Abstract
Purpose
To evaluate the diagnostic performance of contrast-enhanced (CE) ultrasound using Sonazoid (SNZ–CEUS) by comparing with contrast-enhanced computed tomography (CE–CT) and contrast-enhanced magnetic resonance imaging (CE–MRI) for differentiating benign and malignant renal masses.
Materials and methods
306 consecutive patients (from 7 centers) with renal masses (40 benign tumors, 266 malignant tumors) diagnosed by both SNZ–CEUS, CE–CT or CE–MRI were enrolled between September 2020 and February 2021. The examinations were performed within 7 days, but the sequence was not fixed. Histologic results were available for 301 of 306 (98.37%) lesions and 5 lesions were considered benign after at least 2 year follow-up without change in size and image characteristics. The diagnostic performances were evaluated by sensitivity, specificity, positive predictive value, negative predictive value, and compared by McNemar’s test.
Results
In the head-to-head comparison, SNZ–CEUS and CE–MRI had comparable sensitivity (95.60 vs. 94.51%, P = 0.997), specificity (65.22 vs. 73.91%, P = 0.752), positive predictive value (91.58 vs. 93.48%) and negative predictive value (78.95 vs. 77.27%); SNZ–CEUS and CE–CT showed similar sensitivity (97.31 vs. 96.24%, P = 0.724); however, SNZ–CEUS had relatively lower than specificity than CE–CT (59.09 vs. 68.18%, P = 0.683). For nodules > 4 cm, CE–MRI demonstrated higher specificity than SNZ–CEUS (90.91 vs. 72.73%, P = 0.617) without compromise the sensitivity.
Conclusions
SNZ–CEUS, CE–CT, and CE–MRI demonstrate desirable and comparable sensitivity for the differentiation of renal mass. However, the specificity of all three imaging modalities is not satisfactory. SNZ–CEUS may be a suitable alternative modality for patients with renal dysfunction and those allergic to gadolinium or iodine-based agents.
Key Points
-
This prospective multicenter study demonstrated that the diagnostic performance of SNZ–CEUS was comparable to CE–CT and CE–MRI.
-
The three imaging modalities displayed desirable sensitivity, while the specificity needs to be further improved.
-
CE–MRI may have better specificity than SNZ–CEUS for differentiating renal masses bigger than 4 cm
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) was designated as being a top 10 cancer [1], which is one of the major public health problems [2]. The differentiation of malignant from benign renal lesions is essential for disease management and prognosis.
The latest 2020 European Association of Urology (EAU) guidelines specify that contrast-enhanced computed tomography (CE–CT) and contrast-enhanced magnetic resonance imaging (CE–MRI) are recommended for characterizing renal masses [3]. CT examination provides high definition and high spatial resolution. The application of MRI has been widened by the availability of advanced techniques such as diffusion-weighted and perfusion-weighted imaging [4]. However, CT examination requires the use of ionizing radiation along with potentially nephrotoxic contrast agents; and MRI examinations typically require extended image collection intervals and are not suitable for patients with metal implants or claustrophobia.
CEUS is easy accessibility and high reproducibility. Malignant renal masses show heterogeneous enhancement in cortical phase, and hypoenhancement to renal cortex in parenchymal phase according to previous study [5,6,7]. Sonazoid is a microbubble-based contrast agent consisting of perfluorobutane bubbles (mean diameter, 2.1 μm) that are stabilized using hydrogenated egg phosphatidylserine sodium [8]. Studies have shown that the lung is the major metabolic organ for the perfluorobutane component, avoiding possible nephrotoxicity [9]. Furthermore, this agent has strong, long-lasting contrast effects due to the low boiling point of perfluorobutane [10]. Therefore, it is preferred for patients with impaired kidney function or known allergic predispositions to contrast material containing iodine or gadolinium [11]. Thus, Sonazoid may provide a promising tool in the diagnosis of renal tumors.
Up to now, the diagnostic efficacy of contrast-enhanced ultrasound based on Sonazoid in renal tumors is still not clear. We carried out this multicenter study to evaluate the value of contrast-enhanced ultrasound with Sonazoid in differentiating benign and malignant renal tumors, and compared the differential diagnostic performance with CE–CT and CE–MRI.
