Abstract
Purpose
To evaluate the feasibility, safety, and early oncologic outcomes after post-chemotherapy robot-assisted retroperitoneal lymph node dissection (PC-RARPLND) for metastatic germ cell tumors (mGCT).
Methods
We retrospectively analyzed patients from four tertiary centers who underwent PC-RARPLND for mGCT, from 2011 to 2021. Previous treatment of mGCT, intraoperative and postoperative complications, and early oncologic outcomes were assessed.
Results
Overall, 66 patients were included. The majority of patients had non-seminoma mTGCT (89%). Median size of retroperitoneal lymph node (RLN) before surgery was 26 mm. Templates of PC-RARPLND were left modified, right modified, and full bilateral in 56%, 27%, and 14%, respectively. Median estimated blood loss and length of stay were 50 mL [50–150] and 2 [1–3] days. Four patients (6.1%) had a vascular injury, only one with significant blood loss and conversion to open surgery (OS). Two other patients had a conversion to OS for difficulty of dissection. No patient had transfusion, most frequent complications were ileus (10.6%) and symptomatic lymphorrea (7.6%) and no complications grade IIIb or more occurred. With a median follow-up of 16 months, two patients had a relapse, all outside of the surgical template (one in the retrocrural space with reascending markers, one in lungs).
Conclusion
PC-RARPLND is a challenging surgery. In expert centers and for selected patients, it seemed safe and feasible, with a low morbidity. Further prospective evaluation of this procedure and long-term oncologic results are needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Testicular germ cell tumors (GCT) occur mostly in young patients, and are highly curable, even in case of metastatic spread [1,2,3]. The management requires multidisciplinary collaboration and high expertise. In case of retroperitoneal lymph node metastasis, upfront cisplatin-based chemotherapy is mostly proposed, with three or four cycles of BEP according to IGCCCG risk group. Subsequently, post-chemotherapy retroperitoneal lymph node dissection (RPLND) is indicated for supracentimetric residual mass (non-seminoma GCT) or more than 3 cm hypermetabolic masses (seminoma GCT).
Robot-assisted surgery has become widely used for radical prostatectomy [4], partial nephrectomy [5], and is increasing also for radical cystectomy [6]. For urologists with extensive experience in robotic surgery, RPLND may represent the next challenge, keeping in mind that no compromise regarding the extent of surgery due to the surgical approach could be accepted [7].
Logically, robot-assisted RPLND started initially for stage I diseases [8], avoiding the potential difficulties of chemotherapy-induced modifications of the tissues. However, most of RPLNDs in Europe are nowadays planned in a post-chemotherapy setting [9], considering the superiority of adjuvant chemotherapy upon primary RPLND [10], the chemosensitivity of seminomas, and the rareness of stage IIA non-seminoma germ cell tumor with negative markers. Post-chemotherapy RPLND remains a demanding surgery, and open RPLND is undoubtedly the standard [3]. Evidently, PC-RARPLND will not replace open PC-RPLND for all cases, as the great extent of the disease frequently precludes a minimally invasive approach [11]. However, in selected cases, PC-RARPLND is proposed in more and more expert centers to improve perioperative outcomes [12].
Oncological concerns have been previously published regarding PC-RARPLND [13], suggesting that pneuperitoneum could alter the natural history of surgical relapses, describing paracolic recurrences or peritoneal carcinomatosis. Nevertheless, recent reports showed favorable oncological outcomes, without unusual recurrences [14,15,16]. Moreover, surgical safety is an important aspect to be questioned, since operating close to the large vessels could be associated with major bleeding complications, delicate to control in a robot-assisted laparoscopic setting.
Until now, no prospective trial has been published in this setting, and small retrospective series only started to emerge recently. Therefore, there is an unmet need for a comprehensive and contemporary analysis of a large PC-RARPLND series. Thus, the aim of this study was to describe our multicenter experience in patients managed with R-RPLND regarding perioperative and early oncological outcomes.
