Abstract
Objectives
To comprehensively investigate the potential association between prostate cancer (PCa) and the G84E mutation within the Homeobox Protein B13 (HOXB13) gene among individuals of Turkish descent, our study aims to undertake a prospective examination.
Methods
We evaluated 300 patients (150 diagnosed with prostate cancer, 150 controls) who presented in our clinic. Data collected were prospectively examined. DNA isolation was performed using an isolation kit. The HOXB13-G84E mutation (rs138213197) was analyzed in the obtained samples. Data encoding and statistical analysis were performed.
Results
The pathological allele for the G84E mutation was T. According to the findings, no mutations were detected in the control group, while the G84E mutation was detected in 17 patients in the patient group, all of whom had the TC genotype. The analysis showed that having the CC genotype reduced the risk of prostate cancer by 0.47 times (OR=0.47, CI=0.415-0.532). Our results did not support a trend toward family history or earlier-onset disease in comparisons between carriers and non-carriers of HOXB13 G84E mutation. Individuals with a positive family history exhibited a higher frequency of the G84E mutation.
Conclusions
We concluded that HOXB13 gene mutation is indeed linked to PCa in Turkish men. However, we did not find a relationship between the HOXB13 gene G84E mutation carrier status and either early-onset PCa or familial PCa in Turkish men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) stands as the most prevalent cancer among men and ranks second in cancer-related male mortality in 2024, according to the American Cancer Society [1]. The escalated incidence in developed countries is a result of the widespread use of prostate-specific antigen (PSA) testing [2]. Variances in PCa prevalence across geographical regions and ethnicities are conspicuous. Northern and Western Europe, the Caribbean, Australia/New Zealand, North America, and South Africa exhibit the highest rates, contrasting with Asia and North Africa, where incidence rates range from 6.3 to 83.4 per 100,000 men [3].
A familial history of PCa and ethnic background noticeably heighten PCa risk [4]. The elevated incidence among families with PCa histories implies genetic susceptibility. While Hereditary prostate cancer (HPCa) correlates with earlier onset, there seems to be no disparity concerning disease aggressiveness or clinical course [5]. In the last few years, the expanding area of genetic research has shed light on cancer genetics [6, 7]. These progressions have opened doors for genetic counseling and personalized risk assessments in cancer. Specific genetic mutations have been associated with heightened PCa risk. Germline mutations, prevalent in approximately 15–17% of PCa patients irrespective of cancer stage, involve specific genes with varying frequencies. The most commonly linked genes with PCa and germline mutations include BRCA2, ATM, CHEK2, BRCA1, HOXB13, and MMR genes (MLH1, MSH2, MSH6, PMS2) [8].
The HOXB13 (Homeobox Protein B13) gene encodes the HOXB13 protein that binds to DNA. This protein belongs to the extensive group of transcription factors known as the Homeobox protein family. Notably categorized as a PCa risk gene by the National Comprehensive Cancer Network (NCCN), HOXB13 gene analysis holds potential for genetic counseling in individuals meeting specific risk criteria [9]. Though there is consensus on the association between the HOXB13 gene and PCa, it remains relatively uncommon. The precise role of these gene mutations in the pathophysiology of PCa has yet to be fully understood, although several mechanisms have been proposed. If its mechanism of action in PCa pathophysiology can be elucidated, targeting HOXB13 may soon have specific benefits in PCa treatment [10]. PCa-associated mutations in the HOXB13 gene encompass G84E, F127C, A128D, G132E, G135E, and X285K [11,12,13]. Numerous studies indicate that having the HOXB13 gene G84E (rs138213197) mutation increases the risk of PCa [11, 14, 15]. However, the rates of this mutation vary across diverse populations and ethnicities. The G84E mutation, has not been studied in Turkish men with PCa in any previous study, enhancing the originality of our research. This study aims to investigation is to determine the overall carrier frequency of the G84E mutation (rs138213197) in HOXB13 and its association with PCa in the Turkish population.
