is observed in less than 10 % of patients with mitral valve disease and chronic atrial fibrillation undergoing isolated mitral surgery [13]. Late (after hospital discharge) recovery of SR in patients who underwent RF treatment of AF is not frequent [9]. In our investigation, only 5/126 patients recovered sinus rhythm at an average follow-up period of 24 months. Close follow-up and further hospital admission for attempt of sinus rhythm restoration may be considered in non-responders, but add additional economic charges and are associated with low success rate. Thus, identification of predictive factors related to successful result at hospital discharge may be useful in selection of patients for RF maze procedure in association with mitral valve surgery. In present investigation, we found that the only independent factors related to failure of sinus conversion by the RF maze procedure in patients with permanent AF and mitral valve disease were preoperative left atrial area and rheumatic aetiology of mitral valve disease. Male sex, duration of AF <24 months, and a lower NYHA functional class were associated with an higher percentage of SR restoration after RF ablation, but none had independent predictive value at multivariate analysis. Left atrial dimension, AF duration and LVEF have been the more frequent independent factors associated with long-term RF results. Previous investigations suggest that in patients with AF and mitral valve disease undergoing surgical maze operation, a lower sinus conversion rate was associated with a larger left atrial diameter [10]. More recently, Williams et al. [14] reported that a preoperative left atrial area of 56.25 cm2 or a preoperative left atrial diameter of 57.8 mm could discriminate between responders and non-responders. Rheumatic mitral valve disease has been demonstrated to be an independent factor related to a lower success rate after RF ablation of AF [15, 16]. Spotted focal areas of micro-reentry-inducing AF may be related to fibrotic exits of inflammatory disease of atrial muscular fibres. Efficacy of usual RF ablation lines in focal AF may be limited, and mapping of atrial electric activity during surgery may be useful [17, 18]. Novel circumferential lines of ablation may improve clinical results [19]. In our investigation, only 59 % of patients undergoing surgery for rheumatic mitral valve disease were discharged in sinus rhythm after RF ablation in comparison with 84 % of mitral valve disease related to different aetiologies. An higher success rate in rheumatic valve disease has been reported by Sternik et al. [20].
Study limitations
The present study was limited by its observational nature, by a relative short follow-up period (2 years) and by the number of patients investigated. Similar to other studies, a related potential bias results from the reliance on self-reporting for follow-up cardiac rhythm data. The use of questionnaires and clinical examination during follow-up may not accurately identify paroxysmal episodes of AF and may potentially have underestimated the incidence of arrhythmia recurrences.
Conclusions
Results from present investigation suggest that in patients with permanent atrial fibrillation, rheumatic aetiology and enlarged left atrium significantly decrease the success rate of RF ablation in patients undergoing mitral valve surgery. Moreover, duration of AF significantly affects outcome of treatment although we failed to demonstrate an independent predictive value for this factor. Low rate of sinus rhythm recovery at follow-up confirm results of previous investigations. Thus, identification of clinical factors associated with a low success rate of RF ablation at hospital discharge may help to improve the selection of patients eligible for treatment. Our data suggest that indication to treatment should be carefully weighted in patients with enlarged left atrium and rheumatic valve disease in particular when duration of AF before surgery is longer than 24 months. The probability of sinus rhythm recovery at discharge is lower than 15 %, and AF recurrence is not negligible in these patients.