Methods
Study population
All patients who underwent post-chemotherapy robotic retroperitoneal lymph node dissection for metastatic germ cell tumor in four tertiary care centers from 2011 to August 2021, were retrospectively included. Patients with previous RPLNDs were excluded. RARPLNDs were classified “post-chemotherapy” when patients classically finished chemotherapy 4–6 weeks before surgery, or when patients had a history of successful first-line chemotherapy for stage II disease, and relapsed thereafter (considering that tissues had been significantly modified by the exposure of multiple cycles of chemotherapy in this setting). All patients were staged with CT scans before and after chemotherapy, and serum tumor markers (α-fetoprotein, human chorionic gonadotropin, and lactate dehydrogenase). Before surgery, all patients were discussed at multidisciplinary meetings including urologists, radiologists, medical oncologists, and radiation therapists. Institutional review board approved the study (ROBOTESTIS-IPC-2021-039). Follow-up was performed according to international guidelines: serum tumor markers every 3 months and CT scans every 6 months during the first 2 years, with reduced frequency thereafter.
Surgical technique
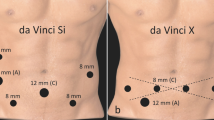
Every procedure was done by experienced robotic surgeons (FB, JCB, GR, ND, JBB, GV, JW). Patient positioning (decubitus dorsal or decubitus lateral) and port placement depended on surgeon’s preference. The extension of the templates was decided by each surgeon and depended on the size and location of the mass(es) in imaging. Postoperative drainage depended on surgeon’s preference.
Outcomes of interest
Preoperative data [histology of tumor at orchiectomy, history of chemotherapy, initial stage of the disease or relapse, location and size of the mass(es)], perioperative (length of surgery, estimated blood loss, intraoperative complications), and postoperative data (complications, pathologic results, relapse) were collected and analyzed. Regarding pathological results, patients were divided into three exclusive categories: necrosis/fibrosis only, teratoma (with or without necrosis/fibrosis, but without viable tumor), and viable tumor (whether concomitant teratoma or not). Postoperative complications were assessed using the Clavien–Dindo classification.
Statistical analysis
Descriptive statistics included frequencies and proportions for categorical variables. Means, medians, and ranges were reported for continuously coded variables. The statistical significance of differences in medians and proportions was evaluated with the Kruskal–Wallis and Chi-square tests. Univariable and multivariable logistic regression models tested the relationship between complications (all complications and severe complications) and several variables, namely age, body mass index (BMI), time between orchiectomy and lymph node dissection, type of preoperative chemotherapy, number of cycles of chemotherapy, type of lymph node dissection, intraoperative blood loss, intraoperative patient positioning, operative time, and histological type. They were included in the multivariable models if significantly associated with the outcome in the univariable analysis.
For all statistical analyses, R software environment for statistical computing and graphics (version 3.4.3) was used. All tests were two sided with a level of significance set at p < 0.05.
Results
Patient characteristics
Overall, 66 patients, with a median age of 34 years, were included (Table 1). The majority of patients had non-seminoma germ cell tumors (59 patients, 89%).
The majority of patients had lymph node metastasis at the initial diagnosis of the disease (53 patients, 80%) and 13 patients (20%) had retroperitoneal lymph node relapse after initial stage I disease, or after successful first-line chemotherapy for stage II/III disease (metachronous relapse, median time of the relapse: 9 months). The proportions of patients with good, intermediate, and poor IGCCCG prognostic classification were, respectively, 65%, 27%, and 7.5%.
Surgeries and postoperative results
The median size of the largest retroperitoneal mass was 25 mm in great axis; six patients (9.1%) had a retroperitoneal mass of more than 50 mm (Table 1). The location of largest mass was mainly pre or latero aortic (38 patients, 58%).
Median operative time was 200 min [108–248] and estimated blood loss was 50 mL [IQR 50–150] (Table 2). Most patients had a modified template RARPLND (45 patients, 68%). No additional procedures (such as organ resection, or aorta/vena cava resection or reconstruction) were needed.