Methods
Study group
The study included 150 patients diagnosed with PCa and 150 controls diagnosed with Benign Prostate Hyperplasia (BPH) who presented to our clinic between September 2021 and August 2022. Data collected were prospectively examined. The participants were selected from those 18–80 years old and those without other malignancies. In our clinical experience, rare cases of BPH and PCa have been diagnosed in younger patients. Since the HOXB13 gene G84E mutation has been associated with familial PCa patients diagnosed at a young age in the literature, we wanted to include these younger patients, who could potentially be mutation carriers, in our prospective sample, and therefore, we chose the age range of 18–80 years. Patients who were histologically diagnosed with PCa via prostate biopsy and subsequently included in a treatment plan such as active surveillance, radical prostatectomy, or radiotherapy, as well as those who were diagnosed with PCa in the past through prostate biopsy, radical prostatectomy, or transurethral resection of the prostate (TUR-P) and presented to our clinic for routine follow-up, were included in the study. Therefore, the patients’ ages at the time of presentation and their ages at the time of PCa diagnosis were recorded. The presence of metastasis was evaluated using imaging techniques and recorded. Patients presenting with lower urinary tract symptoms (LUTS), showing prostate volume increase on ultrasound, having PSA values within the normal range, and not exhibiting any suspicious findings of malignancy on digital rectal examination were included in the control group.
The participants who met the inclusion criteria were thoroughly briefed about the study and signed an informed consent form. Demographic data and comorbidities such as age, weight, height, diabetes mellitus (DM), hypertension (HT), coronary artery disease (CAD), family history of PCa (1st and 2nd-degree relatives), smoking, and alcohol use were assessed for all individuals in both study groups.
This study received approval from the local ethics committee on 23.06.2021, under committee decision number 2021/472. Funding was provided by the University Scientific Research Projects Unit under code 2021-2-TP3-4493. Since this is a prospective study, it has been registered with the Council of Higher Education Thesis Center of the Republic of Turkey (tez.yok.gov.tr) under the reference code 10,584,905 and thesis number 833,878 at the beginning of the research.
Materials
-
1.
Centrifuge (Sigma k-15-1, Germany).
-
2.
1.5 ml capped Eppendorf tubes (Isolab, Germany).
-
3.
Automatic adjustable pipette (Eppendorf, Germany).
-
4.
+ 4 °C storage refrigerator.
-
5.
LightCycler 480 II device (Roche Cat No: 5015278).
-
6.
3 ml 7.5% EDTA tubes (BD, Vacutainer, England).
Kits
-
1.
SNP Genotyping Assay rs138213197 Assay Kit.
-
2.
TaqMan™ Genotyping Master Mix (Thermo Cat No: 4371353).
-
3.
DNA isolation kit (Roche Diagnostics, Mannheim, Germany).
DNA isolation
DNA isolation from the blood samples taken from participating patients and stored at + 4 °C was conducted using a DNA isolation kit according to the following procedure:
-
1.
200 µL whole blood was taken into a sterile 1.5 ml capped tube, followed by adding 200 µL binding buffer and 40 µL proteinase K successively. The tube caps were mixed after adding proteinase.
-
2.
The tubes were incubated at 70 °C for 10 min.
-
3.
After incubation, 100 µL isopropanol was added and thoroughly mixed, and the mixture was transferred to a filter tube.
-
4.
The mixture was centrifuged at 8000 g for one minute.
-
5.
The collection tube was changed, 500 µL of Inhibitor Removal Buffer was added, then centrifuged at 8000 g for one minute. This process was repeated, and the collection tube was changed.
-
6.
Subsequently, 500 µL of wash buffer was added to the tube, centrifuged at 8000 g for one minute, and then changed the collection tube.
-
7.
This washing process was repeated, and the collection tube was changed.
-
8.
The tube was centrifuged for 10 s at 13,000 g.
-
9.
200 µL of elution buffer at 70 °C was added to filter tubes placed into 1.5 ml capped DNA storage tubes. The mixture was centrifuged at 8000 g for one minute, completing the DNA extraction process after the filter tubes were removed with DNA elution buffer.
HOXB13-G84E analysis
Isolated DNA samples were genotyped for the G84E mutation in HOXB13 using a custom TaqMan assay (rs138213197). The analysis was performed by RT-PCR, each sample was studied in duplicate and the concordance between replicates was 100%. Empty wells were used in each plate for control and all empty wells giving no calls (Fig. 1).
Statistical analysis
Various studies investigating the HOXB13 gene G84E mutation (rs138213197) in PCa patients observed a mutation detection rate ranging from 1 to 4%. Therefore, the estimated rate for our study was 2.5%, with an estimated margin of error of ± 2%. Based on these data, a power analysis was conducted, determining a sample size of 150 individuals in both the patient and control groups.
