Abstract
Mechanisms of saliva formation by wombat parotid glands were investigated in anaesthetized wombats at two levels of cholinergically-stimulated flow viz. mid-range (30–40% maximum flow) and maximum flow using ion-transport and carbonic-anhydrase inhibitors. Bumetanide (0.005–0.1 mmol l−1 carotid plasma) progressively reduced mid-range flow by 52 ± 3.4% (mean ± SEM). Concurrently, saliva [Cl] decreased, [Na] and [HCO3] increased but HCO3 excretion was unaltered. Salivary flow during high-rate cholinergic stimulation was 31 ± 1.1% of the pre-bumetanide maximum. During mid-range stimulation, SITS (0.075 mmol l−1) was without effect whereas 0.75 mmol l−1 stimulated transient increases in fluid output. The higher SITS concentration caused no alterations to flow or electrolyte concentrations during maximal stimulation. Carotid plasma [amiloride] (0.05 mmol l−1) caused immediate falls in flow rate of 20–30% followed by progressive recovery over 25 min to levels above pre-amiloride flow rates despite plasma [amiloride] increasing tenfold. Concurrently, salivary [Na] and [Cl] rose to equal plasma concentrations and [K] fell by 50% indicating blockade of acinar Na/H exchangers and luminal Na channels in the ducts. Increased salivary osmolarity caused the flow recovery. Saliva flow during maximum cholinergic stimulation was reduced by 38–46%. The depression of flow was interpreted as resulting from competition between amiloride and acetylcholine for access to the muscarinic receptors. Plasma [acetazolamide] (0.35–2.5 mmol l−1) did not alter saliva outflow during mid-range or maximum flow regimes whereas salivary [Cl] increased and [HCO3] decreased consistent with reduced anion exchange resulting from inhibition of carbonic anhydrase. Combined with bumetanide, acetazolamide (1.5 mmol l−1) reduced flow by an additional 18–22% relative to bumetanide alone thereby demonstrating that acinar HCO3 synthesis supported a limited proportion of saliva formation and that some HCO3 secretion was independent of carbonic anhydrase activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following the extinction event of 66 million years ago, increasing body size allowed some mammal species to enlarge the hindgut, thereby providing a site for microbial breakdown of cellulose. This development was unlikely to have required modification of salivary electrolyte composition. Subsequently, body size permitting, some of these hindgut fermenters developed chambers anterior to the gastric stomach and concurrently had to modify the composition of saliva to control the pH in the more vigorous foregut fermentation. The parotid glands of foregut-fermenting eutherian herbivores, such as ruminants and camelids, produce a secretion which typically has higher concentrations of HCO3 and PO4 than parotid saliva from monogastric animals (Coats and Wright 1957; Bailey and Balch 1961; Hoppe et al. 1975; Ortiz et al. 1974). Kangaroos and wallabies (metatherian herbivores) also utilize foregut fermentation to digest their high-fibre diets and have independently evolved a parotid saliva having anion concentrations reminiscent of ruminants (Beal 1984, 1989). Arguably, saliva with this anion composition is a necessary adjunct to increased dependence on foregut fermentation and animals must either be pre-adapted or evolve such a salivary composition as they become more dependent on foregut fermentation. However, the ruminants and the macropods have not used identical cellular mechanisms to increase the [HCO3] of the parotid saliva in that sheep rely on increased transport of HCO3 from the blood by a basolateral Na–HCO3 co-transporter and kangaroos on increased acinar carbonic anhydrase activity (Beal 1991a, 1995; Steward et al 1996). In both species, parotid salivary Cl concentrations were very low and unresponsive to the administration of Na–K–2Cl co-transporter blockers (Wright et al. 1986; Beal 1995).
In addition to the large macropods, parotid salivary anion composition has been reported for five species of marsupials which are not reliant on foregut fermentation viz Rufous Bettong, Long-nosed Potoroo, Koala, Brush-tailed Possum and Common Wombat. The bettong and potoroo are closely related to the macropodid marsupials. Although the fossil record indicates the past existence of large species, the extant rat kangaroos are smaller than the smallest wallaby and regarded as more primitive than the macropods. Stomach anatomy of these potoroos is superficially similar to that of the kangaroos in that it consists of tubular and saccular regions anterior to the gastric region. However, the oesophagus enters the stomach close to the gastric region so that the tubiform region is very short and the saccular region, which constitutes up to 75% of the total stomach volume, appears to have a short-term food storage function (Hume 1982; Hume and Carlisle 1985). They have been classed as fungivore/omnivores (Lee and Cockburn 1985). The koala, possum and wombat have simple stomachs and enlarged caecum and/or proximal colon. Four of these animals (viz. bettong, potoroo, koala and possum) have parotid HCO3 concentrations that increase with rising salivary flow reaching concentrations at maximum flow approximately 25–30% higher than typical of monogastric species (Beal 1990, 1992; Scott and Beal 1994). Except at peak salivary flow rates in the possum, HCO3 concentrations exceed Cl concentrations in all four species. Parotid salivary PO4 concentrations of the bettong, potoroo and koala are similar to those of kangaroos. So, despite the differences in diet and gut function, the composition of the parotid saliva in these four species has some of the characteristics of saliva in the foregut fermenters.
Except for the males of the large kangaroo species, wombats are the largest living Australian marsupials. They are herbivores consuming a diet consisting preferentially of green grass but including bark, roots of shrubs and trees, and some species of fungi. The length of the wombat gut is approximately eight times that of kangaroos and consists of a simple stomach, a relatively-short small-intestine and a large colon contributing over 50% of the length (Dierenfeld 1984; Barbosa and Hume 1992). Thus, the colon is the only site for fermentation. In contrast to the above marsupials, HCO3 concentrations in the parotid saliva of the common wombat, rather than rising with increasing salivary flow, remain near constant at about 60 mmolar over the whole flow range (Beal 1991b). Thus, HCO3 secretion is increasing but at a rate that matches the increase in fluid secretion. Despite this, HCO3 concentrations exceed Cl concentrations at all but peak saliva flows. Consequently, saliva formation by the wombat parotid gland could be initiated by acinar Cl transport using the Na–K–2Cl co-transporter and/or the coupled antiports (Na/H and Cl/HCO3) as is common in mandibular salivary glands [review: Catalan et al. 2009] and/or acinar HCO3 secretion as in the kangaroo and sheep parotid glands followed by substantial ductal exchange of HCO3 for Cl.
This paper reports the results of administration of the Na–K–2Cl symport blocker, bumetanide; the Cl/HCO3 antiport blocker, SITS; the Na/H antiport blocker, amiloride; and the carbonic anhydrase inhibitor, acetazolamide; on secretion by the parotid gland of the common wombat. In addition, the effects on secretion of bumetanide combined with acetazolamide are also reported.