Regarding intraoperative complications, four patients (6.0%) had a vascular injury (two vena cava, two aorta), only one had an estimated blood loss of more than 500 mL, and no one had blood transfusion. Three patients (4.5%) had a conversion to open surgery: one for active bleeding, and two for difficulty of dissection (one was a post-chemotherapy seminoma, the other one a primary retroperitoneal tumor).
Regarding postoperative complications, seven patients (11%) had a postoperative ileus, five during hospitalization and two after. Five patients (7.6%) had lymphatic complications (symptomatic lymphocele needing paracentesis or drainage, lymphatic flow through trocar orifice); all of these complications occurred after hospitalization. Six patients (9.1%) needed re-hospitalization.
Three patients (3.5%) had a IIIa Clavien–Dindo complication (percutaneous drainage of lymphocele), there was no IIIb or more Clavien–Dindo complications.
In univariable analyses predicting intraoperative and early postoperative complications within 30 days (14 events), blood loss (Odds ratio [OR]: 1.01, 95% confidence interval [95% CI] 1.0–1.01, p = 0.02), lateral intraoperative patient positioning toward the right side (OR: 0.2, 95% CI 0.03–0.7, p = 0.03), and operative time (OR: 1.01, 05% CI 1.0–1.01, p = 0.02) reached independent predictor status. None of the other tested variables, namely age, BMI, time between orchiectomy and lymph node dissection, type of preoperative chemotherapy, number of cycles of chemotherapy, type of lymph node dissection, and histological type reached independent predictor status.
In multivariable analyses (including blood loss, patient positioning, operative time) predicting intraoperative and early postoperative complications within 30 days, no factor reached independent predictor status.
In univariable analyses predicting severe (Clavien–Dindo ≥ IIIa) intraoperative and early postoperative complications within 30 days (3 events), no variable reached independent predictor status.
Pathology and early oncologic outcomes
Median number of lymph nodes in pathological reports was 10 [6–17]. Teratoma, necrosis, and viable tumor was found in 53%, 39%, and 7.6% of the cases, respectively.
With a median follow-up of 16 months, two patients had a relapse: one in the retrocrural space associated with reascending serum tumor markers and equivocal lung nodules months after PC-RARPLND, managed with second-line chemotherapy, with complete response; the other patient had multiple lung metastases 5 months after surgery and died 1 month later.
Discussion
Since there is a gap in the literature for a thorough and updated examination of a large PC-RARPLND series, the purpose of our study was to outline our multicenter experience with PC-RARPLND in terms of perioperative and early oncological outcomes. Our study showed that PC-RARPLND for selected cases was a feasible procedure with acceptable complication rates. In addition, no adverse or unusual oncological events occurred.
In the light of our results, PC-RARPLND should still only be performed by highly experienced robotic surgeons knowing that major vessel injury could occur and need to be managed with efficacy and safety [17]. A 6.0% rate of vessel injury was observed, but only one patient had significant bleeding with the need to an open conversion. This underlines the added value of the robotic procedure in selected cases as it provides important advantages such as short length of stay, low estimated blood loss, and small skin incisions.
The majority of patients had a modified template resection. This proportion is a consequence of a stringent selection of favorable patients for the robotic approach. A full bilaterally retroperitoneal lymph node resection is not mandatory for selected patients as described by Heidenreich et al. [18, 19]. The safety of modified template resection was recently validated by Gerdtsson et al. [20].
Our results are in accordance to the recent and growing data regarding PC-RARPLND, which are all retrospective series. Regarding intraoperative and postoperative outcomes, Fankhauser et al. reported a 3% conversion rate to open surgery, and a blood transfusion rate of 3% in the largest cohort so far reported [14]. Regarding oncological outcomes, recurrence rates ranged from 0 to 16.1% [14, 15, 21, 22].