Data collected from patients and the control group were coded and subjected to statistical analysis using SPSS 22 software. Descriptive statistics presented continuous variables as mean and median, while categorical variables were expressed as frequency and percentage.
For comparative analysis between groups, the Mann-Whitney U test was utilized for continuous variables, and the Chi-square test and Fisher’s Exact test were used for categorical variables. The correlation between variables was examined using the Spearman test. The impact of the mutation (rs138213197) on PCa risk was determined by calculating the Odds Ratio (OR). A significance level of 0.05 was adopted for all analyses. The genotype frequencies for G84E were tested for and consistent with Hardy-Weinberg equilibrium.
Results
Among all patients, the HOXB13 gene G84E mutation (rs138213197) was detected in 17 cases (5.7%). Notably, all patients carrying the HOXB13 gene G84E mutation (rs138213197) were exclusively from the PCa-diagnosed group (11.3%, p < 0.001). The HOXB13-G84E genotype was consistently TC for all mutation carriers. Upon analysis, it was found that possessing the CC genotype reduced the risk of PCa by 0.47 times (OR = 0.47, CI = 0.415–0.532).
The median age of all patients was 67.5 (IQR:62–72) years, with the PCa patient group exhibiting a statistically higher age average compared to the BPH patient group (69 [IQR:63–75]) vs. 66 [IQR:60–71], p = 0.001). Among PCa patients, the mean age at diagnosis was 65 (IQR:60–71) years. The additional demographic and clinical characteristics of the patients are detailed in Table 1.
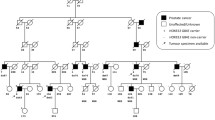
The patients diagnosed with PCa was stratified into two subgroups, as seen in Table 2: individuals carrying the G84E mutation (rs138213197) (n = 17) and those who did not (n = 133). Notably, all patients in the G84E mutation-carrying subgroup were over 55, and their age at diagnosis was also around 55. In contrast, 10.5% of the patients in the other subset were 55 or younger. Although not statistically significant, the subgroup carrying the G84E mutation (rs138213197) exhibited a higher incidence of family history (47.1% vs. 27.8%, p = 0.103) than the non-mutation-carrying subgroup.
The incidence rates of metastatic disease were comparable in both subgroups (mutation-carrying subgroup: 29.4%; non-mutation-carrying subgroup: 30.1%). Notably, all patients diagnosed with oligometastatic disease belonged to the non-mutation-carrying subset (22.6% vs. 0, p < 0.001). Besides these observations, no statistically significant associations were identified between the patients’ demographic, clinical, and pathological characteristics and the G84E mutation.
Discussion
Given the diverse genetic landscape of the Turkish population, no clinical studies have been conducted to identify the HOXB13-G84E mutation in Turkish patients diagnosed with PCa. In a survey of the Turkish population, Hamid et al. discovered heightened HOXB13 expression in PCa cells compared to non-malignant cells, suggesting the involvement of HOXB13 in cell regulation and cancer development [16]. Upon examining urinary samples from 10 Turkish PCa patients, Kavalcı et al. did not detect any variants in the HOXB13 gene, including G84E, F127C, A128D, G132E, or G135E [17]. However, in our study, 17 patients were identified with the HOXB13-G84E mutation, and all were diagnosed with PCa. All carriers of the pathological allele exhibited a heterozygous (TC) genotype. None of the 150 control group patients carried the risk allele. The analysis established a significant correlation between the G84E mutation and PCa, concluding that lacking the HOXB13-G84E risk allele reduces the disease’s risk.
Literature indicates the G84E variant to be less prevalent in individuals of African descent. However, a study on African-American PCa patients identified the G84E variant in three individuals, suggesting a potential link to genes inherited from their likely European ancestors [18]. In patients of African descent, the HOXB13 gene X285K variant is more frequently observed and associated with PCa risk [13, 19]. Researchers in different studies have identified various mutations in the HOXB13 gene among Japanese, Chinese, and Korean PCa patients, signifying a significant association between these variants and PCa risk [12, 20, 21].