Materials and methods
Animals
Nine common wombats were used, five males (27.3 ± 1.50 kg) and four non-lactating females (27.4 ± 2.14 kg). Ipsilateral to the gland being studied, each animal had a permanent vinyl cannula (0.75 mm i.d., 1.45 mm o.d.; Dural Plastics, NSW) surgically implanted into the common carotid artery with the cannula exiting at the acnestis between the shoulder blades. The dead-space fluid volume in the cannulae ranged between 1.2 and 1.4 ml. The internal carotid artery was permanently ligated on the same side. Before closure of the neck incision, blood flow in the carotid artery was measured with a perivascular ultrasonic volume flow-sensor (Transonic Systems Inc., Ithaca, USA) during a 15 min intracarotid infusion of acetylcholine at rates sufficient to stimulate and maintain a stable salivary flow of approximately 1 ml min−1. These data were used when calculating the drug infusion rates for each wombat. The carotid cannula was flushed daily with heparinized saline (500 IU/ml) to maintain its patency The animals were fed with fresh grass and vegetables, bran, whole oats, lucerne chaff, kangaroo cubes and drinking water containing 25 mmol/1 NaC1 + 25 mmol/l NaHCO3.
Experimental procedures
Food was removed 15–16 h before each experiment with saline drinking solution being available until the experiment began. Anaesthesia was induced by intramuscular injection of ketamine (Ketamil; Troy Laboratories, Smithfield, Australia) at the rate of 17–28 mg kg−1. The animals were placed on an electrically heated pad for the duration of the experiment to maintain body temperature. A disposable Teflon cannula (Introcan, 22G; Braun, W. Germany) was introduced into the lesser saphenous vein of one hind leg. Thereafter, anaesthesia was maintained by intravenous injection of sodium pentobarbitone as a 5% aqueous solution. Hartmann's solution, modified by the addition of 1 ml of 1 mol l−1 MgCl2 and 40–50 ml of sterile water to each litre, was infused intravenously at 1.5–2.0 ml min−1 for the duration of the experiment to minimize changes in body fluid composition resulting from transpiration and salivary loss. The wombats were intubated with a cuffed endotracheal tube (7–8 mm), shortened to minimize dead-space, and thereafter ventilated with ambient air using a Campbell ventilator to maintain blood gases and blood pH within the normal range for conscious animals. The duct of the parotid gland ipsilateral to the cannulated carotid artery was catheterized using a vinyl tube (1.57 mm i.d., 2.08 mm o.d.; Dural Plastics, NSW) which was inserted not more than 3 cm through the duct orifice in the mouth. Saliva was collected in polypropylene sample tubes which were closed except for a small (20 wire gauge) air bleed. The distal end of the salivary catheter was positioned at 5–10 cm below the duct orifice. The dead-space volume in the parotid catheter was 0.4–0.5 ml. Salivary secretion was stimulated by intracarotid infusion of acetylcholine chloride (Sigma Chemical Co., St Louis, USA).
The level of acetylcholine infusion necessary to produce maximal flow was established and saliva sampled. Salivary flow was reduced to and maintained at approx. 1 ml min−1 (ie.30–40% maximum flow). After sampling for 25–35 min, physiological saline or glucose/saline (4%/0.18%) containing the blocking drug under test was infused into the carotid artery at rates sufficient to produce carotid plasma concentrations previously shown to be effective in other marsupials. The infusion rate was specific to each animal being based on a nominal plasma flow past the point of infusion calculated from the carotid blood flow obtained during intracarotid acetylcholine infusion on the day of carotid cannulation and the haematocrit on the day of experiment. Just before the end of the infusion of blocker, the acetylcholine infusion was increased to rates similar to those used initially to give maximal salivary secretion. Consequently, the impact of each blocking agent was assessed at two levels of cholinergic stimulation and saliva secretion; at mid-range secretion rates approximately 30–40% of maximum flow and at maximum stimulation/secretion rates. The blocking agents tested were acetazolamide (Lederle Laboratories, Australia), amiloride (Sigma Chemical Co., St Louis, USA), bumetanide (Astra Pharmaceuticals P/L, North Ryde, Australia) and SITS (Sigma). Each animal also underwent one experiment in which the protocol was repeated without the blocking agents in the infusate to provide control data that could be used to distinguish any changes in plasma and salivary variables associated with the general protocol from those caused by the blocking agent.
In a second series of experiments, five wombats underwent an experiment in which they were given intracarotid infusions of acetazolamide superimposed on bumetanide blockade. Preparation of the animals and stimulation of salivary flow with acetylcholine to achieve a maintained flow of approximately 1 ml min−1 before blocker administration were as described above. Bumetamide was infused for 60 min with acetazolamide infusion being added after 30 min.
Recovery
At the finish of each experiment, the leg cannula and salivary catheters were removed and a single intramuscular injection (1 ml 10 kg−1) of procaine and benzathine penicillin (Benacillin; Troy Laboratories P/L, NSW) was given while the wombats were anaesthetized. The endotracheal tube was removed when the swallowing reflex had returned and the animals were monitored over the following 15–30 min to ensure that respiration was unimpaired.
Analytical procedures
Blood samples were centrifuged at 2200g for 10 min to obtain plasma for analysis. Microhaematocrit determinations were made in triplicate on blood spun at 12,500g for 10 min in a microhaematocrit centrifuge (Heraeus-Christ, Osterode, Germany). Blood plasma and saliva were analysed in duplicate for Na, K, CI, HCO3, PO4, H+ and osmolality. Glandular secretion rates for these ions were calculated as the product of the ion concentration and the concomitant salivary flow rate. Na and K were measured by atomic absorption spectroscopy using appropriate ionization suppressants. Estimations were made using a Radiometer chloride titrator (model CMT 10) for Cl; using thermostated Radiometer microelectrodes for pH, pCO2 and pO2; using the method of Baginski et al. (1967) for total inorganic PO4; and using an Advanced freezing-point osmometer for osmolality. Bicarbonate concentration was determined by the titration procedure of Gyory and Edwards (1967) modified for 0.2 ml portions of sample. Estimates of the upper limit of salivary amiloride and SITS were made using the absorption peaks characteristic of amiloride (288 and 362 nm) and SITS (340 nm).
Statistical procedures
Comparisons between experiments with transport-blocking agents and control experiments having a similar protocol were done by analysis of covariance, the covariate used being the initial stable-flow value (1 ml min−1) for each variable being analysed. If the variance ratio was significant, Tukey’s w procedure was applied to find individual differences between corresponding means (Steel and Torrie 1960). Salivary and plasma electrolyte concentrations within experiments were compared by Student’s t test for uncorrelated means or the paired t test.
