Abstract
Purpose
Hypospadias surgery is challenging. Numerous techniques have been described with variable complication rates. The main objectives of our study were to evaluate the urethroplasty complication rate of primary hypospadias repair and to identify risk factors for complications.
Methods
We retrospectively evaluated the outcomes of all patients who underwent primary hypospadias repair in our department between January 2012 and December 2020. Demographic, anatomical, operative, and postoperative data were reported. Univariate and multivariate logistic regression analyses were performed to identify variables associated with complications. Statistical significance was set at p < 0.05.
Results
Of 292 patients, 203 (69.5%) had distal hypospadias, 63 (21.6%) had mid-penile hypospadias, and 26 (8.9%) had proximal hypospadias. The mean age at the time of surgery was 22.8 months. Seventy-eight patients (26.7%) had urethroplasty complications. The rate of complications was higher for proximal hypospadias (57.7%), onlay island flap (44.4%), and Koyanagi (75%) procedures. The mean follow-up duration was 29 months. Two predictors of complications were identified by multivariate analysis: catheterization duration and urethroplasty technique. The reoperation rate was 30.5%.
Conclusion
Urethroplasty complications frequently occur after primary hypospadias repair. The complication rate was higher in proximal hypospadias. Catheterization duration and surgical technique were significant predictors of complications. A longer and more standardized follow-up is needed for a better assessment of hypospadias repair outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypospadias is a common urogenital anomaly in males [1]. Hypospadias represent a heterogeneous entity with different types and grades of severity. Treatment is mainly surgical, often performed between 6 and 18 months of age [2]. Numerous correction techniques have been described but none of them has proven to be superior [3, 4]. Hypospadias surgical repair remains challenging with a high rate of complications that can reach 60% for the most severe grades [5,6,7,8]. Many questions remain unanswered regarding the classification of hypospadias [9, 10], the optimal age to perform the primary repair [11], the choice of surgical technique [12], and the postoperative management. There is no gold standard of care in hypospadias management and decisions are mainly based on the surgeon’s preference.
Therefore, we aimed to evaluate the outcomes of primary hypospadias repair performed in our department. The main objectives of our study were to analyze urethroplasty complications and to identify their risk factors.
Materials and methods
We retrospectively identified and reviewed data of all patients who underwent primary hypospadias repair between January 2012 and December 2020 at our Department of Pediatric Surgery. Patients who underwent a primary hypospadias repair before 2012 or in another department, operated with staged procedures, operated for other genital issues or who did not have hypospadias and patients who failed to attend the follow-up consultations were excluded. The demographic, anatomical, operative, and postoperative data were obtained from the patient files. Urological and cosmetic results were also collected. The assessments of the final cosmetic outcomes were based on clinical evaluation by the surgeon.
Data were reported as means and ranges for the continuous variables, and as numbers and percentages for the categorical variables. Continuous variables were compared using the Mann–Whitney U test. Discrete variables were analyzed using the chi-squared test or Fisher's exact test. Univariate and multivariate logistic regression analyses were used to identify variables predicting complications. A p value < 0.05 was considered statistically significant.
This study did not require IRB approval.
Results
Patients and grades of hypospadias
Of the 357 patients identified in our database 41 were excluded because they failed to attend the postoperative checkup, 13 because they had undergone a primary repair before 2012 (n = 6) or in another hospital (n = 7) and 11 because surgery was performed for another genital malformation. We ultimately included 292 patients.
All demographic, anatomical, and surgical data are shown in Table 1. Fifty patients (17.1%) presented associated genital anomalies of whom 27 had micropenis preoperatively treated with androgen stimulation.
Hypospadias were classified according to the meatal position description found in the medical records or surgical report. If different, the perioperative description was chosen. Patients were regrouped into three grades of hypospadias: distal hypospadias (n = 203) with the meatus in a glandular, coronal, sub-coronal, or anterior penile position; mid-penile hypospadias (n = 63); and proximal hypospadias (n = 26) with the meatus in a posterior penile, penoscrotal, scrotal, or perineal position. The mean age at surgery was 22.8 months [5–170 months]. The mean postoperative catheterization time was 3.67 days [0–13 days].