Our analysis found that the PCa patient group had a higher average age than the BPH patient group. PCa is typically associated with older age, a non-modifiable risk factor for PCa [22]. With cellular aging, the propensity for cancer foci in the prostate increases. It is also known that the prevalence of BPH increases with age [23]. While BPH might manifest symptoms as early as one’s 40s, PCa typically remains asymptomatic in its initial stages, with clinical manifestations surfacing primarily in advanced stages.
In the PCa patient group, more individuals had a positive family history compared to the BPH control group, yet this was not statistically significant. Men with a family history of PCa exhibit a higher incidence of the disease than the general population [24]. In our analysis, this might be attributed to PCa cases not yet clinically apparent or diagnosed in the control group.
In our study, upon internal analysis of the PCa patient group, it was observed that all carriers of the G84E mutation were over 55. Among patients lacking this mutation, it was determined that 10.5% were under 55. Additionally, concerning family history, although statistically insignificant in the group carrying the G84E variant, a higher prevalence of positive family history was detected. Studies support the significant relationship between an early diagnosis age, positive family history, and the G84E variant [24, 25]. Kote-Jarai et al. discovered a significantly higher likelihood of the G84E mutation in patients under 55 with early-onset PCa and a positive family history [26].
Likewise, Ewing et al. found a higher prevalence of the G84E variant in PCa patients under 55 with a positive family history, concluding its significance in positive family history and early-onset PCa [27]. Akbari et al. identified a statistically significant association between PCa patients and the G84E mutation, notably in white males under 55 with a positive family history [28]. Breyer et al. identified a significantly higher prevalence of the G84E variant in PCa patients with a positive family history but did not find a relationship with an early diagnosis age [29]. Another study in Poland [30] reported a higher prevalence of the G84E mutation in PCa patients diagnosed under 60, though statistically insignificant, with a significant relationship found concerning family history. Heise et al. [11], while no significant relationship was identified between G84E mutation carriage and an early PCa diagnosis age and positive family history, relatively more G84E variants were observed in patients with a positive family history.
In exploring the relationship between different HOXB13 gene variants and PCa across diverse ethnic groups, a study detected the HOXB13 gene X285K mutation in African males, associating this variant with PCa. However, no significant relationship was established in this study between this mutation and an early diagnosis age or a positive family history [19]. In a study by Kurihara et al. on Japanese males [12], carriers of the HOXB13 gene G132E mutation exhibited a significantly lower age at PCa diagnosis, with the G132E variant notably prevalent among individuals with a positive family history.
In our study, upon internal evaluation of the PCa patient group, similar rates of metastatic disease were observed between the group carrying the G84E mutation and the group without it. There was no significant difference between the two groups concerning the TNM stage. Additionally, no significant relationship was identified between diagnostic PSA level, ISUP grade, NCCN risk classification, and G84 variant carriage. Furthermore, all patients exhibiting characteristics of oligometastatic disease were observed in the group without the G84E mutation. In a study conducted on British men, no relationship was found between the G84E variant and PSA level, Gleason score, NCCN risk class, or TNM stage [26]. Similarly, studies conducted in Poland found no significant relationship between G84E mutation carriage and diagnostic PSA levels, Gleason score, or TNM stages [11, 30]. Storebjerg et al., in their study on Danish males diagnosed with PCa undergoing radical prostatectomy, observed a significant correlation between the G84E mutation and diagnostic PSA levels, postoperative pathological examination-derived Gleason score, and positive surgical margins, suggesting a correlation between disease aggressiveness and G84E variant carriage [31]. However, data regarding the relationship between oligometastatic disease and the G84E mutation are limited.
All these findings underscore the relationship between the HOXB13 gene and PCa across diverse ethnic backgrounds and have revealed different variants. The G84E variant is notably prevalent in Europe. Our research is the first in the country to confirm the presence of the G84E variant in Turkish men and its correlation with an elevated risk of PCa, and it highlights the originality and significance of our research. In addition, our study has some limitations, including being conducted at a single center with a sample size constrained by the available budget.
Conclusion
We concluded that HOXB13 gene mutation is indeed linked to PCa in Turkish men.
However, we did not find a relationship between the HOXB13 gene G84E mutation carrier status and either early-onset PCa or familial PCa in Turkish men.
Future studies, encompassing larger samples and involving family members of mutation carriers, will further illuminate the relevance of these new genetic biomarkers in PCa and underscore their role in PCa screening programs.