Results
Blocker-free control infusion
The concentrations of ions in the plasma and the haematocrit were unaltered by this treatment. Plasma osmolality increased over the period of salivary collection from 289.1 ± 0.43 to 290.7 ± 0.81 mmol kg−1 (paired t = 2.99; P = 0.020). The rates of acetylcholine infusion needed to maintain constant salivary flow at the mid-range rate of 1 ml min−1 were unaltered over the 75 min of salivary collection and there were no significant changes in salivary composition under stable cholinergic stimulation.
Bumetanide infusion
Plasma and cardiovascular parameters
The concentrations of plasma electrolytes, plasma osmolality and haematocrit did not change significantly during this treatment. Mean haematocrit was 29.9 ± 2.89% and the estimated carotid plasma flow for individual wombats ranged between 6.6 and 8.4 ml kg−1 min−1.
Fluid
A range of concentrations of bumetanide (0.005, 0.05 and 0.1 mmol l−1) in carotid artery plasma was established stepwise over 50 min. At 0.005 mmol l−1, bumetanide administration was associated with a fall in salivary flow (Fig. 1) from a steady-state flow of approx. 1 ml min−1 (1.04 ± 0.013 ml min−1) to 0.70 ± 0.046 ml min−1 (67 ± 10.8% of the pre-treatment flow; P = 0.0002). Increasing the bumetanide concentration to 0.05 mmol l−1 reduced flow to 0.53 ± 0.030 ml min−1 (51 ± 2.6% of initial flow) and at 0.1 mmol l−1 to 0.50 ± 0.039 ml min−1 (48 ± 3.4% of initial flow; P < 0.0001). A higher carotid concentration of bumetanide (0.3 mmol l−1) in two animals did not suppress flow further.
Effect of bumetanide (0.005, 0.05 and 0.1 mmol l−1 carotid plasma) on parotid salivary flow rate, chloride concentration and chloride secretion rate during acetylcholine (Ach) stimulation. Pretreatment reference values for maximum and mid-range (30–40% maximum) salivary flow rates are shown in the left panels (unshaded) (means ± SEM; n = 6)
At bumetanide concentrations of 0.1 mmol l−1, high rates of acetylcholine infusion which had been shown in the initial reference samples to be sufficient to stimulate salivary flows averaging greater than 3 ml min−1, elicited a maximum flow of 0.98 ± 0.100 ml min−1 or 31 ± 1.1% of the flow rate for the same level of stimulation prior to bumetanide administration (paired t = 9.979; P = 0.0002; Fig. 1).
Anions
Correlated with the falling salivary flow rates, salivary [Cl] decreased progressively with increasing bumetanide levels (Fig. 1) whereas salivary [HCO3] increased (Fig. 2) and [PO4] was not altered significantly (Table 1). At 0.005 mmol l−1 bumetanide, salivary [Cl] fell from the pre-treatment value of 70.2 ± 9.53 mmol l−1 to 45.3 ± 5.91 mmol l−1 (P < 0.0001) and [HCO3] rose from 49.0 ± 2.94 to 79.7 ± 5.40 mmol l−1 (P = 0.0004). At the maximum bumetanide concentration, salivary [Cl] had fallen to 23.1 ± 4.00 mmol l−1 (P < 0.0001) and [HCO3] had risen to 110.2 ± 3.96 mmol l−1 (P < 0.0001). Concurrently, Cl secretion rate fell from 72.6 ± 9.28 to 11.3 ± 1.80 µmol min−1 (P < 0.0001; Fig. 1) whereas HCO3 secretion was unaltered (51.1 ± 3.52 to 55.6 ± 5.86 µmol min−1; Fig. 2).
Effect of bumetanide (0.005, 0.05 and 0.1 mmol l−1 carotid plasma) on parotid salivary bicarbonate concentration and on salivary secretion rates of sodium, potassium and bicarbonate during acetylcholine (Ach) stimulation. Pretreatment reference values for maximum and mid-range (30–40% maximum) salivary flow rates are shown in the left panels (unshaded) (means ± SEM; n = 6)
High-rate acetylcholine stimulation during bumetanide administration was associated with further elevation of salivary [HCO3] (P = 0.0033) and HCO3 secretion (P = 0.0056; Fig. 2) but did not cause any additional change in [Cl] (Fig. 1) or [PO4]. As Cl secretion averaged 236 ± 26.9 µmol min−1 in the initial reference sample during high-level acetylcholine stimulation, the bumetanide treatment blocked glandular Cl secretion to about 7% of the initial maximum secretion rate. Concurrently, the average falls in HCO3 and PO4 secretion were 26% and 79%, respectively.
Cations and osmolality
During bumetanide infusion, salivary [Na] rose progressively from 102.7 ± 8.67 to 113.7 ± 5.51 mmol l−1 (P = 0.021) with the [Na] being increased further during high-rate cholinergic stimulation. Salivary [H+] decreased from 19.1 ± 2.17 to 7.1 ± 0.66 ηmol l−1 (P = 0.0004; Table 1). Neither low-rate nor high-rate cholinergic stimulation were associated with any consistent/significant changes in salivary [K] or osmolality (Table 1). Concurrently, the secretion rates of Na and K (Fig. 2) fell during acetylcholine infusion at both mid-range level (P < 0.0001 and 0.017, respectively) and high level (P < 0.0001 and 0.0001, respectively).
SITS infusion
Plasma and cardiovascular parameters
The concentrations of plasma electrolytes and the haematocrit did not change significantly during this treatment. Plasma osmolality rose from 289.9 ± 0.55 to 291.8 ± 0.85 mmol kg−1 (paired t = 5.960; P = 0.009) but covariance analysis showed that these effects were quantitatively similar to those occurring over the course of the blocker-free control experiment. Mean haematocrit was 29.7 ± 4.12% and the estimated carotid plasma flow for individual wombats ranged between 7.1 and 8.1 ml kg−1 min−1.
Fluid
Concentrations of SITS (0.075 and 0.75 mmol l−1) in carotid artery plasma were established in two steps over 47 min. Under mid-range acetylcholine stimulation, SITS administration at 0.075 mmol l−1for 15 min had no effect on salivary flow. Increasing SITS to the higher level of 0.75 mmol l−1 was rapidly followed by increased salivary flow (Fig. 3) which was significant relative to pre-treatment samples (paired t = 18.79; P = 0.0003) and to corresponding samples of the control experiment (P < 0.0001). Having peaked during the initial 5 min of this treatment, flow fell progressively over the following 15 min to levels not statistically different to pre-treatment control rates. High-rate cholinergic stimulation during high-rate SITS administration was as effective at augmenting salivary flow as similar levels of cholinergic stimulation prior to SITS treatment (Fig. 3).