Technique for primary repair
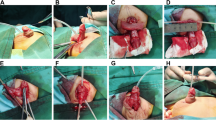
Numerous techniques were used for primary repair based on the surgical evaluation and the surgeon’s preference: meatal advancement (MAGPI), primary plate tubularization and modifications (Duplay and Snodgrass procedures), complete urethral mobilization (Koff procedure), meatal-based flap technique (Mathieu procedure), transverse island flap technique (Duckett procedure), onlay island flap, and Koyanagi one-stage repair. Figure 1 shows the proportion of techniques performed overall and for each grade of hypospadias.
Follow-up
The mean follow-up after first surgery was 29 months [1–118 months]. It was 23 months for patients without complications and 46 months for those with complications.
Complications
In 292 patients, 78 (26.7%) presented at least one complication during follow-up. Among all complications we noted 40 urethrocutaneous fistulas (13.7%), 29 meatal strictures (9.9%) and 22 urethroplasty dehiscences (7.6%). The complication rate was higher in proximal hypospadias (57.7%) than in mid-penile hypospadias (39.7%) and distal hypospadias (18.7%). The complication rate also varied depending on the surgical technique: meatoplasty and MAGPI 0%, complete urethral mobilization 12.5%, meatal-based flap 25%, primary plate tubularization and modifications 27% (Duplay 27.1%, Snodgrass 27.4%), onlay island flap 44%, Koyanagi one-stage repair 75%, and transverse island flap 89%.
During the study period a total of 409 surgeries were performed on 292 patients, equating to a mean of 1.4 surgery per patient [1,2,3,4,5,6] and a reoperation rate of 30.5%.
Risk factors for complications
Patients were divided into two groups based on whether or not they presented an urethroplasty complication. Potential risk factors for complications were evaluated for each group: age at first surgery, associated genital anomalies, grade of hypospadias, surgical technique, and duration of catheterization.
The results of the univariate analysis are presented in Table 2. There was a significant association between urethroplasty complications and the grade of hypospadias (p < 0.001), surgical technique (p < 0.001), catheterization duration (p < 0.001), and associated genital anomalies (p = 0.002).
Multiple logistic regression including significant factors in the univariate analysis demonstrated that the type of urethroplasty (p = 0.03) and the catheterization duration (RR 1.3, 95% CI 1.01; 1.72) were independent risk factors for complications. There was no significant association between complications and associated genital anomalies (p = 0.08), the grade of hypospadias (p = 0.05), or the age at first surgery (p = 0.7).
Urological and cosmetic outcomes
Urinary symptoms were diagnosed in 3.8% of patients. Postoperatively, 44 patients (15.1%) underwent uroflowmetry. Only six were abnormal with a maximum flow rate of < 10 mL/s. None of these six patients were symptomatic.
For 227 patients (77.7%), the surgeon was satisfied with the final cosmetic outcome. The main cosmetic issue (65%) was redundant skin. The urethral meatus was in a glandular position in 94.2% of patients. Persistent curvature was found in 6.5% of the patients. Among patients with unsatisfactory cosmetic results, only 25 (38.5%) underwent reoperation.
Discussion
In this study, 78 patients (26.7%) presented one or more urethroplasty complications. The overall complication rate is rarely reported in the literature as studies tend to report complications related to a specific grade of hypospadias or a type of urethroplasty. Some series reporting overall complication rates had similar results, with complication rates of 24%–31% [13, 14]. The complication rate depends on the grade of hypospadias and the type of urethroplasty. In our study, it ranged from 18.7% for the distal forms to 39.7% and 57.7% for the mid-penile and proximal forms, respectively. These results are consistent with several studies in the literature [8, 15]. For hypospadias who underwent primary plate tubularization procedures, the complication rate was 27.1% (Duplay procedure) and 27.4% (Snodgrass procedure). Braga et al. reported a complication rate of 10% using these techniques, but only for distal forms of hypospadias [16]. The relatively high complication rate in our study could be explained by the large number of mid-penile hypospadias operated using these techniques (89%). Other studies have reported similar results using these urethroplasties for mid-penile and proximal hypospadias [15, 17].