Materials and methods
Patients
This prospective multicenter study was approved and supervised by the institutional review boards of seven participating institutions. The inclusion criteria were as follows: (1) age ≥ 18 years; (2) patient willingness to abide by the research protocol; (3) patients for whom SNZ–CEUS and CE–CT, or SNZ–CEUS and CE–MRI, were performed before the renal mass operation. The exclusion criteria were as follows: (1) unsatisfactory image; (2) undefined diagnosis (unclear histopathology diagnosis, or the follow-up period was less than 2 years for the renal mass without histopathology result); and (3) subjects who could not undergo CE–CT or CE–MRI. The SNZ–CEUS and CE–CT, or the SNZ–CEUS and CE–MRI, were performed within 7 days of one another, but the order of the examination sequence was not fixed.
SNZ–CEUS
For each center, all of the examinations were performed by a single operator with a minimum of 20 years of abdominal ultrasonographic expertise. A comprehensive evaluation of the renal mass was performed by two-dimensional ultrasound, including location, size, shape, echoic characteristics, etc., to define the optimal parameters for the examination by SNZ–CEUS. The mechanical index (MI) ranged from 0.18 to 0.20, thereby avoiding potential accidental damage from microbubbles. Following blending of Sonazoid with sterile physiological saline, a specified dose (0.015 mL/kg) of the solution was injected rapidly into the left elbow vein, immediately followed by a flush with 10 mL saline. Imaging features, including margin, shape, echogenicity, properties, enhancement model, pseudocapsule, homogeneity, unenhanced zone, wash-in and wash-out pattern were recorded. The enhancement model was classified as hyper-, iso-, and hypo-enhancement if the enhancement degree of lesion was higher, equal to or lower than the surrounding normal renal cortex. The wash-in and wash-out patterns of renal mass were defined as “early,” “iso,” or “later” compared to the peripheral renal parenchyma; The homogeneous or heterogeneous enhancement was defined as uniform distribution or with unenhanced areas in renal mass regardless of the enhancement degrees. The rim enhancement around the lesion and without washout on SNZ–CEUS is defined as pseudocapsule.
CE–CT and CE–MRI
Abdominal CE–CT scanning following intravenous administration of contrast agent was performed after the plain scan. Renal MRI examinations were performed on 1.5-T or 3-T MRI scanners. Non-contrast T1 images were acquired prior to administration of the agent. The sequences acquired by MRI include axial T1-weighted images, T2-weighted images, diffusion-weighted images, and contrast-enhanced MRI imaging.
Differentiation between benign and malignant lesions
The renal mass was classified as benign or malignant based on imaging examination. All characteristics were elucidated and reported at the ultrasonic examination by ultrasonologists with at least 20 years of abdominal imaging experience. The diagnostic result of the ultrasonic examination was acquired by radiologist with at least 20 years of abdominal imaging experience in each center, and the CEUS reports would be re-reviewed by another independent experienced ultrasonologists, and the discrepancy was solved by a more senior ultrasonologists. All of the CE–MRI and CE–CT imaging results were acquired from the original report, which was reviewed by a corresponding radiologist with at least 20 years of radiological expertise. As for the final imaging report, as long as the word “malignant” or “malignancy” was mentioned in the diagnostic result, the mass was regarded as malignant, including terms such as “considered malignant,” “possibly malignant,” “great possibility of malignancy,” except for “not malignant”. The diagnostic criteria for SNZ–CEUS are shown in Table S1. Lesions with hyper-, iso-, or hypo-enhancement in the cortical phase, and no washout in the parenchymal and late phase, or followed up for more than 2 years without any change (including size and image characteristics) were diagnosed as benign; heterogeneous echogenic masses with hyper-, iso-, or hypo-enhancement in the cortical phase that demonstrated washout in the parenchymal and late phase were considered malignant.
Statistics
Continuous variables are presented as mean ± standard deviation; categorical variables are presented as numbers and percentages. A non-paired Student’s t test was performed for comparisons of normally distributed continuous variables. The diagnostic efficiency of different examinations was evaluated by sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV), as well as their 95% CI. Sensitivity was defined as the percentage of positive (malignant) confirmed by imaging and pathology at the same time to positive of pathology. Specificity was defined as the percentage of negative results (benign) confirmed by imaging and pathology at the same time to negative of pathology or stable in the follow-up period for more than 2 years. Variables with p values < 0.05 in univariate analysis were included in the multivariate analysis by logistic regression. Interobserver agreement for SNZ–CEUS feature was evaluated by Kappa or weighted Kappa test. The subgroup analyses were performed according to the size (1–4 cm, and > 4 cm). All statistical analyses were conducted as two-sided tests using SPSS 24.0; p values of < 0.05 were considered significant.