Effect of SITS (0.075 and 0.75 mmol l−1 carotid plasma) on parotid salivary flow rate and on concentrations of chloride, bicarbonate, sodium and potassium in the parotid saliva during acetylcholine (Ach) stimulation. Pretreatment reference values for maximum and mid-range (30–40% maximum) salivary flow rates are shown in the left panels (unshaded) (means ± SEM; n = 4). Apparent absence of error bars indicates the error value was relatively small
Electrolytes
SITS administration at the lower rate (0.075 mmol l−1) had no effect on the concentrations of major electrolytes in the saliva. The higher rate of SITS infusion caused no significant changes in salivary electrolyte concentrations (Fig. 3; Table 2). Likewise, ion concentrations in saliva evoked during SITS administration by high-rate cholinergic stimulation were similar to those in the pre-treatment maximum-flow saliva.
Amiloride infusion
Plasma and cardiovascular parameters
The concentrations of plasma electrolytes, osmolality and haematocrit did not change significantly during this treatment. Mean haematocrit was 33.1 ± 3.39% and the estimated carotid plasma flow for individual wombats ranged between 6.8 and 8.1 ml kg−1 min−1.
Fluid
A range of amiloride concentrations (0.05, 0.25 and 0.5 mmol l−1) was established stepwise in carotid artery plasma over 44 min (Fig. 4). Immediately following the onset of amiloride infusion, saliva secretion rate fell by 20–30% from 1.04 ± 0.010 to 0.79 ± 0.030 ml min−1. Thereafter, salivary flow increased progressively to 1.28 ± 0.025 ml min−1 (P = 0.0002) despite the rate of cholinergic stimulation being unaltered throughout and the rate of amiloride infusion rising tenfold. However, maximum salivary flow during amiloride infusion (1.63 ± 0.050 ml min−1) was significantly lower than the maximum flow (2.96 ± 0.098 ml min−1; P < 0.0001) prior to amiloride administration.
Effect of amiloride (0.05, 0.25 and 0.5 mmol l−1 carotid plasma) on parotid salivary flow rate, on sodium, potassium, chloride and bicarbonate concentrations and on bicarbonate secretion rate in the parotid saliva during acetylcholine (Ach) stimulation. Pretreatment reference values for maximum and mid-range (30–40% maximum) salivary flow rates are shown in the left panels (unshaded) (means ± SEM; n = 4). Apparent absence of error bars indicates the error value was relatively small
Electrolytes
At the mid-range flow of 1.0 ml min−1, amiloride infusion was associated with progressive increases in salivary Na, Cl, H+ and PO4 concentrations and osmolality and decreases in K and HCO3 concentrations (Fig. 4; Table 3). At the final amiloride concentration of 0.5 mmol l−1, salivary [Na] had risen from the pre-treatment concentration of 101.0 ± 8.24 to 134.8 ± 4.67 mmol l−1 (P = 0.0001), [H+] 17.2 ± 0.24 to 20.0 ± 0.88 ηmol l−1 (P = 0.025), [Cl] from 68.0 ± 7.10 to 100.8 ± 4.31 mmol l−1 (P = 0.0002), [PO4] from 0.36 ± 0.021 to 0.65 ± 0.043 mmol l−1 (P = 0.009), and osmolality from 224.3 ± 13.50 to 279.7 ± 4.55 mosmol kg−1 (P = 0.0003) (Fig. 4;Table 3). Concurrently, [K] fell from 17.6 ± 1.49 to 9.1 ± 0.15 mmol l−1 (P < 0.0001) and [HCO3] from 51.1 ± 0.89 to 44.2 ± 1.01 mmol l−1 (P = 0.0025). A similar pattern of electrolyte concentration occurred at maximum salivary flow during amiloride infusion with [Na], [Cl], [PO4] and osmolality being significantly higher (paired t = 5.487, 6.029, 21.424 and 4.673; P = 0.012, 0.009, 0.0002 and 0.019, respectively) and [K] and HCO3] being lower (paired t = 4.921 and 3.606; P = 0.016 and 0.037) than for maximum flow prior to amiloride administration (Fig. 4; Table 3).
Acetazolamide infusion
Plasma and cardiovascular parameters
None of the small changes in plasma electrolyte concentrations were statistically significantly whereas plasma osmolality increased from 288.0 ± 1.90 to 291.3 ± 1.20 mosmol kg−1 (P = 0.025). Mean haematocrit was 28.0 ± 2.87% and the estimated carotid plasma flow for individual wombats ranged between 6.8 and 8.7 ml kg−1 min−1.
Fluid
A range of concentrations of acetazolamide (0.35, 1.0 and 2.5 mmol l−1) in carotid artery plasma was established stepwise over 44 min (Fig. 5). Neither the salivary flow nor the rate of acetylcholine infusion necessary to maintain flow at the nominal 1.0 ml min−1 was altered by the presence of acetazolamide at any of the above concentrations. At the highest plasma concentration of acetazolamide, high rates of acetylcholine infusion stimulated a maximum salivary flow rate of 2.59 ± 0.292 ml min−1 which was similar to the initial flow rate (2.64 ± 0.369 ml min−1) prior to acetazolamide administration.
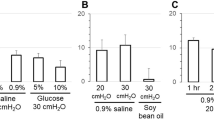
Effect of acetazolamide (0.35, 1.0 and 2.0 mmol l−1 carotid plasma) on parotid salivary flow rate and on chloride, bicarbonate, sodium and potassium concentrations in the parotid saliva during acetylcholine (Ach) stimulation. Pretreatment reference values for maximum and mid-range (30–40% maximum) salivary flow rates are shown in the left panels (unshaded) (means ± SEM; n = 6)
Anions
Correlated with the increasing rates of acetazolamide infusion, salivary [Cl] increased, salivary [HCO3] decreased (Fig. 5) and [PO4] was not altered significantly (Table 4). At 0.35 mmol l−1 acetazolamide, salivary [Cl] rose from the pre-treatment value of 67.1 ± 5.54 mmol l−1 to 82.9 ± 4.27 mmol l−1 (P < 0.0001) and [HCO3] fell from 52.0 ± 1.23 to 33.5 ± 1.42 mmol l−1 (P < 0.0001). At the highest acetazolamide concentration, salivary [Cl] had risen to 91.4 ± 4.76 mmol l−1 (P = 0.0002), and [HCO3] had fallen to 31.6 ± 0.99 mmol l−1 (P < 0.0001). The resulting HCO3 excretion rate was 61 ± 2.2% of the excretion rate under the initial control conditions.
At maximal cholinergic stimulation, the levels of [Cl] and Cl secretion were higher (P = 0.0001 and 0.0014, respectively) and the levels of [HCO3] and HCO3 secretion were lower (P < 0.0001 and P = 0.0033, respectively) during acetazolamide infusion than during the high flow controls. The HCO3 excretion rate was 50 ± 1.6% of the rate obtained prior to acetazolamide infusion.