The complication rate was substantial for onlay island flap and Koyanagi urethroplasties, at 44.4% and 75%, respectively. Outcomes after onlay island flap urethroplasty are highly variable with a complication rate of 20% to 57% [15, 17,18,19]. The results reported in the literature for Koyanagi urethroplasty generally indicate a complication rate approximately 65% [20, 21]. Koyanagi urethroplasty outcomes are difficult to compare with authors considering it a two-step procedure [21]. In this series, the small number of patients operated with this technique may have influenced our results. But this result also reflects the impact of the surgeon's experience in severe hypospadias surgery [13].
Univariate analysis revealed a significant association between the grade of hypospadias and complications. Surprisingly, this association was not confirmed in multivariate analysis (p = 0.05) but was at the limit of the statistical significance. Spinoit et al. identified the grade of hypospadias as the only risk factor for reintervention [22]. Our result could be explained by the relatively small number of patients with proximal hypospadias (n = 26, 8.9%). An increase in the size of our cohort would probably lead to another conclusion.
In this study, the duration of postoperative bladder catheterization was identified as a risk factor for complications in multivariate analysis. A longer catheterization time was associated with an increased rate of complications. These results warrant further discussion. Indeed, the catheterization duration is associated with the severity of the malformation and, consequently, with the complexity of the urethroplasty which may constitute a bias. Furthermore, postoperative antibiotic prophylaxis remains debated [23]. Its role in limiting the risk of complications has not been proven. A recent meta-analysis did not show any benefit from the use of systematic antibiotic prophylaxis [24]. However, this study only focused on distal hypospadias. Data on postoperative antibiotic prophylaxis in our cohort were unavailable. Therefore, its possible impact on complications related to bladder catheterization could not be studied.
The optimal age for the first hypospadias surgery remains an issue of debate [11]. It was initially performed at 2 years of age. The age for the first repair has been progressively lowered with some teams considering that the risk of complications increases after 6 months of age [11]. Conversely, a recent study by Tack et al. showed an increased risk of reoperation if the first surgery is performed before the age of 12 months [25]. The current recommendations of the European Association of Urology are to perform the first surgery between 6 and 18 months of age [26]. In our retrospective cohort, the mean age at first surgery was 22.8 months. Although this is slightly higher than what is recommended it did not emerge as a risk factor for complications.
Patients lost to follow-up are a genuine concern. In our study, 41 (11.5%) potentially eligible patients were excluded because they had not consulted after the first surgery. Among the included patients, 98 (33.6%) had still not had follow-up 1 year after the last scheduled appointment. The modalities for hypospadias follow-up are unclear and its organization lacks standardization. Spinoit et al. proposed a standardized follow-up protocol at 6 days, 6 weeks, 6 months, then at the age compatible with uroflowmetry and finally at puberty [27]. The substantial number of patients lost to follow-up may be explained by the absence of a validated postoperative protocol.
Our study has some limitations. First, data were gathered retrospectively, thus exposing to a risk of missing information. Reporting outcomes of hypospadias surgery is challenging because of the lack of consensus regarding its management. Even hypospadias classification is subject to debate [9, 10, 28]. In this study, we classified hypospadias on a meatal position basis as it is often done [9]. This classification is subject to a lack of objectivity and reproducibility. As mentioned by some authors, other criteria such as the position of the corpus spongiosum divisum or the quality of the urethral plate should be taken into account [29]. The use of more objective classifications may help with standardizing outcome reports [30].
The evaluation of the meatal position was carried out preoperatively and sometimes corrected perioperatively if this evaluation was different. However, perioperative evaluation was sometimes missing and this may have led to an underestimation of the severity of the hypospadias. As it concerns the whole cohort, it probably did not generate any differences between the two groups. Without any recommendations guiding the choice of urethroplasty technique, this choice was mainly based on the surgeon’s preference. This could represent another bias.
Operative report did not mentioned the use of an intermediate protective layer to cover the neourethra. As the use of this protection might have a role on decreasing the incidence of urethrocutaneous fistula, it may have impact our results.
Finally, limited follow-up with a minimum follow-up period of 1 month and 25% of patients with less than 6 months follow-up is another bias in assessing complications after hypospadias surgery.