Results
Patients and tumor characteristics
323 patients were entered into this study between September 2020 and February 2021. Of these patients, 10 and 7 were excluded due to (respectively) unsatisfactory images and undefined diagnosis, Fig. 1. The diagnostic results were confirmed by histopathology (surgery resection:172/306, 56.21%, ultrasound-guided biopsy (129/306, 42.16%) or follow-up (5/306, 1.63%) for more than 2 years. 208 patients underwent both SNZ–CEUS and CE–CT scans, 114 patients underwent both SNZ–CEUS and CE–MRI examination, and 24 patients underwent all the three examinations. In 40 cases (40/306, 13.07%), the masses were benign lesions, including 25 angioleiomyomas (ALMs), 1 adenoma, 1 oncocytoma, 5 complex cysts, 3 instances of granulomatous inflammation, and 5 cases were followed up for more than 2 years without any size and image characteristics change. In 266 cases (266/306, 86.92%), the masses were diagnosed as malignant lesions, including 224 cases of clear-cell RCC (ccRCC), 7 cases of papillary RCC, 11 cases of chromophobe RCC, 14 urothelial carcinomas, and 10 other malignant carcinomas, including 1 Wilms tumor, 1 highly differentiated squamous cell carcinoma, 1 lymphoma, 3 metastatic tumors, 2 Xp11.2 translocation TRANSCRIPTION FACTOR E3 (TFE3) gene fusion RCCs (Xp11.2/TFE3 RCCs), 1 spindle cell carcinoma, and 1 fumarate hydratase (FH)-deficient RCC. The patients and tumor characteristics, classified based on benign and malignant lesions, are presented in Table 1.
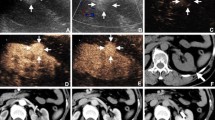
Comparison of diagnostic efficiency between SNZ–CEUS and CE–CT
Of the 208 patients (208/306, 67.97%) examined by both SNZ–CEUS and CE–CT, 187 were concordantly and correctly diagnosed by both SNZ–CEUS and CE–CT, while 14 had divergent results. Of these 14 patients, 5 (4 with ccRCCs and 1 with complex renal cyst) were correctly diagnosed by SNZ–CEUS but misdiagnosed by CE–CT. Among the 4 cases of ccRCC, 2 were misdiagnosed as adenomas and 2 as ALMs; the complex renal cysts were misdiagnosed as RCC. 1 oncocytoma was misdiagnosed by both SNZ–CEUS and CE–CT. In the head-to-head comparison between SNZ–CEUS and CE–CT (Table 2), the sensitivity (97.31 vs. 96.24%, P = 0.724), the specificity (59.09 vs. 68.18%, P = 0.683), positive predictive value (95.26 vs. 96.24%) and negative predictive value (72.22 vs. 68.18%) were similar between them. There was no statistical difference for sensitivity and specificity between the two examinations in terms of nodules bigger than 4 cm (Table S3).
Comparison of diagnostic performance between SNZ–CEUS and CE–MRI
SNZ–CEUS and CE–MRI showed comparable sensitivity (95.60 vs. 94.51%), positive predictive value (91.58 vs. 93.48%) and negative predictive value (78.95 vs. 77.27%) in the head-to-head comparison, the specificity of CE–MRI was more desirable than SNZ–CEUS (73.91 vs. 65.22%, P = 0.752) (Table 2). The CE–MRI has higher specificity than SNZ–CEUS (90.91%, 95% CI 58.72–99.77 for CE–MRI vs. 72.73%, 95% CI 39.03–93.98 for CEUS) for nodules > 4 cm when didn’t compromise the sensitivity (Table S4). Among the 114 patients (114/306, 37.25%) that underwent both SNZ–CEUS and CE–MRI examinations, 4 patients with ALM were incorrectly classified by SNZ–CEUS but correctly diagnosed by CE–MRI. Four patients with ccRCC were correctly classified by SNZ–CEUS but incorrectly diagnosed by CE–MRI. Another 3 patients were misdiagnosed by both SNZ–CEUS and CE–MRI, including, 1 adenoma and 1 case with complex renal cysts that were misdiagnosed as malignant; and 1 ccRCC that was misdiagnosed as benign.