Cations and osmolality
At the beginning of acetazolamide infusion, salivary [Na] and Na secretion fell (7 ± 1.2 and 9 ± 1.8%; P = 0.005 and 0.006, respectively) but thereafter rose progressively returning to control values over the next 15 min (Fig. 5). Concurrently, salivary [H+] and H+ secretion increased (P = 0.0002), whereas [K] and osmolality and their secretion rates were unaltered by acetazolamide administration during low-level cholinergic stimulation (Fig. 5; Table 4). Under maximal stimulation, [K] and K secretions during acetazolamide blockade were lower and [H+] and H+ secretions were higher than during maximal stimulation in the absence of the blocker (P < 0.0001, P = 0.014, P = 0.003 and 0.007, respectively).
Simultaneous bumetanide and acetazolamide infusion
Plasma and cardiovascular parameters
With the exception of osmolality, the concentrations of plasma electrolytes and the haematocrit did not change significantly during this treatment. Plasma osmolality rose from 291.3 ± 2.57 to 293.9 ± 3.02 mosmol kg−1 (P = 0.014). Mean haematocrit was 27.7 ± 1.54% and the estimated carotid plasma flow for individual wombats ranged between 7.0 and 8.0 ml kg−1 min−1.
Fluid
Bumetanide concentrations of 0.005 and 0.1 mmol l−1 in carotid artery plasma were established stepwise over 30 min. Thereafter, acetazolamide and bumetanide were infused concurrently for a further 30 min (Fig. 6). Bumetanide infusion reduced salivary flow from a steady-state flow of approx. 1 ml min−1 (1.03 ± 0.007 ml min−1) to 0.52 ± 0.029 ml min−1 (50 ± 2.8% of the pre-treatment flow; paired t = 17.615; P < 0.0001). Adding acetazolamide to the infusate to establish a carotid artery plasma concentration of 1.5 mmol l−1 reduced saliva secretion by a further 23% to 0.28 ± 0.022 ml min−1 (to 27 ± 2.1% of the steady-state flow; paired t = 6.597; P < 0.0001). Under maximum flow conditions, the combination of acetazolamide with bumetanide reduced flow by 86% from 3.1 ± 0.42 to 0.42 ± 0.05 ml min−1 (paired t = 7.292; P = 0.002).
Effect of simultaneous administration of bumetanide (0.1 mmol l−1 carotid plasma) and acetazolamide (CAI; 1.5 mmol l−1 carotid plasma) on parotid salivary flow rate, on chloride and bicarbonate concentrations and on chloride and bicarbonate secretion rates in the parotid saliva during acetylcholine (Ach) stimulation. Pretreatment reference values for maximum and mid-range (30–40% maximum) salivary flow rates are shown in the left panels (unshaded) (means ± SEM; n = 5). Apparent absence of error bars indicates the error value was relatively small
Anions
Bumetanide at 0.1 mmol l−1 reduced salivary [Cl] and Cl secretion to 17.1 ± 1.74 mmol l−1 and 8.7 ± 0.72 µmol min−1, respectively (Fig. 6). Bicarbonate concentration increased to 116.0 ± 2.28 mmol l−1 whereas HCO3 secretion remained stable and not significantly different from the control values. Phosphate concentration increased (P = 0.009; Table 5) and secretion fell (P = 0.014). Adding acetazolamide to the infusate was associated with a further reduction in Cl secretion, but not [Cl], to a plateau level of 4.35 ± 0.681 µmol min−1 (paired t = 6.12; P = 0.004). Concurrently, [HCO3] fell progressively over the period of CAI administration to 91.6 ± 4.31 mmol l−1 (paired t = 5.81; P = 0.004) whereas HCO3 secretion fell initially (paired t = 7.21; P = 0.002) to plateau for the remainder of the acetazolamide infusion.
Under conditions of maximum stimulation/secretion, the presence of the two transport blockers reduced [Cl] from 56.3 ± 5.83 to 13.1 ± 2.06 mmol l−1 and Cl secretion from 175 ± 28.3 to 5.7 ± 1.34 µmol min−1. Concurrently, [HCO3] rose from 57 ± 3.4 to 108 ± 5.7 mmol l−1 and HCO3 secretion fell from 172 ± 16.1 to 45 ± 5.4 µmol min−1. Phosphate concentrations were unaltered (Table 5) whereas PO4 secretion was lower (P = 0.018).
Cations and osmolality
During the initial bumetanide infusion, salivary [Na] rose progressively from 90.1 ± 4.86 to 111.5 ± 3.40 mmol l−1 (P = 0.003) and salivary osmolality increased from 208 ± 10.2 to 261 ± 4.6 mosmol kg−1 whereas salivary [H+] fell (Table 5) and changes in salivary [K] were inconsistent (either rising or falling). Concurrently, the Na, K, H+ and osmolal secretion rates fell (93.3 ± 5.21 to 57.6 ± 4.15; 20.7 ± 0.53 to 14.2 ± 1.82 µmol min−1; 18 5 ± 1.21 to 3.9 ± 0.27 pmol min−1 and 216 ± 10.9 to 134 ± 5.7 µosmol min−1: P = 0.0007; 0.012; 0.0003 and 0.0005, respectively). Adding acetazolamide in the infusate caused a progressive reduction in [Na] (111 to 70 ± 8.8 mmol l−1; P = 0.008) and Na secretion (58 to 21.2 ± 3.07 µmol min−1; P = 0.0005). Concurrently, salivary osmolality fell from 261 to 217 ± 7.7 mosmol kg−1 (P = 0.0001) and osmolal secretion was stable at 64.5 ± 5.58 µosmol min−1.
At maximal flow stimulation, simultaneous infusion of bumetanide and acetazolamide decreased [Na] (101 ± 4.6 to 77 ± 6.7 mmol l−1; P = 0.008) and Na secretion (304 ± 33.7 to 34 ± 6.3 µmol min−1; P = 0.0006). Salivary [H+] decreased (P < 0.0001) and secretion rate fell from 57.8 ± 8.71 to 3.3 ± 0.31 pmol min−1 (P = 0.002). Concomitantly, salivary [K] increased (18.0 ± 0.47 to 48.4 ± 10.6 mmol l−1; P = 0.02) with K secretion decreasing (56 ± 8.6 to 19 ± 3.9 µmol min−1; P = 0.004). Osmolal secretion fell from 680 ± 78.8 to 100 ± 12.2 µosmol min−1; P < 0.0001).
Concentrations of SITS and amiloride in saliva
During high-level SITS infusion, the concentration of SITS in the final steady-state saliva was 47 ± 1.4 µmol l−1 falling to 19 ± 0.60 µmol l−1 in the maximum flow sample. The amiloride concentration in final steady-state saliva was 35 ± 0.8 µmol l−1 and during maximum flow was 28 ± 0.6 µmol l−1.
Discussion
The effects of membrane transport blockers on parotid secretion were assessed during steady-state mid-range salivary flow (approximately 30% maximum rate) and during maximum flow stimulated by intracarotid acetylcholine infusion.