Despite these limitations, the strength of our study is that it reports the outcomes of a large cohort including all grades of hypospadias operated with various techniques. It has the advantage of reporting usual practices and its results offer a broad view of hypospadias management.
Conclusions
Urethroplasty complications frequently occur after primary hypospadias repair. In this retrospective study, 26.7% of patients presented one or more urethroplasty complications during follow-up. The rate of complications increases with hypospadias severity, reaching 57.7% in proximal hypospadias. The catheterization duration and the surgical technique were identified as significant predictors of complications, but association could be biased. A longer and more standardized follow-up is needed, however, for a better assessment of hypospadias repair outcomes.
Data availability
Not applicable.
References
Springer A, Van Den Heijkant M, Baumann S (2016) Worldwide prevalence of hypospadias. J Pediatr Urol 12:152-e1
Keays MA, Dave S (2017) Current hypospadias management: diagnosis, surgical management, and long-term patient-centred outcomes. Can Urol Assoc J 11:S48–S53. https://doi.org/10.5489/cuaj.4386
Subramaniam R, Spinoit AF, Hoebeke P (2011) Hypospadias repair: an overview of the actual techniques. Semin Plast Surg 25:206–212. https://doi.org/10.1055/s-0031-1281490
Snodgrass W, Bush N (2016) Primary hypospadias repair techniques: a review of the evidence. Urol Ann 8:403–408. https://doi.org/10.4103/0974-7796.192097
Thiry S, Saussez T, Dormeus S, Tombal B, Wese FX, Feyaerts A (2015) Long-term functional, cosmetic and sexual outcomes of hypospadias correction performed in childhood. Urol Int 95:137–141. https://doi.org/10.1159/000430500
Örtqvist L, Fossum M, Andersson M, Nordenström A, Frisén L, Holmdahl G, Nordenskjöld A (2015) Long-term followup of men born with hypospadias: urological and cosmetic results. J Urol 193:975–982. https://doi.org/10.1016/j.juro.2014.09.103
Jaber J, Kocherov S, Chertin L, Farkas A, Chertin B (2017) Voiding patterns of adult patients who underwent hypospadias repair in childhood. J Pediatr Urol 13:78-e1
Rynja SP, de Kort LMO, de Jong TPVM (2012) Urinary, sexual, and cosmetic results after puberty in hypospadias repair: current results and trends. Curr Opin Urol 22:453–456. https://doi.org/10.1097/MOU.0b013e328357bc9e
Hadidi AT (2004) Classification of hypospadias. In: Hypospadias surgery. Springer, pp 79–82
Orkiszewski M (2012) A standardized classification of hypospadias. J Pediatr Urol 8:410–414. https://doi.org/10.1016/j.jpurol.2011.08.011
Perlmutter AE, Morabito R, Tarry WF (2006) Impact of patient age on distal hypospadias repair: a surgical perspective. Urology 68:648–651. https://doi.org/10.1016/j.urology.2006.03.079
Mouriquand PDE, Persad R, Sharma S (1995) Hypospadias repair: current principles and procedures. Br J Urol 76:9–22
Ceccarelli PL, Lucaccioni L, Poluzzi F, Bianchini A, Biondini D, Iughetti L, Predieri B (2021) Hypospadias: clinical approach, surgical technique and long-term outcome. BMC Pediatr 21:523. https://doi.org/10.1186/s12887-021-02941-4
Dokter EM, Mouës CM, van Rooij IALM, van der Biezen JJ (2018) Complications after hypospadias correction: prognostic factors and impact on final clinical outcome. Eur J Pediatr Surg Off J Austrian Assoc Pediatr Surg Al Z Kinderchir 28:200–206. https://doi.org/10.1055/s-0037-1599230
Prat D, Natasha A, Polak A, Koulikov D, Prat O, Zilberman M, Abu Arafeh W, Moriel EZ, Shenfeld OZ, Mor Y, Farkas A, Chertin B (2012) Surgical outcome of different types of primary hypospadias repair during three decades in a single center. Urology 79:1350–1354. https://doi.org/10.1016/j.urology.2011.11.085