Several limitations of our study need to be mentioned. First, our study is based on a retrospective analysis with all of its inherent limitations leading to selection and data collection bias. We cannot exclude that some adverse events had been missed, especially small complications resulting in outpatient visits if patients had been re-admitted to other facilities not visible to the surgical team. Second, the template of RARPLND was chosen by each surgeon and varied between patients and centers. Additionally, information regarding antegrade ejaculation was not available and follow-up was only intermediate, as centers only recently started to perform this procedure robotically. Lastly, a comparison to a control group treated with open surgery was not available.
Conclusion
In this multicenter study, we saw that for selected cases and in expert hands, PC-RARPLND seemed to be a feasible and reasonably safe procedure, with no adverse oncological results. Prospective evaluation or ideally a comparative randomized trial versus open surgery should be performed to have more consistent data regarding the safety and oncologic efficacy of this procedure.
Data availability
The data that support the findings of this study are available from the corresponding author, Nicolas Branger, upon reasonable request.
Abbreviations
- GCT:
-
Germ cell tumor
- RLN:
-
Retroperitoneal lymph node
- RPLND:
-
Retroperitoneal lymph node dissection
- RARPLND:
-
Robot-assisted retroperitoneal lymph node dissection
References
Wymer KM, Pearce SM, Harris KT, Pierorazio PM, Daneshmand S, Eggener SE (2017) Adherence to national comprehensive cancer network® guidelines for testicular cancer. J Urol. 197(3):684–9
Honecker F, Aparicio J, Berney D, Beyer J, Bokemeyer C, Cathomas R et al (2018) ESMO Consensus Conference on testicular germ cell cancer: diagnosis, treatment and follow-up. Ann Oncol 29(8):1658–86
Laguna MP, Pizzocaro G, Klepp O, Algaba F, Kisbenedek L, Leiva O (2022) EAU guidelines on testicular cancer. Eur Urol 40(2):102–110
Costello AJ (2020) Considering the role of radical prostatectomy in 21st century prostate cancer care. Nat Rev Urol 17(3):177–188
Touijer K, Jacqmin D, Kavoussi LR, Montorsi F, Patard JJ, Rogers CG et al (2010) The expanding role of partial nephrectomy: a critical analysis of indications, results, and complications. Eur Urol 57(2):214–222
Parekh DJ, Reis IM, Castle EP, Gonzalgo ML, Woods ME, Svatek RS et al (2018) Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): an open-label, randomised, phase 3, non-inferiority trial. Lancet 391(10139):2525–2536
Stephenson AJ, Sheinfeld J (2004) The role of retroperitoneal lymph node dissection in the management of testicular cancer. Importance Lymph Node Dissection Urol Cancers 22(3):225–233
Chalfin HJ, Ludwig W, Pierorazio PM, Allaf ME (2016) Robotic primary RPLND for stage I testicular cancer: a review of indications and outcomes. Curr Urol Rep 17(5):41
Ghandour R, Ashbrook C, Freifeld Y, Singla N, El-Asmar JM, Lotan Y et al (2020) Nationwide patterns of care for stage II nonseminomatous germ cell tumor of the testicle. Eur Urol Oncol 3(2):198–206
Albers P, Siener R, Krege S, Schmelz HU, Dieckmann KP, Heidenreich A et al (2008) Randomized phase III trial comparing retroperitoneal lymph node dissection with one course of bleomycin and etoposide plus cisplatin chemotherapy in the adjuvant treatment of clinical stage I nonseminomatous testicular germ cell tumors: AUO trial AH 01/94 by the German Testicular Cancer Study Group. J Clin Oncol 26(18):2966–2972
Nini A, Boschheidgen M, Hiester A, Winter C, Antoch G, Schimmöller L et al (2022) Preoperative clinical and radiographic predictors of major vascular surgery in patients with testicular cancer undergoing post-chemotherapy residual tumor resection (PC-RPLND). World J Urol 40(2):349–354