Discussion
The study evaluated the diagnostic efficacy of Sonazoid-based contrast-enhanced ultrasound in renal tumors, and compared it with CT and MRI. The SNZ–CEUS showed satisfactory diagnostic efficiency in differentiating benign and malignant renal tumors, which provided a basis for its application in the diagnosis of renal tumors.
The diagnostic applications of CEUS in the characterization of renal masses have been investigated extensively. Previous research revealed that CEUS has high sensitivity (ranging from 93 to 97%), which is consistent with the result in this study (ranging from 95.60 to 97.31%) [12, 13]. The specificity of CEUS is lower than that of CE–CT (59.09 vs. 68.18%, P = 0.683) and CE–MRI (65.22 vs. 73.91%, P = 0.752), and the specificity all of three examination is lower than that of sensitivity. Among the benign tumors, more than half (25/40, 62.5%) were ALM and the rest of them incorporated various tumor types with atypical features. Therefore, it was hardly to find a uniform pattern of enhancement, which made the determination of benign tumors difficult, consequently may interpret the low specificity.
Comparative diagnosis between ALM and ccRCCs were the focus of this study. The image characteristics of two tumor types often overlap, which may impede effective diagnosis between them. In the head-to-head comparison, 4 patients with ccRCCs were misdiagnosed by CE–CT and CE–MRI, respectively, and 4 ALMs were incorrectly classified by SNZ–CEUS. A previous study reported that the percentage of macroscopic fat is a key criterion for diagnosing ALM [5], and ALMs typically contain macroscopic fat. Early studies also reported difficulties in discriminating between ALM and RCC [14]. A prospective study by Ascenti et al. [15] showed that ALM had a large range of variable characteristics concerning contrast enhancement. Smaller ccRCCs also have been reported to demonstrate homogeneous enhancement [16], and some ALM cases can present as hyperenhancement and pseudocapsules or more complicated image representation [17] on CEUS images.
Resolution of temporal and space-related properties is much higher with CEUS than that with CT or MRI [18]. Consistent with that interpretation, an early study suggested CEUS as an alternative to MRI for imaging examination and diagnosis of renal masses [19, 20]. Previous work has shown that the majority of malignant renal masses show heterogeneous enhancement, given that invasive growth was more likely to lead to bleeding; thus, malignant renal masses often contain hemorrhages or necrotic regions, such that imaging with CE agents exhibits nonenhanced areas. In this study, unenhanced zone within the tumor was the independent risk factor between benign and malignant renal mass.
This study has some limitations. First, CEUS was performed by 7 radiologists from 7 centers, the report may be affected due to the highly operator-dependent property of CEUS, although each operator with a minimum of 20 years of abdominal ultrasonographic expertise. Second, there is no strict criterion for the choice of CE–CT or CE–MRI, about half of the renal masses (129/306, 42.16%) were cured by ultrasound-guided microwave ablation, and the study incorporate 5 lesions without histopathological confirmation, all the factors may lead to potential selection bias. In addition, the scanners and contrast agents used for CT and MRI at different institutions may slightly discrepant, which might affect the diagnostic performance.
Conclusions
This study confirmed that SNZ–CEUS is a valuable diagnostic tool for differentiating renal masses. Given the known limitations of CE–CT, which may expose to the ionizing radiation, and CE–MRI, which cannot be used in patients with metal implants or claustrophobia, SNZ–CEUS may be a suitable alternative modality for patients with renal dysfunction and those allergic to gadolinium or iodine-based agents.
Data availability
The article does not contain applicable data availability statements.