Braga LHP, Lorenzo AJ, Salle JLP (2008) Tubularized incised plate urethroplasty for distal hypospadias: a literature review. Indian J Urol IJU J Urol Soc India 24:219–225
Castagnetti M, El-Ghoneimi A (2010) Surgical management of primary severe hypospadias in children: systematic 20-year review. J Urol 184:1469–1475
Cambareri GM, Yap M, Kaplan GW (2016) Hypospadias repair with onlay preputial graft: a 25-year experience with long-term follow-up. BJU Int 118:451–457. https://doi.org/10.1111/bju.13419
Wang C-X, Zhang W-P, Song H-C (2019) Complications of proximal hypospadias repair with transverse preputial island flap urethroplasty: a 15-year experience with long-term follow-up. Asian J Androl 21:300–303. https://doi.org/10.4103/aja.aja_115_18
de Mattos e Silva E, Gorduza DB, Catti M, Valmalle AF, Demède D, Hameury F, Pierre-Yves M, Mouriquand P (2009) Outcome of severe hypospadias repair using three different techniques. J Pediatr Urol 5:205–211. https://doi.org/10.1016/j.jpurol.2008.12.010
Madec F-X, Desplanches M, Chabaud M, Irtan S, Suply E, Audry G (2022) Koyanagi urethroplasty for proximal hypospadias: a stage procedure? Prog En Urol 32:312–318. https://doi.org/10.1016/j.purol.2021.09.008
Spinoit A-F, Poelaert F, Van Praet C, Groen L-A, Van Laecke E, Hoebeke P (2015) Grade of hypospadias is the only factor predicting for re-intervention after primary hypospadias repair: a multivariate analysis from a cohort of 474 patients. J Pediatr Urol 11:70.e1–6. https://doi.org/10.1016/j.jpurol.2014.11.014
Kanaroglou N, Wehbi E, Alotay A, Bagli DJ, Koyle MA, Lorenzo AJ, Farhat WA (2013) Is there a role for prophylactic antibiotics after stented hypospadias repair? J Urol 190:1535–1539. https://doi.org/10.1016/j.juro.2013.02.015
Chua ME, Kim JK, Rivera KC, Ming JM, Flores F, Farhat WA (2019) The use of postoperative prophylactic antibiotics in stented distal hypospadias repair: a systematic review and meta-analysis. J Pediatr Urol 15:138–148. https://doi.org/10.1016/j.jpurol.2018.10.012
Tack LJW, Springer A, Riedl S, Tonnhofer U, Hiess M, Weninger J, Mahmoud A, Van LE, Hoebeke P, Cools M, Spinoit A-F (2021) Adolescent and young adult urogenital outcome following childhood hypospadias repair: perfection revisited. J Urol 206:734–744. https://doi.org/10.1097/JU.0000000000001869
EAU Guidelines on Paediatric Urology. ISBN 978-94-92671-16-5 (2022).
Spinoit A-F, Poelaert F, Groen L-A, Van Laecke E, Hoebeke P (2013) Hypospadias repair at a tertiary care center: long-term followup is mandatory to determine the real complication rate. J Urol 189:2276–2281. https://doi.org/10.1016/j.juro.2012.12.100
Snodgrass W, Macedo A, Hoebeke P, Mouriquand PD (2011) Hypospadias dilemmas: a round table. J Pediatr Urol 7:145–157
Mouriquand PDE, Gorduza DB, Noché M-E, Targnion A (2011) Long-term outcome of hypospadias surgery: current dilemmas. Curr Opin Urol 21:465–469. https://doi.org/10.1097/MOU.0b013e32834a6da3
Abbas TO (2022) An objective hypospadias classification system. J Pediatr Urol 18:481.e1-481.e8. https://doi.org/10.1016/j.jpurol.2022.05.001
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
OH: protocol development, data collection, manuscript writing. AFK: data analysis. NB: data collection. FA: project development. YC: protocol development, manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflicts of interest or financial ties to disclose.
Ethics approval
This study did not require IRB approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hild, O., Fotso Kamdem, A., Boulard, N. et al. Primary hypospadias repair outcomes: results from a retrospective cohort of 292 children. World J Urol 42, 137 (2024). https://doi.org/10.1007/s00345-024-04811-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04811-x