Data availability
The data that support the findings of this study are openly available in the Figshare Repository at 10.6084/m9.figshare.25590552
Since this is a prospective study, it has been registered with the Council of Higher Education Thesis Center of the Republic of Turkey (tez.yok.gov.tr) under the reference code 10584905 and thesis number 833878 at the beginning of the research.
References
Siegel RL, Giaquinto AN, Jemal A (2024) Cancer statistics, 2024. CA Cancer J Clin Jan. https://doi.org/10.3322/caac.21820
Fleshner K, Carlsson SV, Roobol MJ (2017) The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA, Nature Reviews Urology, vol. 14, no. 1. Nature Publishing Group, pp. 26–37, Jan. 01, https://doi.org/10.1038/nrurol.2016.251
Sung H, Global Cancer Statistics (2020) : GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries, CA Cancer J Clin, vol. 71, no. 3, pp. 209–249, May 2021, https://doi.org/10.3322/caac.21660
Hemminki K (Apr. 2012) Familial risk and familial survival in prostate cancer. World J Urol 30:143–148. no. 210.1007/s00345-011-0801-1
Randazzo M et al (Apr. 2016) A positive family history as a risk factor for prostate cancer in a population-based study with organised prostate-specific antigen screening: results of the Swiss European randomised study of screening for prostate Cancer (ERSPC, Aarau). BJU Int 117(4):576–583. https://doi.org/10.1111/bju.13310
Seibert TM Genetic Risk Prediction for Prostate Cancer: Implications for Early Detection and Prevention, European Urology, vol. 83, no. 3., Elsevier BV et al (2023) pp. 241–248, Mar. 01, https://doi.org/10.1016/j.eururo.2022.12.021
Heidegger I et al (2019) Hereditary prostate cancer – Primetime for genetic testing? Cancer Treatment Reviews, vol. 81. W.B. Saunders Ltd, Dec. 01, https://doi.org/10.1016/j.ctrv.2019.101927
Pritchard CC et al (2016) Aug., Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer, New England Journal of Medicine, vol. 375, no. 5, pp. 443–453, https://doi.org/10.1056/nejmoa1603144
Schaeffer EM et al National Comprehensive Cancer Network (NCCN) Prostate Cancer Guideline Version 1.2023, 2023. [Online]. Available: https://www.nccn.org/home/
Halabi S et al (2024) The impact of circulating tumor cell HOXB13 RNA detection in men with metastatic castration-resistant prostate cancer (mCRPC) treated with abiraterone or enzalutamide. https://doi.org/10.1158/1078-0432.CCR-23-3017/3405221/ccr-23-3017.pdf
Heise M, Jarzemski P, Bąk A, Junkiert-Czarnecka A, Pilarska-Deltow M, Haus O (2019) G84e germline mutation in HOXB13 gene is associated with increased prostate cancer risk in Polish men. Pol J Pathol 70(2):127–133. https://doi.org/10.5114/pjp.2019.87103
Kurihara S et al (2022) Aug., Variants in HOXB13, G132E and F127C, Are Associated With Prostate Cancer Risk in Japanese Men, Cancer Diagnosis & Prognosis, vol. 2, no. 5, pp. 542–548, https://doi.org/10.21873/cdp.10139
Na R et al (2022) Mar., The HOXB13 variant X285K is associated with clinical significance and early age at diagnosis in African American prostate cancer patients, Br J Cancer, vol. 126, no. 5, pp. 791–796, https://doi.org/10.1038/s41416-021-01622-4
Dupont WD, Breyer JP, Johnson SH, Plummer WD, Smith JR (Dec. 2021) Prostate cancer risk variants of the HOXB genetic locus. Sci Rep 11(1). https://doi.org/10.1038/s41598-021-89399-7
Boyle JL et al (2020) Pathogenic Germline DNA Repair Gene and HOXB13 Mutations in Men With Metastatic Prostate Cancer,., [Online]. Available: https://doi.org/10
Hamid SM et al (Mar. 2014) HOXB13 contributes to G1/S and G2/M checkpoint controls in prostate. Mol Cell Endocrinol 383:1–2. https://doi.org/10.1016/j.mce.2013.12.003
Kavalci E, Onder AU, Brusgaard K, Bostanci A, Selhanoglu MY, Serakinci N (Feb. 2021) Identification of genetic biomarkers in urine for early detection of prostate cancer. Curr Probl Cancer 45(1). https://doi.org/10.1016/j.currproblcancer.2020.100616
Trendowski MR et al (2022) Germline variants in DNA damage repair genes and HOXB13 among black patients with early-onset prostate Cancer. https://doi.org/10.1200/PO.22