Effect of bumetamide
Blockade of salivary secretion by serosal administration of loop diuretics is considered to be evidence for the involvement of a basolaterally located Na–K–2Cl symport (NKCC transporter) in primary fluid secretion. Intracarotid bumetanide infusion in the wombats was associated with falls in salivary flow of 50% during exposure to plasma bumetanide concentrations of 0.05 and 0.1 mmol l−1 under steady-state mid-range flow conditions. At maximal acetylcholine stimulation, bumetanide administration reduced glandular output of fluid and Cl by approximately 68% and 93%, respectively (Fig. 1). Thus, if bumetanide blocks the Na–K–2Cl transporter specifically, the data for bumetanide indicate that about two-third of fluid secretion by the wombat parotid gland was supported by the electroneutral triple symport. This degree of blockade is substantially less than that found for red kangaroo mandibular glands at similar bumetanide concentrations (Beal 1997) but is similar to that reported for mandibular glands of various eutherian species (60–75%) under similar electrolyte perfusion regimes (Poulsen et al. 1982; Martinez and Cassity 1983; Novak and Young 1986; Pirani et al. 1987; Lau et al. 1990). The incomplete blockade of parotid fluid secretion during bumetanide treatment in wombats would occur if the bumetanide level was insufficient or if secretion was partially supported by other ion transport mechanisms. The similar levels of blockade at 0.05 and 0.1 mmol l−1 (and 0.3 mmol l−1; data not presented) in the wombats are an indication that the bumetanide levels were sufficient to achieve near-complete blockade of the Na–K–2Cl transporter as does the near-total blockade of Cl secretion. Three additional mechanisms have been proposed to explain the inability of loop diuretics to abolish salivary fluid secretion totally; functional coupling of Na/H and Cl/HCO3 exchangers in the acinar basolateral membrane resulting in Cl transport (Martinez and Cassity 1985; Novak and Young 1986) or acinar formation and secretion of HCO3 involving carbonic anhydrase (Lau et al. 1990; Beal 1991a) or basolateral transport of plasma HCO3 (Steward et al. 1996). Based on data for the rabbit mandibular gland, Lau et al (1990) have postulated that the Na–K–2Cl symport is maximally inhibited by bumetanide concentrations of 0.01 mmol l−1 and greater inhibition of fluid output obtained at bumetanide levels of 0.1 mmol l−1 was due to blockade of acinar HCO3 synthesis. In the wombats, the output of HCO3 by the parotid gland did not change during mid-range cholinergic stimulation regardless of whether the bumetamide blockade was present or not (Fig. 2).
Maximum salivary flow rates during bumetanide blockade averaged 31% of the maximum flow rates obtained prior to bumetanide administration. During the transition from mid-range to maximal cholinergic stimulation, salivary [Cl] fell (Fig. 1) whereas the concurrent increases in salivary [HCO3] (Fig. 2) and saliva flow would be consistent with increased acinar HCO3 synthesis/secretion driving the rise in saliva outflow. However, with the [HCO3] having risen to 124 ± 2.5 mmol l−1 under the current conditions, the gland has no scope to raise HCO3 secretion and consequently saliva production further.
Effect of SITS
Administration of SITS at levels that should inhibit the Cl/HCO3 exchangers and the Na HCO3 co-transporter augmented, rather than depressed, parotid fluid output in wombats during mid-range acetylcholine stimulation (Fig. 3). With the exception of the sheep parotid, stilbene derivatives (SITS and DIDS) stimulate salivary flow from rat, rabbit and kangaroo mandibular glands and kangaroo parotid glands (Martinez and Cassity 1985; Novak and Young 1986; Wright et al. 1986; Pirani et al. 1987; Lau et al. 1990; Beal 1995, 1997). However, the ion-transport mechanisms used by these glands to initiate acinar fluid secretion are fundamentally different; the sheep and kangaroo parotids being dependent on different mechanisms of HCO3 secretion whereas the mandibular glands depend predominantly on Cl secretion. Thus, the stilbene derivatives probably enhance fluid secretion by acting at the signal transduction level rather than by direct action on some component of ion transport. This would be consistent with the observation that DIDS elicited mandibular secretion in the rabbit in the absence of acetylcholine stimulation (Lau et al. 1990). In wombats, the increased salivary flow that accompanied the high-level SITS infusion peaked during the initial 5 min collection and thereafter declined progressively toward pre-SITS control flows during the subsequent 15 min of low-level stimulation. Similar patterns of waning saliva flow increase occurred during DIDS administration in isolated rat and rabbit mandibular glands (Martinez and Cassity 1985; Lau et al. 1990). Depending on the animal species and salivary gland, changes in salivary [HCO3], [Cl], [Na] or [K] during stilbene administration have been inconsistent with each ion increasing or decreasing or unaltered in concentration (Martinez and Cassity 1985; Novak and Young 1986; Wright et al. 1986; Pirani et al. 1987; Lau et al. 1990; Beal 1995, 1997). SITS administration in the wombat did not alter the concentrations of any of the major ions in the parotid saliva (Fig. 3; Table 2).
Under conditions of maximal acetylcholine stimulation and saliva flow, SITS administration did not reduce saliva secretion rate nor alter the concentrations of the major ions in the wombat parotid saliva. The stilbene sensitive transporters did not appear to contribute significantly to the production of saliva in the wombat parotid gland. However, there are Cl/HCO3 exchanger isoforms that are resistant to stilbene blockade (Tsuganezewa et al. 2001).
Effect of amiloride
Amiloride administration into wombats caused substantial increases in parotid salivary [Na] and [Cl] and a 50% fall in [K] during both mid-range stable flow and maximum flow stimulation (Fig. 4). These responses differ from those found for the kangaroo parotid and mandibular glands (Beal 1995, 1997) but are broadly similar to those reported for rat and rabbit mandibular glands (Martinez and Cassity 1985; Lau et al. 1990) and are consistent with the expected effects of blockade of the basolateral Na/H antiports in the acini and ducts and the luminal Na channels in the duct system. Under stable mid-range conditions and acetylcholine stimulation, saliva flow fell by 20–30% immediately following the onset of amiloride infusion at the lowest concentration (0.05 mmol l−1 carotid plasma) but rose progressively thereafter to levels significantly above the control despite the tenfold increase in amiloride level. The initial reduction in saliva output relative to control conditions coincides with reductions in luminal K and HCO3 secretion (54 and 28%, respectively) which would be an expected consequence of rising acinar cell [H+] resulting from blockade of the basolateral Na/H antiport. Additionally, amiloride competes with acetylcholine for access to muscarinic receptors (Kuipers et al. 1984; Martinez et al. 1989; Dehaye and Verhasselt 1995) providing another possible contributor to this reduction in flow rate.