References
Kernis SJ, Nkomo VT, Messika-Zeitoun D, Gersh BJ, Sundt TM 3rd, Ballman KV, Scott CG, Schaff HV, Enriquez-Sarano M (2004) Atrial fibrillation after surgical correction of mitral regurgitation in sinus rhythm: incidence, outcome, and determinants. Circulation 110:2320 –2325
Obadia JF, el Farra M, Bastien OH, Lièvre M, Martelloni Y, Chassignolle JF (1997) Outcome of atrial fibrillation after mitral valve repair. J Thorac Cardiovasc Surg 114(2):179-185
Lim E, Barlow CW, Hosseinpour AR, Wisbey C, Wilson K, Pidgeon W, Charman S, Barlow JB, Wells FC (2001) Influence of atrial fibrillation on outcome following mitral valve repair. Circulation 104(12 Suppl 1):I59
Raanani E, Albage A, David TE, Yau TM, Armstrong S (2001) The efficacy of the Cox/maze procedure combined with mitral valve surgery: a matched control study. Eur J Cardiothorac Surg 19:438-442
Khargi K, Hutten BA, Lemke B, Deneke T (2005) Surgical treatment of atrial fibrillation: a systemic review. Eur J Cardiothorac Surg 27:258-265
Reston JT, Shuhaiber JH (2005) Meta-analysis of clinical outcomes of maze-related surgicalprocedures for medically refractory atrial fibrillation. Eur J Cardiothor Surg 28: 724-730
Sie HT, Beukema, WP, Misier, AR, Elvan A, Ennema JJ, Haalebos MM, Wellens HJ (2001) Radiofrequency modified maze in patients with atrial fibrillation undergoing concomitant cardiac surgery. J Thorac Cardiovasc Surg 122:249-256
Wong JJW, Mak KH (2006) Impact of Maze and Concomitant Mitral Valve Surgery on Clinical Outcomes. Ann Thorac Surg 82:1938-1947
Benussi S (2004) Treatment of atrial fibrillation. Eur J Cardiothorac Surg 26 (suppl 1):S39- S41
Fukuda Y, Yoshida T, Inage T, Takeuchi T, Gondo T, Takii E, Imaizumi T (2012) Long-term results of the maze procedure on left ventricular function for persistentatrial fibrillation associated with mitral valve disease. Heart Vessels 27(1):53-57
Kosakai Y (2000) Treatment of atrial fibrillation using the maze procedure: the Japanese experience. Semin Thorac Cardiovasc Surg 12:44-52
Shin SH, Park MY, Oh WJ, Hong SJ, Pak HN, Song WH, Lim DS, Kim YH, Shim WJ (2008) Left atrial volume is a predictor of atrial fibrillation recurrence after catheter ablation. J Am Soc Echocardiogr 21(6):697-702
Budera P, Straka Z, Osmančík P,, Vaněk T, Jelínek Š, Hlavička J, Fojt R, Červinka P, Hulman M, Šmíd M, Malý M, Widimský P (2012) Comparison of cardiac surgery with left atrial surgical ablation vs. cardiac surgery without atrial ablation in patients with coronary and/or valvular heart disease plus atrial fibrillation: final results of the PRAGUE-12 randomized multicentre study Eur Heart J 33(21): 2644–2652
Williams MR, Stewart JR, Bolling SF, Freeman S, Anderson JT, Argenziano M, Smith CR, Oz MC (2001) Surgical treatment of atrial fibrillation using radiofrequency energy. Ann Thorac Surg 71: 1939-1944
Chen MC, Chang JP, Chang HW, Chen CJ, Yang CH, Chen YH, Fu M (2005) Clinical determinants of sinus conversion by radiofrequency maze procedure for persistent atrial fibrillation in patients undergoing concomitant mitral valvular surgery. Am J Cardiol 96:1553-1557
Mataraci I, Polat A, Mert B, Aydin C, Kirali K (2010) Radiofrequency ablation for atrial fibrillation in rheumatic valvular disease. Heart Lung Circ 9(1):43-49
Yoshihara F, Nishikimi T, Sasako Y, Hino J, Kobayashi J, Minatoya K, Bando K, Kosakai Y, Horio T, Suga S, Kawano Y, Matsuoka H, Yutani C, Matsuo H, Kitamura S, Ohe T, Kangawa K (2002) Plasma atrial natriuretic peptide concentration inversely correlates with left atrial collagen volume fraction in patients with atrial fibrillation: plasma ANP as a possible biochemical marker to predict the outcome of the maze procedure. J Am Coll Cardiol 39(2):288-294
Kataoka T, Hamasaki S, Inoue K, Yuasa T, Tomita K, Ishida S, Ogawa M, Saihara K, Koriyama C, Nobuyoshi M, Sakata R, Tei C (2010) Left atrium volume index and pathological features of left atrial appendage as a predictor of failure in postoperative sinus conversion. J Cardiol 55 (2):274-282
Jiang Z, Yin H, He Y, Ma N, Tang M, Liu H, Ding F, Mei J. (2014) Efficacy and safety of novel epicardial circumferential left atrial ablation ewith pulmonary vein isolation in sustained atrial fibrillation. Heart Vessels. doi: 10.1007/s00380-014-0594-4
Sternik L, Luria D, Glikson M, Malachy A, First M, Raanani E (2010) Efficacy of surgical ablation of atrial fibrillation in patients with rheumatic heart disease. Ann Thorac Surg 89 (5):1437-1442
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rostagno, C., Gelsomino, S., Capecchi, I. et al. Factors related to sinus rhythm at discharge after radiofrequency ablation of permanent atrial fibrillation in patients undergoing mitral valve surgery. Heart Vessels 31, 593–598 (2016). https://doi.org/10.1007/s00380-015-0647-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-015-0647-3