Darst BF et al (May 2022) A rare germline HOXB13 variant contributes to risk of prostate Cancer in men of African ancestry. Eur Urol 81(5):458–462. https://doi.org/10.1016/j.eururo.2021.12.023
Song SH et al (2023) Germline DNA-Repair genes and HOXB13 mutations in Korean men with metastatic prostate Cancer: data from a large Korean cohort. World J Men’s Health 41. https://doi.org/10.5534/wjmh.220190
Lin X et al (2013) Jan., A novel Germline mutation in HOXB13 is associated with prostate cancer risk in Chinese men, Prostate, vol. 73, no. 2, pp. 169–175, https://doi.org/10.1002/pros.22552
Bergengren O et al (2023) 2022 update on prostate Cancer epidemiology and risk Factors—A systematic review. Eur Urol Elsevier B V. https://doi.org/10.1016/j.eururo.2023.04.021
Shao WH, Zheng CF, Ge YC, Chen XR, Zhang BW, Wang GL, Zhang WD Age-related changes for the predictors of benign prostatic hyperplasia in Chinese men aged 40 years or older. Asian J Androl 2023 Jan-Feb ;25(1):132–136. https://doi.org/10.4103/aja202223. PMID: 35532557; PMCID: PMC9933963.
Raghallaigh BS (2022) The role of Family History and Germline Genetics in prostate Cancer Disease Profile and Screening. Exon Publications, 2022. https://doi.org/10.36255/exon-publications-urologic-cancers
Isaacs WB, Cooney KA, Xu J (2019) Updated insights into genetic contribution to prostate cancer predisposition: focus on HOXB13
Kote-Jarai Z et al (2015) Prevalence of the HOXB13 G84E germline mutation in British men and correlation with prostate cancer risk, tumour characterisitics and clinical outcomes,., [Online]. Available: http://annonc.oxfordjournals.org/
Ewing CM et al (2012) Germline Mutations in HOXB13 and Prostate Cancer Risk,., [Online]. Available: http://cran.r-project.org
Akbari MR et al (2012) Aug., Association between germline HOXB13 G84E mutation and risk of prostate cancer, J Natl Cancer Inst, vol. 104, no. 16, pp. 1260–1262, https://doi.org/10.1093/jnci/djs288
Breyer JP, Avritt TG, McReynolds KM, Dupont WD, Smith JR (2012) Confirmation of the HOXB13 G84E germline mutation in familial prostate cancer, Cancer Epidemiology Biomarkers and Prevention, vol. 21, no. 8, pp. 1348–1353, Aug. https://doi.org/10.1158/1055-9965.EPI-12-0495
Kluźniak W et al (2013) Apr., The G84E mutation in the HOXB13 gene is associated with an increased risk of prostate cancer in Poland, Prostate, vol. 73, no. 5, pp. 542–548, https://doi.org/10.1002/pros.22594
Storebjerg TM et al (Oct. 2016) Prevalence of the HOXB13 G84E mutation in Danish men undergoing radical prostatectomy and its correlations with prostate cancer risk and aggressiveness. BJU Int 118(4):646–653. https://doi.org/10.1111/bju.13416
Acknowledgements
The researchers would like to thank those who contributed to completing this research. I would like to thank the University of Mersin for this learning opportunity that helped us develop valuable life lessons of patience, perseverance, teamwork, resilience, cooperation, and, most of all, the endless pursuit of knowledge. Lastly, our thanks go to all those who have supported us in completing the research work directly or indirectly.
Funding
Funding was provided by the Mersin University Scientific Research Projects Unit under code 2021-2-TP3-4493.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received approval from the Mersin University Local Ethics Committee on 23.06.2021, under committee decision number 2021/472.
Consent for publication
The authors affirm that human research participants provided informed consent for publishing personal information.
Conflict of interest
No conflict of interest was declared by the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bıyıkoğlu, M., Tanrıverdi, R., Bozlu, M. et al. Evaluation of homeobox protein B13 (HOXB13) gene G84E mutation in patients with prostate cancer. World J Urol 42, 476 (2024). https://doi.org/10.1007/s00345-024-05186-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-05186-9