Change history
13 June 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00345-024-05075-1
Abbreviations
- ALMs:
-
Angioleiomyomas
- BMI:
-
Body mass index
- ccRCC:
-
Clear-cell RCC
- CE:
-
Contrast-enhanced
- CE–CT:
-
Contrast-enhanced computed tomography
- CE–MRI:
-
Contrast-enhanced magnetic resonance imaging
- CEUS:
-
Contrast-enhanced ultrasound
- EAU:
-
European Association of Urology
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RCC:
-
Renal cell carcinoma
- SNZ–CEUS:
-
Contrast-enhanced ultrasound using Sonazoid
- TFE3:
-
Transcription factor e3
References
Siegel RL, Miller KD, Fuchs HE et al (2021) Cancer statistics, 2021. CA Cancer J Clin 71:7
Ferlay J, Colombet M, Soerjomataram I et al (2018) Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 103:356
Ljungberg B, Bensalah K, Canfield S et al (2015) EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 67:913
Song XD, Tian YN, Li H et al (2020) Research progress on advanced renal cell carcinoma. J Int Med Res 48:300060520924265
Barr RG, Peterson C, Hindi A (2014) Evaluation of indeterminate renal masses with contrast-enhanced US: a diagnostic performance study. Radiology 271:133
Kazmierski B, Deurdulian C, Tchelepi H et al (2018) Applications of contrast-enhanced ultrasound in the kidney. Abdom Radiol 43:880
Bertolotto M, Bucci S, Valentino M et al (2018) Contrast-enhanced ultrasound for characterizing renal masses. Eur J Radiol 105:41
Tsuruoka K, Yasuda T, Koitabashi K et al (2010) Evaluation of renal microcirculation by contrast-enhanced ultrasound with Sonazoid as a contrast agent. Int Heart J 51:176
Miyoshi T, Okayama H, Hiasa G et al (2016) Contrast-enhanced ultrasound for the evaluation of acute renal infarction. J Med Ultrason 43(141):2016
Siedlecki AM, Benson C, Frates M et al (2019) First report of perfluorobutane microsphere-enhanced ultrasound in the transplant kidney. Transplantation 103:e283
Davenport MS, Cohan RH, Ellis JH (2015) Contrast media controversies in 2015: imaging patients with renal impairment or risk of contrast reaction. AJR Am J Roentgenol 204:1174
Shen L, Li Y, Li N et al (2019) Clinical utility of contrast-enhanced ultrasonography in the diagnosis of benign and malignant small renal masses among Asian population. Cancer Med 8:7532
Furrer MA, Spycher SCJ, Büttiker SM et al (2020) Comparison of the diagnostic performance of contrast-enhanced ultrasound with that of contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging in the evaluation of renal masses: a systematic review and meta-analysis. Eur Urol Oncol 3:464
Cai Y, Du L, Li F et al (2014) Quantification of enhancement of renal parenchymal masses with contrast-enhanced ultrasound. Ultrasound Med Biol 40:1387
Ascenti G, Zimbaro G, Mazziotti S et al (2001) Usefulness of power doppler and contrast-enhanced sonography in the differentiation of hyperechoic renal masses. Abdom Imaging 26:654
Lu Q, Huang BJ, Wang WP et al (2015) Qualitative and quantitative analysis with contrast-enhanced ultrasonography: diagnosis value in hypoechoic renal angiomyolipoma. Korean J Radiol 16:334
Ignee A, Straub B, Schuessler G et al (2010) Contrast enhanced ultrasound of renal masses. World J Radiol 2:15
Aoki S, Hattori R, Yamamoto T et al (2011) Contrast-enhanced ultrasound using a time-intensity curve for the diagnosis of renal cell carcinoma. BJU Int 108:349
Gassert F, Schnitzer M, Kim SH et al (2021) Comparison of magnetic resonance imaging and contrast-enhanced ultrasound as diagnostic options for unclear cystic renal lesions: a cost-effectiveness analysis. Ultraschall Med 42:411
Zhao P, Zhu J, Wang L et al (2023) Comparative diagnostic performance of contrast-enhanced ultrasound and dynamic contrast-enhanced magnetic resonance imaging for differentiating clear cell and non-clear cell renal cell carcinoma. Eur Radiol 33:3766
Funding
This work was supported by Grants 81871374 and 82171941, 91859201 and 82030047 from the National Scientific Foundation Committee of China. The funders had no role in data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Concept and design: Ping Liang, Zhi-gang Cheng. Experiments and procedures: All authors. Writing of article: Qin-xian Zhao, Yang Bai. Statistical analysis: Qin-xian Zhao, Yang Bai, Ming-jing Mei; Case collection: Qin-xian Zhao, Chong Wu, Hai-xiang Zhang, Mei-mei Zhu, Xiang-ru Dong, Hua Liang, Si-jie Yuan, Yue Song. Thanks for support of GE healthcare pharmaceutical diagnostics medical affairs for contributing to the data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to this work. We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethical approval
The study was approved and supervised by the institutional review boards of the seven participating institutions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to incorrect first author name. Now, it has been corrected from Qin-xin Zhao to Qin-xian Zhao.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, Qx., Wu, C., Tan, S. et al. Comparing Sonazoid contrast-enhanced ultrasound to contrast-enhanced CT and MRI for differentially diagnosing renal lesions: a prospective multicenter study. World J Urol 42, 302 (2024). https://doi.org/10.1007/s00345-024-04885-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04885-7