Stepanian S, Patel M, Porter J (2016) Robot-assisted laparoscopic retroperitoneal lymph node dissection for testicular cancer: evolution of the technique. Eur Urol 70(4):661–667
Sheinfeld J, Feldman DR, DiNatale RG, Bosl GJ (2019) Altering the natural history of surgical relapse in testicular cancer: suboptimal surgery and pneumoperitoneum. Eur Urol 76(5):612–614
Fankhauser CD, Afferi L, Stroup SP, Rocco NR, Olson K, Bagrodia A et al (2022) Minimally invasive retroperitoneal lymph node dissection for men with testis cancer: a retrospective cohort study of safety and feasibility. World J Urol 40(6):1505–1512
Abdul-Muhsin H, Rocco N, Navaratnam A, Woods M, L’Esperance J, Castle E et al (2021) Outcomes of post-chemotherapy robot-assisted retroperitoneal lymph node dissection in testicular cancer: multi-institutional study. World J Urol 39(10):3833–3838
Lloyd P, Hong A, Furrer MA, Lee EWY, Dev HS, Coret MH et al (2022) A comparative study of peri-operative outcomes for 100 consecutive post-chemotherapy and primary robot-assisted and open retroperitoneal lymph node dissections. World J Urol 40(1):119–126
Reeves F, George N, Challacombe B (2023) Red out: bleeding during robotic retroperitoneal lymph node dissection and strategies to manage it. Eur Urol Open Sci 1(48):84–89
Vallier C, Savoie PH, Delpero JR, Bladou F, Gravis G, Salem N et al (2014) External validation of the Heidenreich criteria for patient selection for unilateral or bilateral retroperitoneal lymph node dissection for post-chemotherapy residual masses of testicular cancer. World J Urol 32(6):1573–1578
Heidenreich A, Pfister D, Witthuhn R, Thüer D, Albers P (2009) Postchemotherapy retroperitoneal lymph node dissection in advanced testicular cancer: radical or modified template resection. Eur Urol 55(1):217–226
Gerdtsson A, Thor A, Grenabo Bergdahl A, Almås B, Håkansson U, Törnblom M et al (2022) Unilateral or bilateral retroperitoneal lymph node dissection in nonseminoma patients with postchemotherapy residual tumour? Results from RETROP, a population-based mapping study by the Swedish Norwegian testicular cancer group. Eur Urol Oncol 5(2):235–243
Li R, Duplisea JJ, Petros FG, González GMN, Tu SM, Karam JA et al (2021) Robotic postchemotherapy retroperitoneal lymph node dissection for testicular cancer. Eur Urol Oncol 4(4):651–658
Ohlmann CH, Saar M, Pierchalla LC, Zangana M, Bonaventura A, Stöckle M et al (2021) Indications, feasibility and outcome of robotic retroperitoneal lymph node dissection for metastatic testicular germ cell tumours. Sci Rep 11(1):10700
Author information
Authors and Affiliations
Consortia
Contributions
NB: protocol/project development, data collection or management, data analysis, manuscript writing/editing; FB: data collection or management/ manuscript writing/editing; GV: data collection or management/ manuscript writing/editing; SK: data analysis/manuscript writing/editing; GR: manuscript writing/editing; JCB: manuscript writing/editing; JBB: manuscript writing/editing; AK: data collection or management; AMDV: data collection or management; AF: manuscript writing/editing; JW: manuscript writing/editing; ASB: data collection or management; ND: manuscript writing/editing; MR: protocol/project development; TM: protocol/project development, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This is a retrospective analysis, no interventional actions were done, only data collection.
Informed consent
Institutional review board approved the study (ROBOTESTIS-IPC-2021–039), waiving the need of an informed consent, considering the retrospective characteristic of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Branger, N., Bladou, F., Verhoest, G. et al. Post-chemotherapy robot-assisted retroperitoneal lymph node dissection for metastatic germ cell tumors: safety and perioperative outcomes. World J Urol 41, 2405–2411 (2023). https://doi.org/10.1007/s00345-023-04536-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04536-3