The subsequent rise in flow during mid-range stimulation resulted from the reduction in osmotic gradient between saliva and extracellular fluid (Fig. 4; Table 3). Amiloride infusion was accompanied by a rapid increase in mean salivary osmolality, rising from 80% of the plasma osmolality to 91% at 10 min of treatment and 97% by the end of infusion; hence, the gradient for water reabsorption was progressively eliminated. This increase in salivary osmolality was arguably caused by increasing blockade of the Na channel (ENaC) in the luminal membrane of the duct cells resulting in substantial increases in salivary [Na] with Cl as the accompanying anion. During amiloride blockade, water excretion in the saliva increased by 62 ± 7.4% between the first and last period of stable mid-range cholinergic stimulation (Fig. 4). In the absence of amiloride blockade, this volume of water would have been reabsorbed paracellularly thereby preventing the accumulation of hypertonic fluid in the paracellular spaces. It indicates the amount of volume change that would normally occur in the ducts between acinar input and final salivary output at a secretion rate approximating 25% of maximum.
Effect of acetazolamide
Given by themselves, carbonic anhydrase inhibitors have little effect on fluid output by salivary glands other than the kangaroo parotid (Chauncey and Weiss 1958; Yoshimura et al. 1959; Bruzilow and Diaz 1962; Young et al. 1970; Somner et al. 1975; Blair-West et al. 1980; Case et al. 1980, 1982; Pirani et al. 1987; Beal 1991a). Fluid output by wombat parotid glands is also unaltered by acetazolamide concentrations (Fig. 5) which were five times the concentration that substantially blocked (90%) parotid flow in kangaroos (Beal 1991a). In the absence of flow changes during either of the two cholinergic stimulation regimes, the concomitant increases in [Cl] and Cl excretion and decreases in [HCO3] and HCO3 excretion were consistent with reduced Cl/ HCO3 exchange, possibly in the ducts, as a consequence of partial reduction in HCO3 for exchange. The residual salivary HCO3 excretion remained at 50% or more of that prior to acetazolamide administration indicating that either the blockade of carbonic anhydrase activity was far from complete or the secretory cells had access to another source of HCO3. Given that a plasma acetazolamide concentration of 0.5 mmol l−1 reduced HCO3 excretion by the kangaroo parotid gland by over 90% (Beal 1991a), the blockade of carbonic anhydrase activity in the wombats should have been nearly complete. Thus, basolateral transport of HCO3 from the plasma becomes the probable source. If acinar HCO3 synthesis involving carbonic anhydrase supports any fluid secretion, sensitivity to carbonic anhydrase inhibition should be accentuated by simultaneous blockade of acinar Cl transport with bumetanide as occurs in the isolated rat mandibular gland (Pirani et al. 1987).
In wombats receiving stable mid-range stimulation, the addition of acetazolamide to an established bumetanide infusion reduced parotid fluid secretion by a further 22% (and maximum flow by an additional 18%) relative to bumetanide alone (Fig. 6). The lowered fluid secretion rates are consistent with acetazolamide reducing the acinar production of HCO3. With the synthesis of HCO3 being substantially blocked, the high but progressively falling salivary [HCO3] during the 20 min period of sampling would result from the progressive washout of HCO3 that had accumulated in the gland cells during the previous bumetanide treatment by a relatively low fluid secretion and flow. During maximum stimulation, salivary flow and [HCO3] increased indicating that the higher acetylcholine levels stimulated HCO3 secretion presumably by a basolateral HCO3 transporter.
Comparison of marsupial secretion mechanisms
During maximum acetylcholine-stimulated salivary flow, the acinar NKCC co-transporter supported 69% of secretion by the parotid gland of wombats whereas, in the red kangaroo, the co-transporter supported 88% by the mandibular gland and zero by the parotid gland. Glandular HCO3 synthesis by carbonic anhydrase supports 89% of parotid secretion in kangaroos, 18% of parotid secretion in wombats and zero by kangaroo mandibular gland. In all three glands, the secretion of Cl and HCO3 by the above mechanisms accounts for over 85% of maximal saliva secretion. For the kangaroo parotid gland, much of the remaining deficit would be filled by PO4 secretion. In the wombat parotid and kangaroo mandibular salivas, PO4 constitutes approximately 0.6% and 0.15%, respectively, of the secreted inorganic anions, so the deficit is presumably filled by HCO3 derived from basolateral HCO3 transport and/or the coordinated activities of the basolateral Na/H and Cl/HCO3 exchangers (Beal 1991a, 1995, 1997). The presence of the basolateral Na/H exchanger in the kangaroo parotid gland acini, is essential for sustaining HCO3 production whereas it would be counterproductive for the acini to have a Cl/HCO3 exchanger in the basolateral membrane.
Abbreviations
- CAI:
-
Carbonic anhydrase inhibitor
- SITS:
-
4-Acetamido-4′-isothiocyanatostilbene-2,2′disulphonic acid
- DIDS:
-
4,4′-Diisothiocyanatostilbene-2-2′disulphonic acid
References
Baginski ES, Foa PP, Zak B (1967) Microdetermination of inorganic phosphate, phospholipids and total phosphate in biological materials. Clin Chem 13:326–332
Bailey CB, Balch CC (1961) Salivary secretion and its relation to feeding in cattle. Br J Nutr 15:383–403
Barbosa ES, Hume ID (1992) Digestive tract morphology and digestion in the wombats (Marsupialia: Vombatidae). J Comp Physiol B 162:552–560
Beal AM (1984) Electrolyte composition of parotid saliva from sodium-replete kangaroos. J Exp Biol 111:225–237
Beal AM (1989) Differences in salivary flow and composition among kangaroo species: implications for digestive efficiency. In: Grigg G, Jarman P, Hume I (eds) Kangaroos, wallabies and rat kangaroos. Surry Beatty and Sons, Sydney, pp 189–195
Beal AM (1990) Secretion rates and composition of parotid saliva in the koala (Phascolarctos cinereus). J Zool Lond 221:261–274
Beal AM (1991a) The effect of carbonic anhydrase inhibitors on secretion by the parotid and mandibular glands of red kangaroos Macropus rufus. J Comp Physiol B 161:611–619
Beal AM (1991b) Characteristics of parotid saliva from the common wombat (Vombatus ursinus). J Zool Lond 224:403–417
Beal AM (1992) Relationships between plasma composition and parotid salivary composition and secretion rates in the potoroine marsupials, Aepyprymnus rufescens and Potorous tridactylus. J Comp Physiol B 162:637–645
Beal AM (1995) Mechanisms of fluid and ion secretion by the parotid gland of the kangaroo, Macropus rufus, assessed by administration of transport-inhibiting drugs. J Comp Physiol B 165:396–405
Beal AM (1997) The effect of transport-blocking drugs on secretion of fluid and electrolytes by the mandibular gland of red kangaroos, Macropus rufus. Arch Oral Biol 42:705–716
Blair-West JR, Fernley RT, Nelson JF, Wintour EM, Wright RD (1980) The effect of carbonic anhydrase inhibitors on the anionic composition of sheep’s parotid saliva. J Physiol (Lond) 299:29–44
Bruzilow SW, Diaz CL (1962) Effect of acetazolamide on dog parotid saliva. Am J Physiol 202:158–160
Case RM, Conigrave AD, Novak I, Young JA (1980) Electrolyte and protein secretion by the perfused rabbit mandibular gland stimulated with acetylcholine or catecholamines. J Physiol (Lond) 300:467–487
Case RM, Conigrave AD, Favaloro EJ, Novak I, Thompson CH, Young JA (1982) The role of buffer anions and protons in secretion by the rabbit mandibular gland. J Physiol (Lond) 322:273–286
Catalan MA, Nakamoto T, Melvin JE (2009) The salivary gland fluid secretion mechanism. J Med Investig 56(Suppl):192–196
Chauncey HH, Weiss PA (1958) Composition of human saliva. Parotid gland secretion: flow rate, pH and inorganic composition after oral administration of a carbonic anhydrase inhibitor. Arch Int Pharmacodyn Ther 113:377–383
Coats DA, Wright RD (1957) Secretion by the parotid gland of the sheep: the relationship between salivary flow and composition. J Physiol 135:611–622
Dehaye JP, Verhasselt V (1995) Interaction of amiloride with rat parotid muscarinic and alpha-adrenergic receptors. Gen Pharmacol 26:155–159
Dierenfeld ES (1984) Diet quality of sympatric wombats, kangaroos and rabbits during severe drought. Ph.D. thesis, Cornell University, Ithaca, NY, USA
Gyory AZ, Edwards KDG (1967) Simultaneous titrimetric determination of bicarbonate and titratable acid in urine. Aust J Exp Biol Med Sci 45:141–147
Hoppe P, Kay RNB, Maloiy GMO (1975) Salivary secretion in the camel. J Physiol Lond 244:32-33P
Hume ID (1982) Digestive physiology and nutrition of marsupials. Cambridge University Press, Cambridge
Hume ID, Carlisle CH (1985) Radiographic studies of the structure and function of the gastrointestinal tract of two species of potoroine marsupial. Aust J Zool 33:641–654
Kuipers GAJ, de Pont JJHHM, van Nooy IGP, Fleuren-Jakobs AMM, Bonting SL, Rodrigues de Miranda JF (1984) Amiloride is a cholinergic antagonist in the rabbit pancreas. Biochim Biophys Acta 804:237–244
Lau KR, Howorth AJ, Case RM (1990) The effects of bumetanide, amiloride and Ba2+ on fluid and electrolyte secretion in the rabbit salivary gland. J Physiol (Lond) 425:407–427
Lee AK, Cockburn A (1985) Evolutionary ecology of marsupials. Cambridge University Press, Cambridge
Martinez JR, Cassity N (1983) Effect of transport inhibitors on secretion by the perfused rat submandibular gland. Am J Physiol 245:G711–G716
Martinez JR, Cassity N (1985) Effects of 4,4′-diisothiocyano-2,2′-stilbene and amiloride on salivary secretion by isolated, perfused rat submandibular glands. Arch Oral Biol 30:797–803
Martinez JR, Barker S, Camden J (1989) Amiloride inhibits 22Na uptake and [3H]QNB binding in rat submandibular cells. Eur J Pharm 164:335–339
Novak I, Young JA (1986) Two independent anion transport systems in rabbit mandibular salivary glands. Pflugers Arch 407:649–656
Ortiz C, Cavero J, Sillau H, Cueva S (1974) The parotid saliva of the alpaca (Lama pacos). Res Vet Sci 16:54–56
Pirani D, Evans LAR, Cook DI, Young JA (1987) Intracellular pH in the rat mandibular gland; the role of Na–H and Cl–HCO3 antiports in secretion. Pflugers Arch 408:178–184
Poulsen JH, Laugesen LP, Lielsen JOD (1982) Evidence supporting that basolaterally located Na+–K+-ATPase and a co-transport system for sodium and chloride are key elements in secretion of primary saliva. In: Case RM et al (eds) Electrolyte and water transport across gastrointestinal epithelia. Raven Press, New York, pp 157–159
Scott NA, Beal AM (1994) Effects of cholinergic stimulation and aldosterone administration on salivary parotid secretion in the brushtail possum, Trichosurus vulpecula. Arch Oral Biol 39:351–360
Somner HM, Kaiser D, Drack E (1975) pH and bicarbonate excretion in the rat parotid gland as a function of salivary rate. Pflugers Arch 355:353–360
Steel RDG, Torrie JH (1960) Principles and procedures in statistics. McGraw-Hill, New York, pp 109–110
Steward MC, Poronnik P, Cook DI (1996) Bicarbonate transport in sheep parotid secretory cells. J Physiol Lond 494:819–830
Tsuganezawa H, Kobayashi K, Iyori M, Araki T, Koizuni A, Watanabi S, Kaneko A, Fukao T, Monkawa T, Yoshido T, Kim DK, Kanai Y, Endou H, Hayashi M, Saruta T (2001) A new member of the HCO3 transporter superfamily is an apical anion exchanger of beta-intercalated cells in the kidney. J Biol Chem 276:8180–8189
Wright RD, Blair-West JR, Nelson JF (1986) Effects of ouabain, amiloride, monensin, and other agents on ovine parotid secretion. Am J Physiol 250:F503–F510
Yoshimura H, Iwasasi H, Nishikawa T, Matsumoto S (1959) Role of carbonic anhydrase in the bicarbonate excretion from salivary glands and the mechanism if ionic excretion. Jpn J Physiol 9:106–123
Young JA, Martin CA, Asz M, Weber FD (1970) A microperfusion investigation of bicarbonate secretion by the rat submaxillary gland. Pflugers Arch 319:185–199
Acknowledgements
I would like to thank Abbott Australasia P/L, Astra Pharmaceuticals P/L and Lederle Laboratories for the gifts of Na pentobarbitone, bumetanide and acetazolamide, respectively. Financial support was provided by the Australian Research Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution at which the studies were conducted (Animal Care and Ethics Committee of the University of New South Wales; ACE91/146;97/37;00/41;03/40). The use of the wombats was licensed (# A100) by the NSW National Parksand Wildlife Service.
Additional information
Communicated by P. Withers.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Beal, A.M. The effect of acetazolamide, amiloride, bumetanide and SITS on secretion of fluid and electrolytes by the parotid gland of common wombats, Vombatus ursinus. J Comp Physiol B 191, 777–791 (2021). https://doi.org/10.1007/s00360-021-01367-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00360-021-01367-9